Short-Term Outcomes of Patients Undergoing Transcatheter Aortic Valve Replacement: Early Experience at Chulabhorn Cardiac Center
Keywords:
transcatheter aortic valve replacement (TAVR), transcatheter aortic valve implantation (TAVI), aortic stenosis, bioprosthetic heart valves, echocardiography, hemodynamics, treatment outcomes, complicationsAbstract
Background: Transcatheter aortic valve replacement (TAVR) has emerged as an alternative treatment for severe aortic stenosis in the past few decades. Chulabhorn Cardiac Center initiated a TAVR program in 2019. We herein report the initial 30-day outcomes and complications of the first 60 patients who underwent TAVR in Chulabhorn Cardiac Center.
Methods: This study involved the analysis of descriptive data for the first 60 patients who underwent TAVR from 2019 to 2021. The inclusion criteria were symptomatic severe aortic stenosis or asymptomatic severe aortic stenosis with an indication for valvular intervention according to current standard guidelines. The reported outcomes were retrospectively analyzed, including clinical outcomes, complications, and echocardiographic and hemodynamic changes pre- and post-TAVR.
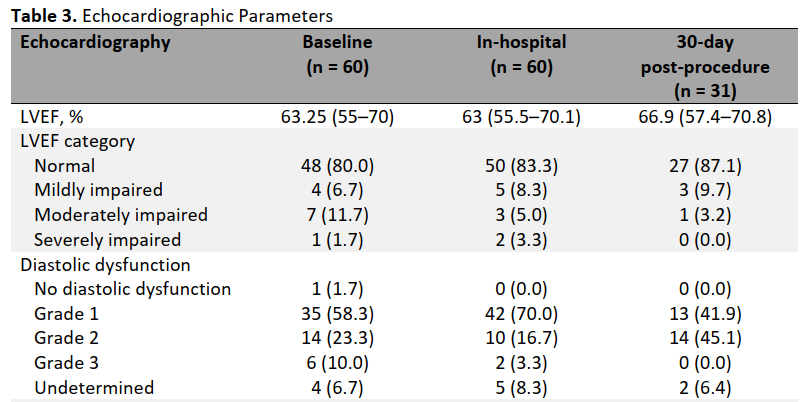
Results: Sixty patients (47% female) were enrolled in this cohort. Their median Society of Thoracic Surgeons score was 3.7. The procedural success rate was 100%. The median in-hospital and 30-day follow-up mean pressure gradient was 9.9 and 11.2 mmHg, respectively, with 46 (93.4%) patients reportedly developing no to mild paravalvular leakage after the procedure. No patients died within the first 30 days after the procedure. With regard to periprocedural complications, 13 (21.7%) patients underwent permanent pacemaker implantation after the TAVR procedure because of new-onset high-grade or complete atrioventricular block. Four (6.6%) patients developed ischemic stroke after the TAVR procedure. Three (5.0%) patients developed a major vascular complication according to the VARC definition, among whom only one (1.7%) patient required surgical correction.
Conclusion: The immediate and 30-day outcomes in our initial 60 patients undergoing TAVR were favorable with a low complication rate.
Downloads
References
d’Arcy JL, Coffey S, Loudon MA, et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study†. Eur Heart J. 2016;37(47):3515-3522. https://doi.org/10.1093/eurheartj/ehw229
Osnabrugge RLJ, Mylotte D, Head SJ, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013;62(11):1002-1012. https://doi.org/10.1016/j.jacc.2013.05.015
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143(5):e72-e227. https://doi.org/10.1161/CIR.0000000000000923
Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739-2791. https://doi.org/10.1093/eurheartj/ehx391
Mack MJ, Leon MB, Smith CR, et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet Lond Engl. 2015;385(9986):2477-2484. https://doi.org/10.1016/S0140-6736(15)60308-7
Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187-2198. https://doi.org/10.1056/NEJMoa1103510
Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597-1607. https://doi.org/10.1056/NEJMoa1008232
Mack MJ, Leon MB, Thourani VH, et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med. 2019;380(18):1695-1705. https://doi.org/10.1056/NEJMoa1814052
Popma JJ, Deeb GM, Yakubov SJ, et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019;380(18):1706-1715. https://doi.org/10.1056/NEJMoa1816885
Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document (VARC-2). Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg. 2012;42(5):S45-60. https://doi.org/10.1093/ejcts/ezs533
Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med. 2016;374(17):1609-1620. https://doi.org/10.1056/NEJMoa1514616
Gilard M, Eltchaninoff H, Iung B, et al. Registry of transcatheter aortic-valve implantation in high-risk patients. N Engl J Med. 2012;366(18):1705-1715. https://doi.org/10.1056/NEJMoa1114705
Downloads
Published
How to Cite
Issue
Section
License
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


