Relationships of the duration of working from home with obesity, obesity-related behaviors, physical activity, and stress level in workers in an academic institution during the COVID-19 pandemic
Keywords:
obesity, COVID-19, working from home, physical activity, stress level, workerAbstract
Background: Obesity is caused by an energy imbalance and predisposes toward the development of comorbidities. During the COVID-19 lockdown, behavioral changes may have disrupted energy balance. Previous studies have shown overeating, lower physical activity, and more substantial mental health issues in adults during such a lockdown. However, the relationships of working from home (WFH) with obesity-related parameters, including behaviors, might differ according to individual circumstances. Therefore, in the present study, we aimed to characterize the relationships of WFH during the initial COVID-19 lockdown on the obesity, stress level, physical activity, and obesity-related behaviors in workers at an academic institution in Thailand.
Methods: We evaluated these parameters using an anonymous online questionnaire.
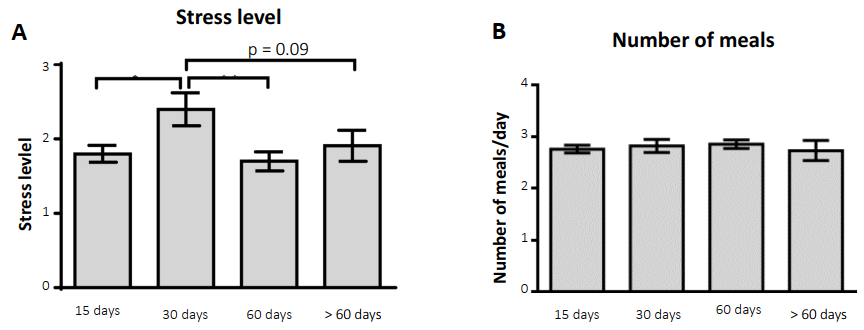
Results: We found that the body weight (p < 0.05) and body mass index (BMI; p < 0.05) of participants who had worked from home were significantly higher after 15 days of the WFH. Similarly, those who had worked from home for 30 days reported that their BMIs had also increased (p < 0.05). The frequency of food delivery was significantly lower in participants who had worked from home for 60 days (p < 0.05) and for >60 days (p < 0.05) than in the 30-day WFH group. In addition, the stress level of the 30-day WFH group was higher than that of the 15-day WFH group (p < 0.05), but lower than that of the 60-day WFH group (p < 0.05).
Conclusions: In conclusion, WFH for a short period of time was associated with increases in body weight and BMI, and changes to obesity-related behaviors. These changes in physical parameters were found to be associated with changes in stress level. These findings may be helpful for the creation of guidelines regarding the preservation of both the physical and mental health of workers during lockdowns. The energy provided by the various sources of nutrition should be assessed in the future because these are important for the bioenergetics and weight gain of workers during such a lockdown.
Downloads
References
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;360:1-8.
Kinlen D, Cody D, O'Shea D. Complications of obesity. QJM. 2018;111(7):437-443. https://doi.org/10.1093/qjmed/hcx152 PMid:29025162
Bendor CD, Bardugo A, Pinhas-Hamiel O, Afek A, Twig G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc Diabetol. 2020;19(1):79. https://doi.org/10.1186/s12933-020-01052-1 PMid:32534575 PMCid:PMC7293793
Misra A. Ethnic-specific criteria for classification of body mass index: a perspective for Asian Indians and American Diabetes Association position statement. Diabetes Technol Ther. 2015;17(9):667-671. https://doi.org/10.1089/dia.2015.0007 PMid:25902357 PMCid:PMC4555479
Pan WH, Yeh WT. How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: an extension of Asian-Pacific recommendations. Asia Pac J Clin Nutr. 2008;17(3):370- 374.
Lim JU, Lee JH, Kim JS, et al. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:2465-2475. https://doi.org/10.2147/COPD.S141295 PMid:28860741 PMCid:PMC5571887
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157-163. https://doi.org/10.1016/S0140-6736(03)15268-3 PMid:14726171
Bassett J, International Diabetes Institute World Health Organization International Association for the Study of Obesity International Obesity TaskForce. The Asia-Pacific Perspective : Redefining Obesity and Its Treatment. Australia: Health Communications Australia; 2000.
Sakboonyarat B, Pornpongsawad C, Sangkool T, et al. Trends, prevalence and associated factors of obesity among adults in a rural community in Thailand: serial cross-sectional surveys, 2012 and 2018. BMC Public Health. 2020;20(1):850. https://doi.org/10.1186/s12889-020-09004-w PMid:32493314 PMCid:PMC7271557
Tchang BG, Saunders KH, Igel LI. Best practices in the management of overweight and obesity. Med Clin North Am. 2021;105(1):149-174. https://doi.org/10.1016/j.mcna.2020.08.018 PMid:33246516
Triukose S, Nitinawarat S, Satian P, et al. Effects of public health interventions on the epidemiological spread during the first wave of the COVID-19 outbreak in Thailand. PLoS One. 2021;16(2):e0246274. https://doi.org/10.1371/journal.pone.0246274 PMid:33606734 PMCid:PMC7894963
Pellegrini M, Ponzo V, Rosato R, et al. Changes in weight and nutritional habits in adults with obesity during the "lockdown" period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7):2016. https://doi.org/10.3390/nu12072016 PMid:32645970 PMCid:PMC7400808
Błaszczyk-Bębenek E, Jagielski P, Bolesławska I, et al. Nutrition behaviors in Polish adults before and during COVID-19 Lockdown. Nutrients.2020;12(10):3084. https://doi.org/10.3390/nu12103084 PMid:33050404 PMCid:PMC7601522
Robinson E, Boyland E, Chisholm A, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156:104853. https://doi.org/10.1016/j.appet.2020.104853 PMid:33038479 PMCid:PMC7540284
Varshney D. How about the psychological pandemic? Perceptions of COVID-19 and work-life of private sector employees-a qualitative study. Psychol Stud (Mysore). 2021;66(3):337-346. https://doi.org/10.1007/s12646-021-00605-y PMid:34334823 PMCid:PMC8316103
Harris MA. The relationship between physical inactivity and mental wellbeing: findings from a gamification-based community-wide physical activity intervention. Health Psychol Open.2018;5(1):2055102917753853. https://doi.org/10.1177/2055102917753853 PMid:29372067 PMCid:PMC5774736
Turna J, Zhang J, Lamberti N, et al. Anxiety, depression and stress during the COVID-19 pandemic: results from a cross-sectional survey. J Psychiatr Res. 2021;137:96-103. https://doi.org/10.1016/j.jpsychires.2021.02.059 PMid:33667763 PMCid:PMC8548032
Marchitelli S, Mazza C, Lenzi A, et al. Weight gain in a sample of patients affected by overweight/obesity with and without a psychiatric diagnosis during the Covid-19 lockdown. Nutrients. 2020;12(11):3525. https://doi.org/10.3390/nu12113525 PMid:33207742 PMCid:PMC7697678
Kwok S, Adam S, Ho JH, et al. Obesity: a critical risk factor in the COVID-19 pandemic. Clin Obes. 2020;10(6):e12403. https://doi.org/10.1111/cob.12403 PMid:32857454 PMCid:PMC7460880
Mohammad S, Aziz R, Al Mahri S, et al. Obesity and COVID-19: what makes obese host so vulnerable? Immun Ageing. 2021;18(1):1. https://doi.org/10.1186/s12979-020-00212-x PMid:33390183 PMCid:PMC7779330
Issue Information-Declaration of Helsinki. J Bone Miner Res. 2019;34(3):BMi-BMii. https://doi.org/10.1002/jbmr.3492
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. https://doi.org/10.2307/2136404 PMid:6668417
Wongpakaran N, Wongpakaran T. The Thai version of the PSS-10: an Investigation of its psychometric properties. Biopsychosoc Med. 2010;4:6. https://doi.org/10.1186/1751-0759-4-6 PMid:20540784 PMCid:PMC2905320
Hill JO, Wyatt HR, Peters JC. The importance of energy balance. Eur Endocrinol. 2013; 9(2):111-115. https://doi.org/10.17925/EE.2013.09.02.111 PMid:29922364 PMCid:PMC6003580
Levine JA. Non-exercise activity thermogenesis (NEAT). Best Pract Res Clin Endocrinol Metab.2002;16(4):679-702. https://doi.org/10.1053/beem.2002.0227 PMid:12468415
Bosy-Westphal A, Eichhorn C, Kutzner D, et al. The age-related decline in resting energy expenditure in humans is due to the loss of fat-free mass and to alterations in its metabolically active components. J Nutr. 2003;133(7):2356-2362. https://doi.org/10.1093/jn/133.7.2356 PMid:12840206
Klausen B, Toubro S, Astrup A. Age and sex effects on energy expenditure. Am J Clin Nutr. 1997;65(4):895-907. https://doi.org/10.1093/ajcn/65.4.895 PMid:9094870
Acheson KJ, Zahorska-Markiewicz B, Pittet P, et al. Caffeine and coffee: their influence on metabolic rate and substrate utilization in normal weight and obese individuals. Am J Clin Nutr. 1980;33(5):989-997. https://doi.org/10.1093/ajcn/33.5.989 PMid:7369170
Wang S, Han Y, Zhao H, et al. Association between coffee consumption, caffeine intake, and metabolic syndrome severity in patients with self-reported rheumatoid arthritis: National Health and Nutrition Examination Survey 2003-2018.Nutrients. 2022;15(1):107. https://doi.org/10.3390/nu15010107 PMid:36615765 PMCid:PMC9824592
Mah E, Chen O, Liska DJ, et al. Dietary supplements for weight management: a narrative review of safety and metabolic health benefits. Nutrients. 2022; 14(9):1787. https://doi.org/10.3390/nu14091787 PMid:35565754 PMCid:PMC9099655
Droit-Volet S, Gil S, Martinelli N, et al. Time and COVID-19 stress in the lockdown situation: Time free, "Dying" of boredom and sadness. PLoS One. 2020;15(8):e0236465. https://doi.org/10.1371/journal.pone.0236465 PMid:32776990 PMCid:PMC7416923
Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res.2020;136:110186. https://doi.org/10.1016/j.jpsychores.2020.110186 PMid:32682159 PMCid:PMC7832650
Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213 PMid:32215365 PMCid:PMC7061893
Zhang SX, Wang Y, Rauch A, et al. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288:112958. https://doi.org/10.1016/j.psychres.2020.112958 PMid:32283450 PMCid:PMC7146665
van der Valk ES, Savas M, van Rossum EFC. Stress and obesity: are there more susceptible individuals? Curr Obes Rep. 2018;7(2):193-203. https://doi.org/10.1007/s13679-018-0306-y PMid:29663153 PMCid:PMC5958156
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.