Pathology of Acute Coronary Syndrome, Assessed Using Optical Coherence Tomography
Keywords:
Plaque rupture, Plaque erosion, Calcified nodule, Optical coherence tomography, Acute coronary syndromeAbstract
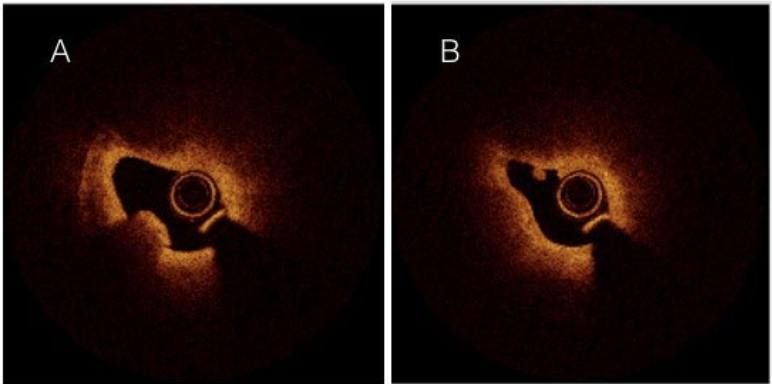
Objectives: We aimed to characterize the pathology of patients with acute coronary syndrome (ACS) using optical coherence tomography (OCT).
Background: OCT is a new, high-resolution intravascular imaging modality that is useful for the assessment of the morphology of ACS lesions.
Methods: We studied 22 patients with ACS using OCT imaging. The pathological features of the disease were classified as plaque rupture, plaque erosion, and calcified nodule.
Results: The incidences of plaque rupture, plaque erosion, and calcified nodule were 73%, 9%, and 9%, respectively. Participants with plaque rupture tended to be younger than those with the other types of lesions (65.7 ± 9.4, 72.0 ± 9.9, and 80.0 ± 8.5 years, respectively; p=0.13). Fibrous plaque tended to be more prevalent than plaque erosion (75%, 100%, and 0%, respectively; p=0.15). The serum creatinine concentration of participants with calcified nodule was higher than that of participants with plaque rupture (1.2 ± 0 vs. 1.0 ± 0.2; p=0.049). The mean minimum luminal diameter (MLD) was highest in participants with calcified nodule and was significantly higher than in participants with plaque rupture (1.5 ± 0.5 vs. 1.0 ± 0.2; p=0.047).
Conclusions: Plaque rupture was the most common lesion, being present in 73% of the patients with ACS, and plaque erosion tended to be associated with the lowest mean luminal area of the three types of lesions. In addition, calcified nodules were common in older patients and were associated with a higher creatinine concentration and MLD than plaque rupture.
Downloads
References
Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47(8 Suppl):C13–C18.
Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From Vulnerable Plaque to Vulnerable Patient: A Call for New Definitions and Risk Assessment Strategies: Part I. Circulation. 2003;108:1664–1672.
Abtahian F, Jang I-K. Optical Coherence Tomography. In Braunwald’s Heart Disease, 10th edition, volume 1. 2015;276–289.
Kubo T, Imanishi T, Takarada S, Kuroi A, Ueno S, Yamano T, et al. Assessment of culprit lesion morphology in acute myocardial infarction: ability of optical coherence tomography compared with intravascular ultrasound and coronary angioscopy. J Am Coll Cardiol. 2007;50:933–939.
Jang I-K, Bouma BE, Kang D-H, Park S-J, Park S-W, Seung K-B, et al. Visualization of coronary atherosclerotic plaques in patients using optical coherence tomography: comparison with intravascular ultrasound. J Am Coll Cardiol. 2002;39:604–609.
Yabushita H, Bouma BE, Houser SL, Aretz HT, Jang I-K, Schlendorf KH, et al. Characterization of Human Atherosclerosis by Optical Coherence Tomography. Circulation. 2002;106:1640–1645.
Jia H, Abtahian F, Aguirre AD, Lee S, Chia S, Lowe H, et al. In Vivo Diagnosis of Plaque Erosion and Calcified Nodule in Patients With Acute Coronary Syndrome by Intravascular Optical Coherence Tomography. J Am Coll Cardiol. 2013;62:1748–1758.
Akasaka T, Kubo T, Mizukoshi M, Tanaka A, Kitabata H, Tanimoto T, et al. Pathophysiology of acute coronary syndrome assessed by optical coherence tomography. J Cardiol. 2010;56:8–14.
van der Wal AC, Becker AE, van der Loos CM, Das PK. Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation. 1994;89:36–44.
Farb A, Burke AP, Tang AL, Liang TY, Mannan P, Smialek J, et al. Coronary plaque erosion without rupture into a lipid core. A frequent cause of coronary thrombosis in sudden coronary death. Circulation. 1996;93:1354–1363.
Hisaki R, Yutani C. Plaque Morphology of Acute Coronary Syndrome. J Atheroscler Thromb. 1998;4:156–161.
Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from Sudden Coronary Death: A Comprehensive Morphological Classification Scheme for Atherosclerotic Lesions. Arterioscler Thromb Vasc Biol. 2000;20:1262–1275.
Burke AP, Farb A, Malcom GT, Liang Y, Smialek J, Virmani R. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation. 1998;97:2110–2116.
Budoff MJ, Rader DJ, Reilly MP, Mohler ER, Lash J, Yang W, et al. Relationship of Estimated GFR and Coronary Artery Calcification in the CRIC (Chronic Renal Insufficiency Cohort) Study. Am J Kid Dis. 2011;58:519–526.
Koukoulaki M, Papachristou E, Kalogeropoulou C, Papathanasiou M, Zampakis P, Vardoulaki M, et al. Increased Prevalence and Severity of Coronary Artery Calcification in Patients with Chronic Kidney Disease Stage III and IV. Nephron Extra. 2012;2:192–204.
Kramer MCA, Rittersma SZH, de Winter RJ, Ladich ER, Fowler DR, Liang Y-H, et al. Relationship of Thrombus Healing to Underlying Plaque Morphology in Sudden Coronary Death. 1J Am Coll Cardiol. 2010;55:122–32.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


