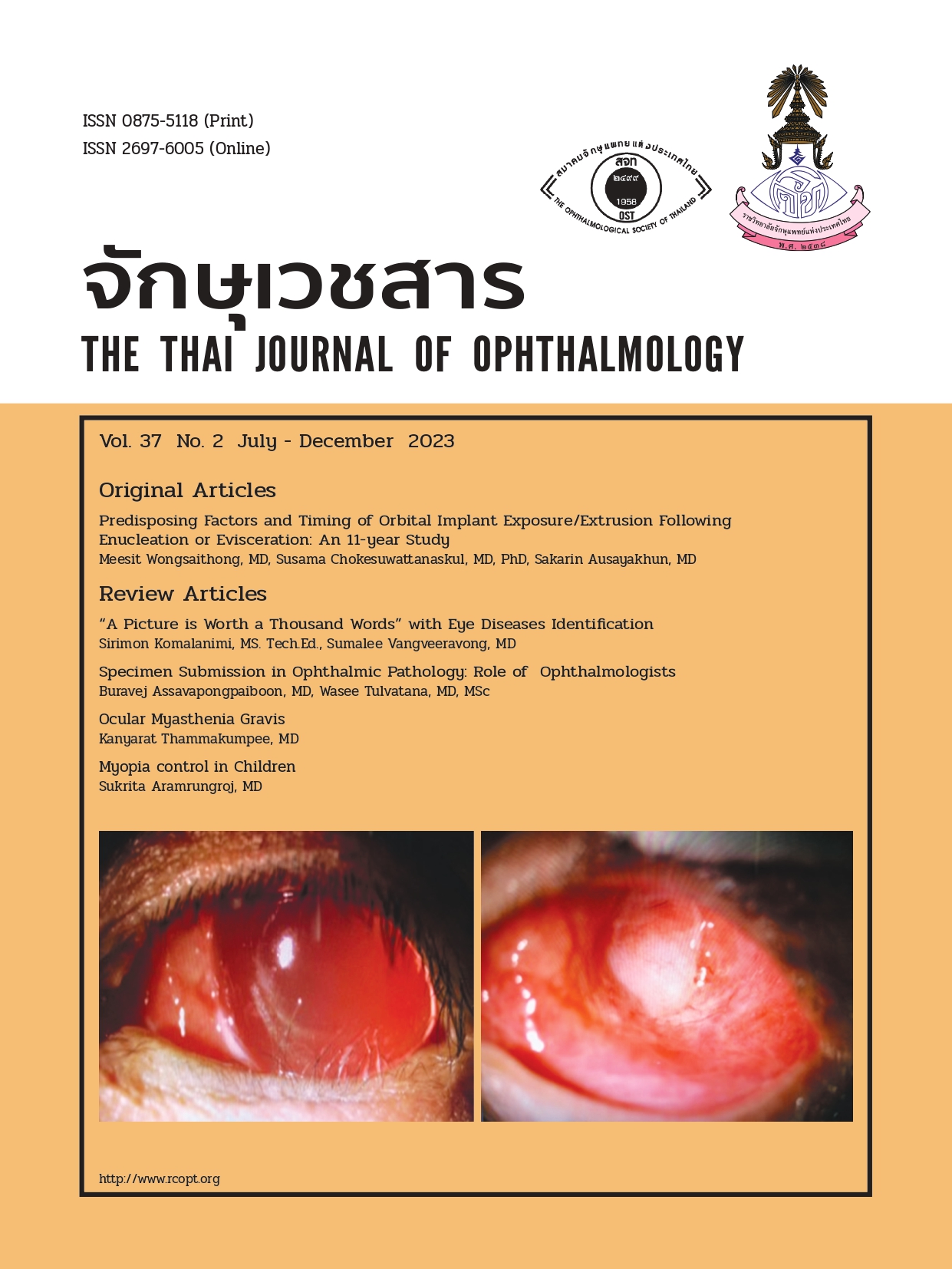
Predisposing Factors and Timing of Orbital Implant Exposure/Extrusion Following Enucleation or Evisceration: An 11-year study
Keywords:
orbital implant extrusion, orbital implant exposure, evisceration, enucleationAbstract
Purpose
Enucleation and evisceration are surgical procedures to remove a diseased eye. An extrusion/exposure of the orbital implants is the most common post-operative orbital implant-related complication. This study aimed to identify the incidence, timing, and possible risk factors of orbital implant exposure/extrusion in patients who underwent enucleation or evisceration.
Methods
The medical records of patients diagnosed with “exposure/extrusion orbital implant” following enucleation or evisceration at Chiang Mai University Hospital between January 2007 and December 2017 were retrospectively reviewed. Multivariable regression analysis was performed to identify the possible predicting factors.
Results
Overall, 466 patients underwent either enucleation (313/466, 67.17%) or evisceration (153/466, 32.83%). Three hundred twelve patients (312/466, 67.16%) were male. The age ranged between 0 and 94 years. The incidence of exposure/extrusion was 12.14% (38/313) in the enucleation group and 17.65% (27/153) in the evisceration group. The most common indication for surgery was ocular infections (218/466, 46.78% patients). Using multivariable regression analysis, older age (p=0.008) and HIV infection (p<0.0001) were significantly associated with the occurrence of exposure/extrusion in patients who underwent enucleation but not the evisceration.
Conclusion
The incidence of extrusion/exposure of the orbital implants following enucleation or evisceration was not uncommon. We identified older age and HIV infection as possible risk factors of orbital implant exposure/extrusion in patients who underwent enucleation. In most cases, the complications occurred within a month following the enucleation (18/38, 47.37% patients) and during 1-12 months following the evisceration (16/27, 59.26% patients), suggesting the appropriate follow-up frequency and period.
References
Al-Farsi HA, Sabt BI, Al-Mujaini AS. Orbital implant exposure following enucleation or evisceration. Oman J Ophthalmol. 2017;10(2):87-90. doi:10.4103/ojo.OJO_156_2016
Ye J, Gao Q, He JJ, et al. Exposure rate of unwrapped hydroxyapatite orbital implants in enucleation surgery. Br J Ophthalmol. 2016;100(6):860-865. doi:10.1136/bjophthalmol-2015-307412
Schellini S, Jorge E, Sousa R, et al. Porous and nonporous orbital implants for treating the anophthalmic socket: A meta-analysis of case series studies. Orbit. 2016;35(2):78-86. doi:10.3109/01676830.2016.1139591
Viswanathan P, Sagoo MS, Olver JM. UK national survey of enucleation, evisceration and orbital implant trends. Br J Ophthalmol. 2007;91(5):616-619. doi:10.1136/bjo.2006.103937
Gradinaru S, Popescu V, Leasu C, et al. Hydroxyapatite ocular implant and non-integrated implants in eviscerated patients. J Med Life. 2015;8(1):90-93.
McElnea EM, Ryan A, Fulcher T. Porous orbital implant exposure: the influence of surgical technique. Orbit. 2014;33(2):104-108. doi:10.3109/01676830.2013.851706
Lin CW, Liao SL. Long-term complications of different porous orbital implants: a 21-year review. Br J Ophthalmol. 2017;101(5):681-685. doi:10.1136/bjophthalmol-2016-308932
Oestreicher JH, Liu E, Berkowitz M. Complications of hydroxyapatite orbital implants. A review of 100 consecutive cases and a comparison of Dexon mesh (polyglycolic acid) with scleral wrapping. Ophthalmology. 1997;104(2):324-329. doi:10.1016/s0161-6420(97)30316-9
Sami D, Young S, Petersen R. Perspective on orbital enucleation implants. Surv Ophthalmol. 2007;52(3):244-265. doi:10.1016/j.survophthal.2007.02.007
Wladis EJ, Aakalu VK, Sobel RK, et al. Orbital Implants in Enucleation Surgery: A Report by the American Academy of Ophthalmology. Ophthalmology. 2018;125(2):311-317. doi:10.1016/j.ophtha.2017.08.006
Yoon JS, Lew H, Kim SJ, et al. Exposure rate of hydroxyapatite orbital implants a 15-year experience of 802 cases. Ophthalmology. 2008;115(3):566-572.e2. doi:10.1016/j.ophtha.2007.06.014
Downloads
Published
Issue
Section
License
Copyright (c) 2024 The THAI Journal of OPHTHALMOLOGY

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Thai Journal of Ophthalmology (TJO) is a peer-reviewed, scientific journal published biannually for the Royal College of Ophthalmologists of Thailand. The objectives of the journal is to provide up to date scientific knowledge in the field of ophthalmology, provide ophthalmologists with continuing education, promote cooperation, and sharing of opinion among readers.
The copyright of the published article belongs to the Thai Journal of Ophthalmology. However the content, ideas and the opinions in the article are from the author(s). The editorial board does not have to agree with the authors’ ideas and opinions.
The authors or readers may contact the editorial board via email at admin@rcopt.org.