Fluid Balance Calculation Tool for Predicting Postoperative Hematocrit and Intraoperative Blood Loss during Cardiac Surgery
Keywords:
Fluid balance, Predicted Hematocrit, Cardiac Surgery, Cardiopulmonary BypassAbstract
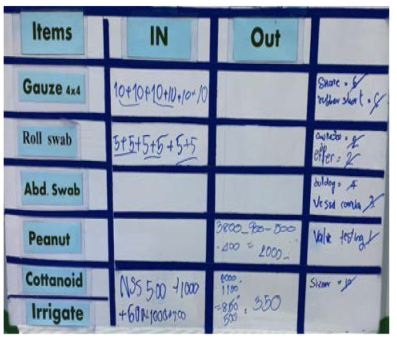
Background and Purpose: Fluid balance management is important in cardiac surgery. During cardiac surgery, patients receive fluid from the anesthesiologist, perfusionist, and surgical field. Greater fluid intake can be obtained from within the surgical field by pumping back through the heart-lung machine. Therefore, it is difficult to calculate the actual fluid balance, which is necessary to predict postoperative hematocrit. Inaccurate calculation of fluid balance can increase the risk of postoperative complications. This study was performed to develop a tool that can calculate the body fluid intake and output of patients undergoing open-heart surgery. The results of the tool can be used to predict postoperative hematocrit and intraoperative blood loss.
Methods: Information technology experts constructed an intake/output chart application, which was used to collect cardiac surgery data at Chulabhorn Hospital during the period from November 2020 to January 2021.
Results: This study included 20 patients (10 men and 10 women; mean age, 68 years). The surgeries consisted of coronary artery bypass graft (CABG) (12 cases, 60%), valve surgery (seven cases, 35%), and combined CABG and valve surgery (one case, 5%). The mean predicted postoperative hematocrit (according to the application) was 33.9%, while the mean actual postoperative hematocrit was 34.06%; these values did not significantly differ (p = 0.064). The mean estimated blood loss during cardiac surgery was 488.40 mL.
Conclusions: Our intake/output chart application can correctly predict postoperative hematocrit and intraoperative blood loss in patients undergoing cardiac surgery
Downloads
References
Bilecen S, de Groot JA, Kalkman CJ, et al. Effect of Fibrinogen Concentrate on Intraoperative Blood Loss Among Patients With Intraoperative Bleeding During High-Risk Cardiac Surgery: A Randomized Clinical Trial. JAMA. 2017;317(7):738-747. https://doi.org/10.1001/jama.2016.21037 PMid:28241354
Monaco F, Nardelli P, Pasin L, et al. Tranexamic acid in open aortic aneurysm surgery: a randomised clinical trial. Br J Anaesth. 2020;124(1):35-43. https://doi.org/10.1016/j.bja.2019.08.028 PMid:31607387
Elassal AA, Al-Ebrahim KE, Debis RS, et al. Re-exploration for bleeding after cardiac surgery: revaluation of urgency and factors promoting low rate. J Cardiothorac Surg. 2021;16(1):166. Published 2021 Jun 7. https://doi.org/10.1186/s13019-021-01545-4 PMid:34099003 PMCid:PMC8183590
Crescini WM, Muralidaran A, Shen I, et al. The use of acute normovolemic hemodilution in paediatric cardiac surgery. Acta Anaesthesiol Scand.2018;62(6):756-764. https://doi.org/10.1111/aas.13095 PMid:29504128
Koc V, Delmas Benito L, de With E, Boerma EC. The Effect of Fluid Overload on Attributable Morbidity after Cardiac Surgery: A Retrospective Study. Crit Care Res Pract. 2020;2020:4836862. Published 2020 Dec 4. https://doi.org/10.1155/2020/4836862 PMid:33489370 PMCid:PMC7787830
Parke RL, Gilder E, Gillham MJ, et al. A Multicenter, Open-Label, Randomized Controlled Trial of a Conservative Fluid Management Strategy Compared With Usual Care in Participants After Cardiac Surgery: The Fluids After Bypass Study. Crit Care Med. 2021; 49(3):449-461. https://doi.org/10.1097/CCM.0000000000004883
Wu B, Sun J, Liu S, et al. Relationship among Mortality of Patients with Acute Kidney Injury after Cardiac Surgery, Fluid Balance and Ultrafiltration of Renal Replacement Therapy: An Observational Study. Blood Purif. 2017;44(1):32-39. https://doi.org/10.1159/000455063 PMid:28237986
Krastiņš J, Pētersons A, Pētersons A. Performance of Fluid Balance as A Marker of Acute Kidney Injury in Children after Open Heart Surgery. Proceedings of the Latvian Academy of Sciences Section B Natural, Exact, and Applied Sciences. 2019;73(2): 125-131. https://doi.org/10.2478/prolas-2019-0020
Mongero L, Stammers A, Tesdahl E,Stasko A, Weinstein S. The effect of ultrafiltration on end-cardiopulmonary bypass hematocrit during cardiac surgery. Perfusion. 2018;33(5) :367-374.
https://doi.org/10.1177/0267659117747046 PMid:29301459
Patel J, Prajapati M, Solanki A, Pandya H. Comparison of Albumin, Hydroxyethyl Starch and Ringer Lactate Solution as Priming Fluid for Cardiopulmonary Bypass in Paediatric Cardiac Surgery. J Clin Diagn Res. 2016;10(6):UC01-UC4 https://doi.org/10.7860/JCDR/2016/18465.7918 PMid:27504382
PMCid:PMC4963742
Vlasov H, Juvonen T, Hiippala S, et al. Effect and safety of 4% albumin in the treatment of cardiac surgery patients: study protocol for the randomized, double-blind, clinical ALBICS (ALBumin In Cardiac Surgery) trial. Trials. 2020;21(1):235. Published 2020 Feb 28. https://doi.org/10.1186/s13063-020-4160-3 PMid:32111230 PMCid:PMC7048052
Cheerranichanunth P, Poolnoi P. Using blood loss pictogram for visual blood loss estimation in cesarean section. J Med Assoc Thai. 2012;95(4):550-556.
Erpicum M, Dardenne N, Hans G, Larbuisson R, Defraigne JO. Prediction of the post-dilution hematocrit during cardiopulmonary bypass. Are new formulas needed?. Perfusion. 2016; 31(6):458-464.
https://doi.org/10.1177/0267659115623357 PMid:26685001
Guevara JH, Zorrilla-Vaca A, Silva-Gordillo GC. The utility of preoperative level of erythrocytosis in the prediction of postoperative blood loss and 30-day mortality in patients with tetralogy of fallot. Ann Card Anaesth. 2017;20(2):188-192. https://doi.org/10.4103/aca.ACA_25_17 PMid:28393779 PMCid:PMC5408524
Bacchetti P, Leung JM. Sample size calculations in clinical research. Anesthesiology. 2002; 97(4):1028-1032. https://doi.org/10.1097/00000542-200210000-00050 PMid:12357184
Cesana BM, Antonelli P. Sample size calculations in clinical research should also be based on ethical principles. Trials. 2016;17(1):149. Published 2016 Mar 18. https://doi.org/10.1186/s13063-016-1277-5 PMid:26993625 PMCid:PMC4797226
Hilberath JN, Thomas ME, Smith T, et al. Blood volume measurement by hemodilution: association with valve disease and reevaluation of the Allen Formula. Perfusion. 2015;30(4):305-311 https://doi.org/10.1177/0267659114547250 PMid:25125291
Willems A, Van Lerberghe C, Gonsette K, et al. The indication for perioperative red blood cell transfusions is a predictive risk factor for severe postoperative morbidity and mortality in children undergoing cardiac surgery. Eur J Cardiothorac Surg. 2014; 45(6):1050-1057. https://doi.org/10.1093/ejcts/ezt548 PMid:24431174
Whitney G, Daves S, Hughes A, et al. Implementation of a transfusion algorithm to reduce blood product utilization in pediatric cardiac surgery. Paediatr Anaesth. 2013; 23(7):639-646. https://doi.org/10.1111/pan.12126 PMid:23506389
Buggeskov KB, Maltesen RG, Rasmussen BS, et al. Lung Protection Strategies during Cardiopulmonary Bypass Affect the Composition of Blood Electrolytes and Metabolites-A Randomized Controlled Trial. J Clin Med. 2018;7(11):462. Published 2018 Nov https://doi.org/10.3390/jcm7110462
PMid:30469433 PMCid:PMC6262287
doi:10.3390/jcm7110462 21. Ranucci M, Ballotta A, La Rovere MT, Castelvecchio S; Surgical and Clinical Outcome Research (SCORE) Group. Postoperative hypoxia and length of intensive care unit stay after cardiac surgery: the underweight paradox?. PLoS One. 2014;9(4):e93992. Published 2014 Apr 7. https://doi.org/10.1371/journal.pone.0093992 PMid:24709952 PMCid:PMC3978074
Sevuk U, Altindag R, Baysal E, et al. The effects of hyperoxaemia on tissue oxygenation in patients with a nadir haematocrit lower than 20% during cardiopulmonary bypass. Perfusion. 2016;31(3):232-239. https://doi.org/10.1177/0267659115595281 PMid:26205807
Ranucci M, Carboni G, Cotza M, et al. Hemodilution on cardiopulmonary bypass as a determinant of early postoperative hyperlactatemia. PLoS One. 2015;10(5): e0126939. Published 2015 May 18. https://doi.org/10.1371/journal.pone.0126939 PMid:25992896 PMCid:PMC4436314
Ranucci M, Carboni G, Cotza M, et al. Hemodilution on cardiopulmonary bypass as a determinant of early postoperative hyperlactatemia. PLoS One. 2015;10(5):e0126939. Published 2015 May 18. https://doi.org/10.1371/journal.pone.0126939 PMid:25992896 PMCid:PMC4436314
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.