Multidisciplinary Approach for the Management in Spinal Metastases Patients
A Review Article
Keywords:
Spinal metastasis, Vertebral metastasis, Metastatic spine tumor, Spinal tumorAbstract
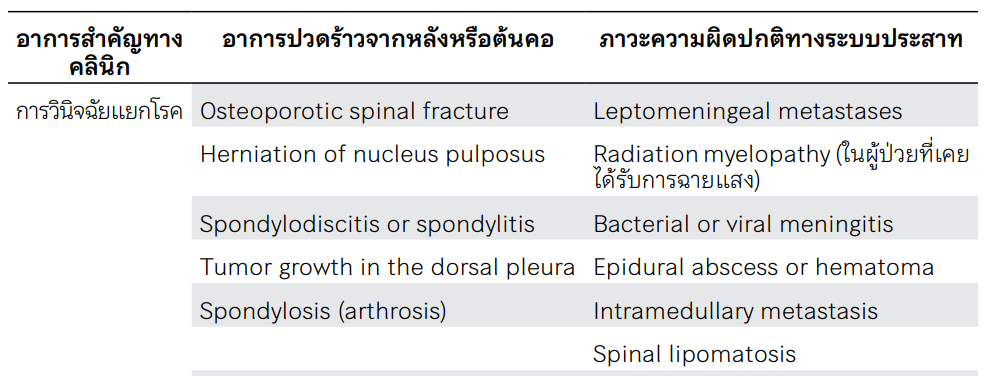
The incidence of spinal metastases is increasing. An early diagnosis contributes to a good result of holistic care and better quality of life for the patients. In Thailand, there are still no standard clinical practice consensus guidelines. Therefore, we would like to review studies relate to spinal metastases. The topic of interest is clinical presentations, diagnosis, imaging investigation, and treatment options (which are conventional and minimally invasive surgery, medication, and radiotherapy). These could be useful and might be developed to use as a general guideline in the future.
Downloads
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7-30.
Weir HK, Thompson TD, Soman A, Moller B, Leadbetter S. The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer. 2015;121(11):1827-1837.
Witham TF, Khavkin YA, Gallia GL, Wolinsky JP, Gokaslan ZL. Surgery insight: current management of epidural spinal cord compression from metastatic spine disease. Nat Clin Pract Neurol. 2006;2(2):87-94; quiz 116.
Loblaw DA, Perry J, Chambers A, Laperriere NJ. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative's Neuro-Oncology Disease Site Group. J Clin Oncol. 2005;23(9):2028-2037.
van der Linden YM, Rolf CA, de Graeff A, Dijkstra PD, Kuijlen JM, Taal W. [Alarm symptoms of spinal metastases in patients with cancer]. Ned Tijdschr Geneeskd. 2015;159:A9256.
Taal W, van der Togt-van Leeuwen AC. [New Dutch guideline on spinal metastasis: extended to include spinal localisations of haematological malignancies]. Ned Tijdschr Geneeskd. 2015;159:A9101.
Helweg-Larsen S, Sorensen PS, Kreiner S. Prognostic factors in metastatic spinal cord compression: a prospective study using multivariate analysis of variables influencing survival and gait function in 153 patients. Int J Radiat Oncol Biol Phys. 2000;46(5):1163-1169.
Boogerd W, van der Sande JJ. Diagnosis and treatment of spinal cord compression in malignant disease. Cancer Treat Rev. 1993;19(2):129-150.
Bollen L, Dijkstra SPD, Bartels R, de Graeff A, Poelma DLH, Brouwer T, et al. Clinical management of spinal metastases-The Dutch national guideline. Eur J Cancer. 2018;104:81-90.
van der Linden YM, Dijkstra SP, Vonk EJ, Marijnen CA, Leer JW, Dutch Bone Metastasis Study Group. Prediction of survival in patients with metastases in the spinal column: results based on a randomized trial of radiotherapy. Cancer. 2005;103(2):320-328.
Buhmann Kirchhoff S, Becker C, Duerr HR, Reiser M, Baur-Melnyk A. Detection of osseous metastases of the spine: comparison of high resolution multi-detector-CT with MRI. Eur J Radiol. 2009;69(3):567-573.
Kim JK, Learch TJ, Colletti PM, Lee JW, Tran SD, Terk MR. Diagnosis of vertebral metastasis, epidural metastasis, and malignant spinal cord compression: are T(1)-weighted sagittal images sufficient? Magn Reson Imaging. 2000;18(7):819-824.
Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13(3):324-8.
Rades D, Douglas S, Huttenlocher S, Rudat V, Veninga T, Stalpers LJ, et al. Validation of a score predicting post-treatment ambulatory status after radiotherapy for metastatic spinal cord compression. Int J Radiat Oncol Biol Phys. 2011;79(5):1503-1506.
Fitzpatrick D, Grabarz D, Wang L, Bezjak A, Fehlings Mg, Fosker C, et al. How effective is a virtual consultation process in facilitating multidisciplinary decision-making for malignant epidural spinal cord compression? Int J Radiat Oncol Biol Phys. 2012;84(2):e167-e172.
Ahmed AK, Goodwin CR, Heravi A, Kim R, Abu-Bonsrah N, Sankey E, et al. Predicting survival for metastatic spine disease: a comparison of nine scoring systems. Spine J. 2018;18(10):1804-1814.
Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010;35(22):E1221-1229.
van der Linden YM, Lok JJ, Steenland E, Martijn H, van Houwelingen H, Marijnen CA, et al. Single fraction radiotherapy is efficacious: a further analysis of the Dutch Bone Metastasis Study controlling for the influence of retreatment. Int J Radiat Oncol Biol Phys. 2004;59(2):528-537.
Falkmer U, Jarhult J, Wersall P, Cavallin-Stahl E. A systematic overview of radiation therapy effects in skeletal metastases. Acta Oncol. 2003;42(5-6):620-633.
Hoskin PJ, Grover A, Bhana R. Metastatic spinal cord compression: radiotherapy outcome and dose fractionation. Radiother Oncol. 2003;68(2):175-180.
Chow E, Harris K, Fan G, Tsao M, Sze WM. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol. 2007;25(11):1423-36.
Chew C, Craig L, Edwards R, Moss J, O'Dwyer PJ. Safety and efficacy of percutaneous vertebroplasty in malignancy: a systematic review. Clin Radiol. 2011;66(1):63-72.
Calmels V, Vallee JN, Rose M, Chiras J. Osteoblastic and mixed spinal metastases: evaluation of the analgesic efficacy of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2007;28(3):570-574.
Dalbayrak S, Onen MR, Yilmaz M, Naderi S. Clinical and radiographic results of balloon kyphoplasty for treatment of vertebral body metastases and multiple myelomas. J Clin Neurosci. 2010;17(2):219-224.
Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine J. 2011;11(9):839-848.
Corcos G, Dbjay J, Mastier C, Leon S, Auperin A, De Baere T, et al. Cement leakage in percutaneous vertebroplasty for spinal metastases: a retrospective evaluation of incidence and risk factors. Spine (Phila Pa 1976). 2014;39(5):E332-E338.
Trathitephun W, Suwanaratana R, Kongthavonskul J, Udomwongsub W. Minimally invasive spinal surgery in spinal metastasis patients: a case series in Chulabhorn Hospital. J Med Assoc Thai. 2021;104(7):79-84.
Jansson KA, Bauer HC. Survival, complications and outcome in 282 patients operated for neurological deficit due to thoracic or lumbar spinal metastases. Eur Spine J. 2006;15(2):196-202.
Bollen L, de Ruiter GC, Pondaag W, Arts MP, Fiocco M, Hazen TJ, et al. Risk factors for survival of 106 surgically treated patients with symptomatic spinal epidural metastases. Eur Spine J. 2013;22(6):1408-1416.
de Ruiter GC, Lobatto DJ, Wolfs JF, Peul WC, Arts MP. Reconstruction with expandable cages after single- and multilevel corpectomies for spinal metastases: a prospective case series of 60 patients. Spine J. 2014;14(9):2085-2093.
Stopeck AT, Lipton A, Body JJ, Steger GG, Tonkin K, de Boer RH, et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol. 2010;28(35):5132-5139.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


