Chronic Postsurgical Pain: Review article
Keywords:
Chronic postsurgical pain, Surgical procedure, Multimodal analgesiaAbstract
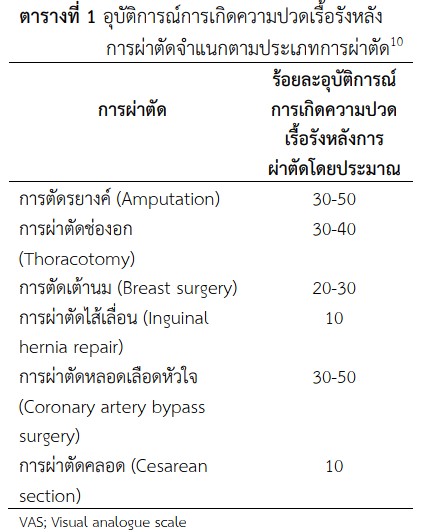
Chronic postsurgical pain is an unpleasant medical condition for both patients and medical team because increased suffering for patients and the workload for medical personnel. Characteristics included neuropathic and inflammatory pain. Surgical procedures with high incidence of chronic postsurgical pain were amputation, thoracotomy, Breast surgery and cardiac surgery. And the risk factor was genetics, psychosocial factors, pain disorders, severity of acute pain, age/gender and type of surgery. Hence, the most controllable factor is severity of acute postoperative pain. Therefore, the effective prevention is less invasive surgical techniques and multimodal analgesia.
Downloads
References
Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet Lond Engl. 2008;372(9633):139-144. https://doi.org/10.1016/S0140-6736(08)60878-8
Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008;101(1):77-86. https://doi.org/10.1093/bja/aen099
Macrae WA, Davies HTO. Chronic postsurgical pain. In: Crombie IK, Croft PR, Linton SJ, LeResche L, Von Korff M, eds. Epidemiology of Pain: A Report of the Task Force on Epidemiology of the International Association for the Study of Pain. IASP Press; 1999:125-142.
Treede R-D, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003-1007. https://doi.org/10.1097/j.pain.0000000000000160
Finnerup NB, Jensen TS. Mechanisms of disease: mechanism-based classification of neuropathic pain-a critical analysis. Nat Clin Pract Neurol. 2006;2(2):107-115. https://doi.org/10.1038/ncpneuro0118
Maguire MF, Latter JA, Mahajan R, Beggs FD, Duffy JP. A study exploring the role of intercostal nerve damage in chronic pain after thoracic surgery. Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg. 2006;29(6):873-879. https://doi.org/10.1016/j.ejcts.2006.03.031
RICHARDSON J, SABANATHAN S, MEARNS AJ, SIDES C, GOULDEN CP. Post-thoracotomy neuralgia. Post-Thoracotomy Neuralgia. 1994;7(2):87-97.
Ivens D, Hoe AL, Podd TJ, Hamilton CR, Taylor I, Royle GT. Assessment of morbidity from complete axillary dissection. Br J Cancer. 1992;66(1):136-138. https://doi.org/10.1038/bjc.1992.230
Fletcher D, Stamer UM, Pogatzki-Zahn E, et al. Chronic postsurgical pain in Europe: An observational study. Eur J Anaesthesiol. 2015;32(10):725-734. https://doi.org/10.1097/EJA.0000000000000319
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. The Lancet. 2006;367(9522):1618-1625. https://doi.org/10.1016/S0140-6736(06)68700-X
Tchivileva IE, Lim PF, Smith SB, et al. Effect of catechol-O-methyltransferase polymorphism on response to propranolol therapy in chronic musculoskeletal pain: A randomized, double–blind, placebo-controlled, crossover pilot study. Pharmacogenet Genomics. 2010;20(4):239-248. https://doi.org/10.1097/FPC.0b013e328337f9ab
Tegeder I, Costigan M, Griffin RS, et al. GTP cyclohydrolase and tetrahydrobiopterin regulate pain sensitivity and persistence. Nat Med. 2006;12(11):1269-1277. https://doi.org/10.1038/nm1490
Vase L, Nikolajsen L, Christensen B, et al. Cognitive-emotional sensitization contributes to wind-up-like pain in phantom limb pain patients. PAIN®. 2011;152(1):157-162. https://doi.org/10.1016/j.pain.2010.10.013
Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122-131. https://doi.org/10.1016/j.amjsurg.2010.02.007
Powell R, Johnston M, Smith WC, et al. Psychological risk factors for chronic post-surgical pain after inguinal hernia repair surgery: a prospective cohort study. Eur J Pain Lond Engl. 2012;16(4):600-610. https://doi.org/10.1016/j.ejpain.2011.08.010
Pinto PR, McIntyre T, Almeida A, Araújo-Soares V. The mediating role of pain catastrophizing in the relationship between presurgical anxiety and acute postsurgical pain after hysterectomy. Pain. 2012;153(1):218-226. https://doi.org/10.1016/j.pain.2011.10.020
Sommer M, de Rijke JM, van Kleef M, et al. Predictors of acute postoperative pain after elective surgery. Clin J Pain. 2010;26(2):87-94. https://doi.org/10.1097/AJP.0b013e3181b43d68
Burgmer M, Pogatzki-Zahn E, Gaubitz M, Wessoleck E, Heuft G, Pfleiderer B. Altered brain activity during pain processing in fibromyalgia. NeuroImage. 2009;44(2):502-508. https://doi.org/10.1016/j.neuroimage.2008.09.008
Peters ML, Sommer M, de Rijke JM, et al. Somatic and Psychologic Predictors of Long-term Unfavorable Outcome After Surgical Intervention. Ann Surg. 2007;245(3):487-494. https://doi.org/10.1097/01.sla.0000245495.79781.65
Wallace MS, Wallace AM, Lee J, Dobke MK. Pain after breast surgery: a survey of 282 women. Pain. 1996;66(2-3):195-205. https://doi.org/10.1016/0304-3959(96)03064-3
Alfieri S, Rotondi F, Di Giorgio A, et al. Influence of Preservation Versus Division of Ilioinguinal, Iliohypogastric, and Genital Nerves During Open Mesh Herniorrhaphy. Ann Surg. 2006;243(4):553-558.
Gray A, Kehlet H, Bonnet F, Rawal N. Predicting postoperative analgesia outcomes: NNT league tables or procedure-specific evidence? Br J Anaesth. 2005;94(6):710-714. https://doi.org/10.1093/bja/aei144
Kraychete DC, Sakata RK, Lannes L de OC, Bandeira ID, Sadatsune EJ. Postoperative persistent chronic pain: what do we know about prevention, risk factors, and treatment. Braz J Anesthesiol Elsevier. 2016;66(5):505-512. https://doi.org/10.1016/j.bjane.2014.12.005
Karanikolas M, Aretha D, Tsolakis I, et al. Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. Anesthesiology. 2011;114(5):1144-1154. https://doi.org/10.1097/ALN.0b013e31820fc7d2
Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth. 2013;111(5):711-720. https://doi.org/10.1093/bja/aet213
Borghi B, D’Addabbo M, White PF, et al. The use of prolonged peripheral neural blockade after lower extremity amputation: the effect on symptoms associated with phantom limb syndrome. Anesth Analg. 2010;111(5):1308-1315. https://doi.org/10.1213/ANE.0b013e3181f4e848
Van de Ven TJ, John Hsia H-L. Causes and prevention of chronic postsurgical pain. Curr Opin Crit Care. 2012;18(4):366-371. https://doi.org/10.1097/MCC.0b013e3283557a7f
Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428-442. https://doi.org/10.1213/ANE.0b013e318249d36e
Panah Khahi M, Yaghooti AA, Marashi SH, Nadjafi A. Effect of pre-emptive gabapentin on postoperative pain following lower extremity orthopaedic surgery under spinal anaesthesia. Singapore Med J. 2011;52(12):879-882.
Laskowski K, Stirling A, McKay WP, Lim HJ. A systematic review of intravenous ketamine for postoperative analgesia. Can J Anaesth J Can Anesth. 2011;58(10):911-923. https://doi.org/10.1007/s12630-011-9560-0
Gurbet A, Basagan-Mogol E, Turker G, Ugun F, Kaya FN, Ozcan B. Intraoperative infusion of dexmedetomidine reduces perioperative analgesic requirements. Can J Anaesth J Can Anesth. 2006;53(7):646-652. https://doi.org/10.1007/BF03021622
McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery: a systematic review of randomized controlled trials. Drugs. 2010;70(9):1149-1163. https://doi.org/10.2165/10898560-000000000-00000
Kaluzny BJ, Kazmierczak K, Laudencka A, Eliks I, Kaluzny JJ. Oral acetaminophen (paracetamol) for additional analgesia in phacoemulsification cataract surgery performed using topical anesthesia Randomized double-masked placebo-controlled trial. J Cataract Refract Surg. 2010;36(3):402-406. https://doi.org/10.1016/j.jcrs.2009.09.035
Bell RF, Kalso EA. Ketamine for pain management. Pain Rep. 2018;3(5). https://doi.org/10.1097/PR9.0000000000000674
White PF, Kehlet H. Improving postoperative pain management: what are the unresolved issues? Anesthesiology. 2010;112(1):220-225. https://doi.org/10.1097/ALN.0b013e3181c6316e
Brookoff D. Chronic pain: 1. A new disease? Hosp Pract 1995. 2000;35(7):45-52, 59. https://doi.org/10.1080/21548331.2000.11444031
Girish PJ. Persistent Postoperative Pain: How Can We Prevent it? In: California Society of Anesthesiologists Annual Meeting and Clinical Anesthesia Update; May 14 – 16, 2010. ; 2010.
Brennan TJ, Kehlet H. Preventive analgesia to reduce wound hyperalgesia and persistent postsurgical pain: not an easy path. Anesthesiology. 2005;103(4):681-683. https://doi.org/10.1097/00000542-200510000-00004
Dauri M, Faria S, Gatti A, Celidonio L, Carpenedo R, Sabato AF. Gabapentin and pregabalin for the acute post-operative pain management. A systematic-narrative review of the recent clinical evidences. Curr Drug Targets. 2009;10(8):716-733. https://doi.org/10.2174/138945009788982513
Downloads
Published
How to Cite
Issue
Section
License
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


