Angiographic Complications Using a Medium or Small Initial Burr-toArtery Ratio for Rotational Atherectomy
Keywords:
rotational atherectomy, angiographic complication, burr-to-artery ratioAbstract
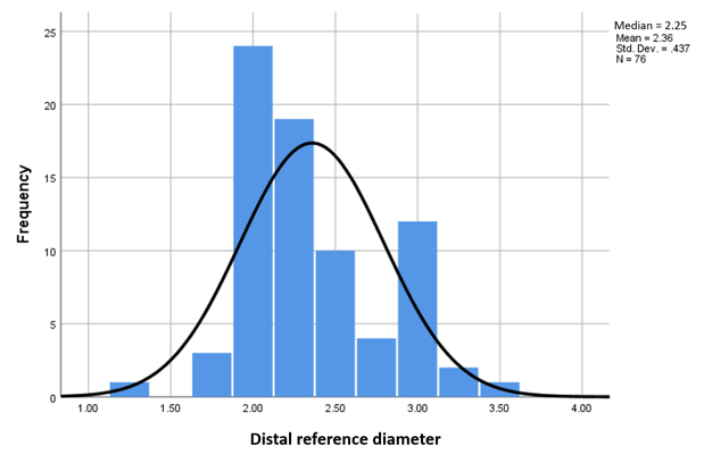
Objectives: In this prospective cohort study, we investigated the safety and efficacy of rotational atherectomy, comparing the use of an initial small with medium burr-to-artery ratio. Background: Rotational atherectomy (RA) is recommended in heavily calcified lesion preparation. Inadequate RA with a burr-to-artery ratio ≤0.6 is associated with increased rate of instent restenosis A burr-to-artery ratio > 0.7 is associated with an increased risk of immediate post-procedural angiographic complications Thus, selection of the initial burr size for RA remains debatable. Methods: We enrolled 73 patients and 76 RA procedures in three tertiary hospitals, with a 6-month follow-up. The primary endpoint was any serious intraprocedure or immediate post-RA angiographic complications occurring during or after the final RA run, including severe dissection, uncorrectable no-reflow phenomenon, coronary perforation, and burr entrapment (Kokeshi phenomenon). Results: We found no significant difference in the rate of serious complications between treatment groups with burr-to-artery ratio ≤0.6 and >0.6 (6.45% vs. 8.89%, p=1.00). Regarding the reason for considering RA, we found a trend of an increased rate of serious complications with unplanned versus planned RA (11.5% vs. 6.0%, p=0.33) or with inadequate lesion preparation (16.7% vs. 5.2%, p=0.14). Conclusions: For coronary lesions requiring RA, the rate of serious angiographic complications did not differ when using an initial burr size with a burr-to-artery ratio of ≤0.6 or >0.6.
Downloads
References
Oktavion YH. PCI in patient with heavy calcified lesion. Management and balloon rupture complication. Folia Medica Indonesiana. 2015;51(4):257–267 21.1
Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions [published correction appears in Circulation. 2012 Feb 28;125(8): e412. Dosage error in article text]. Circulation. 2011;124(23): e574–e651. doi:10.1161/CIR.0b013e318 23ba622
Barbato E, Shlofmitz E, Milkas A, Shlofmitz AR, Azzalini L, Colombo A. State of the art: evolving concepts in the treatment of heavily calcified and undilatable coronary stenoses – from debulking to plaque modification, a 40-year-long journey. EuroIntervention. 2017;13(6): 696–705.
Sharma SK, Duvvuri S, Dangas G, et al. Rotational atherectomy for in-stent restenosis: acute and long-term results of the first 100 cases. J Am Coll Cardiol. 1998;32(5): 1358–1365. doi:10.1016/s0735-1097(98)00382-9
Safian RD, Feldman T, Muller DW, et al. Coronary angioplasty and Rotablator atherectomy trial (CARAT): immediate and late results of a prospective multicenter randomized trial. Catheter Cardiovasc Interv. 2001;53(2):213–220. doi:10.1002/ccd.1151
Barbato E, Carrié D, Dardas P, et al. European expert consensus on rotational atherectomy. EuroIntervention. 2015;11(1):30–36. doi: 10.4244/EIJV11I1A6 J Chulabhorn Royal Acad. 2023; 5(3): 122-132
Tomey MI, Kini AS, Sharma SK. Current status of rotational atherectomy. JACC Cardiovasc Interv. 2014;7(4):345–353. doi:10.1016/j.jcin.2013.12.196
Klein LW. Coronary complications of percutaneous coronary intervention: a practical approach to the management of abrupt closure. Catheter Cardiovasc Interv. 2005;64(3):395–401. doi:10.1002/ccd.20218
Klein LW. Coronary artery perforation during interventional procedures. Catheter Cardiovasc Interv. 2006;68(5):713–717. doi:10.1002/ccd.20855
Barbato E, Carrié D, Dardas P, et al. European expert consensus on rotational atherectomy. EuroIntervention. 2015;11(1): 30–36. doi:10.4244/EIJV11I1A6
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.