Development of a Clinical Nursing Guideline for Preventing and Reducing Increased Intracranial Pressure in Patients with Traumatic Brain Injury: Using Evidence - Based Practice
Keywords:
Traumatic Brain Injury, Increased Intracranial Pressure, Clinical Nursing Practice GuidelineAbstract
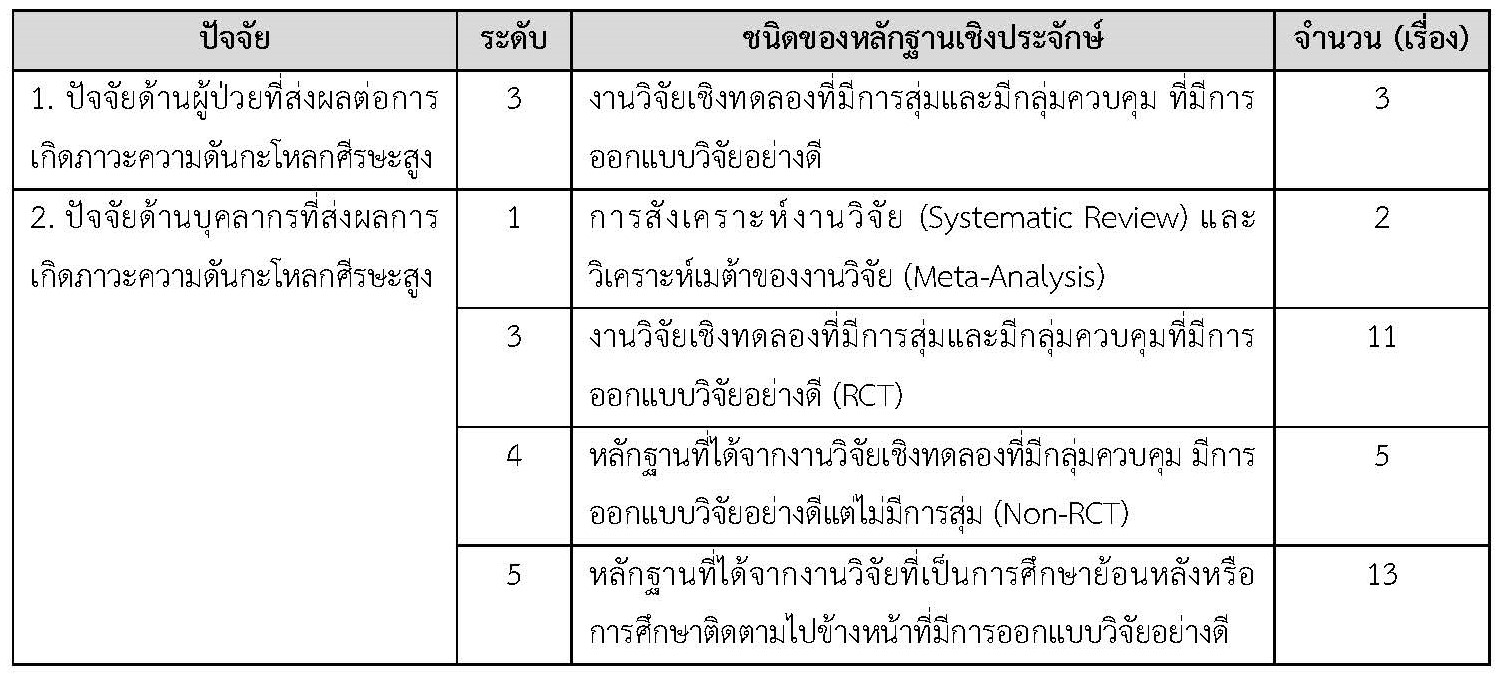
This article aims to propose a clinical nursing guideline for preventing and reducing increased intracranial pressure in patients with traumatic brain injury by using evidence - based practice. The clinical nursing guideline for preventing and reducing increased intracranial pressure in patients with traumatic brain injury consists of eight components: 1) name of the nursing guideline; 2) practice guidelines along with bibliographic references such as assessment and monitoring of intracranial pressure in patients with traumatic brain injury, ensuring effective ventilation, increasing venous return from the brain, managing causes of increased intra-thoracic and intra-abdominal pressure, and monitoring laboratory results that reflect the tendency for increased intracranial pressure in brain injury patients; 3) scope of application of the guideline, including nurses and nursing students, etc; 4) procedures, such as explaining in meetings and presentations to clarify the objectives of using the guideline, etc; 5) recommendations, such as dissemination or implementation, feasibility, and cost-effectiveness; 6) evidence supporting the recommendations, such as assessing the ability to use the guideline and assessing the feasibility of using the guideline; 7) benefits and potential harms from implementing the recommendations from the guideline, such as benefits for brain injury patients, nurses and nursing students, and the organization; and 8) implementing the guideline for practicing nursing skills in clinics. Therefore, using the clinical nursing guideline for preventing and reducing increased intracranial pressure provides guidance for nurses or healthcare personnel, resulting in improved quality of care and better clinical outcomes for brain injury patients.
References
ฉัตรกมล ประจวบลาภ. (2561). ภาวะความดันในกะโหลกศีรษะสูงในผู้ป่วยที่มีพยาธิสภาพที่สมอง: มิติของการพยาบาลตามหลักฐานเชิงประจักษ์. วาสารสภาการพยาบาล, 33(2), 15-28.
นิตยา กออิสรานุภาพ, วรรวิษา สำราญเนตร และวรันณ์ธร โพธารินทร์. (2566). ประสบการณ์การเรียนรู้ของ นักศึกษาพยาบาลจากการฝึกปฏิบัติการพยาบาลผู้ป่วยวิกฤต. วารสารศูนย์อนามัยที่ 9: วารสารส่งเสริม สุขภาพและอนามัยสิ่งแวดล้อม, 17(2), 453-464.
รุ่งนภา เขียวชะอ่ำ. (2556). การปฏิบัติการพยาบาลตามหลักฐานเชิงประจักษ์ (Evidence-Based Nursing).วารสารวิทยาลัยพยาบาลพระปกเกล้า จันทบุรี, 24(2), 94-108.
Altun Uğraş, G., Yüksel, S., Temiz, Z., Eroğlu, S., Şirin, K., & Turan, Y. (2018). Effects of different head-of-bed elevations and body positions on intracranial pressure and cerebral perfusion pressure in neurosurgical patients. The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses, 50(4), 247-251. https://doi.org/10.1097/JNN.0000000000000386
Arbesman, M., Scheer, J., & Lieberman, D. (2008). Using AOTA’s Critically Appraised Topic (CAT) and Critically Appraised Paper (CAP) series to link evidence to practice. OT Practice, 13(5), 18-22.
Bernard, F., Barsan, W., Diaz-Arrastia, R., Merck, L. H., Yeatts, S., & Shutter, L. A. (2022). Brain Oxygen Optimization in Severe Traumatic Brain Injury (BOOST-3): A multicentre, randomised, blinded-endpoint, comparative effectiveness study of brain tissue oxygen and intracranial pressure monitoring versus intracranial pressure alone. BMJ Open, 12(3), e060188. https://doi.org/10.1136/bmjopen-2021-060188
Canac, N., Jalaleddini, K., Thorpe, S. G., Thibeault, C. M., & Hamilton, R. B. (2020). Pathophysiology of intracranial hypertension and noninvasive intracranial pressure monitoring. Fluids and Barriers of The CNS, 17, 1-21. https://doi.org/10.1186/s12987-020 00201-8
Cooper, D. J., et al. (2018). Effect of early sustained prophylactic hypothermia on neurologic outcomes among patients with severe traumatic brain injury: The POLAR randomized clinical trial. The Journal of the American Medical Association, 320(21), 2211-2220. https://doi.org/10.1001/jama.2018.17075
Coverdale, J. P., Katundu, K. G., Sobczak, A. I., Arya, S., Blindauer, C. A., & Stewart, A. J. (2018). Ischemia-modified albumin: Crosstalk between fatty acid and cobalt binding. Prostaglandins, Leukotrienes and Essential Fatty Acids, 135, 147-157. https://doi.org/10.1016/j.plefa.2018.07.014
Craig, J. V., & Smyth, R. L. (2002). The evidence-based practice manual for nurses. Edinburgh, Scotland: Churchill Livingstone.
De Almeida, C. M., Pollo, C. F., & Meneguin, S. (2019). Nursing interventions for patients with intracranial hypertension: Integrative literature review. Aqiochan, 19(4), e1949. https://doi.org/10.5294/aqui.2019.19.4.9
Fargen, K. M., Hoh, B. L., Neal, D., O’connor, T., Rivera-Zengotita, M., & Murad, G. J. (2016). The burden and risk factors of ventriculostomy occlusion in a high-volume cerebrovascular practice: Results of an ongoing prospective database. Journal of Neurosurgery, 124(6), 1805-1812. https://doi.org/10.3171/2015.5.JNS15299
Gemma, M., Tommasino, C., Cerri, M., Giannotti, A., Piazzi, B., & Borghi, T. (2002). Intracranial effects of endotracheal suctioning in the acute phase of head injury. Journal of Neurosurgical Anesthesiology, 14(1), 50-54. https://doi.org/10.1097/00008506-200201000-00010
Griffiths, H. & Gallimore, D. (2005). Positioning critically ill patients in hospital. Nursing Standard, 19(42), 56-64. https://doi.org/10.7748/ns2005.06.19.42.56.c3902
Harrois, A., et al. (2020). Effects of routine position changes and tracheal suctioning on intracranial pressure in traumatic brain injury patients. Journal of Neurotrauma, 37(20), 2227-2233. https://doi.org/10.1089/neu.2019.6873
Hickey, J. V. (2009). The clinical practice of neurological & neurosurgical nursing.6th ed. Wolters Kluwer Health/ Lippincott Williams & Wilkins.
Hickey, J. V. & Strayer, A. L. (2020). The clinical practice of neurological and neurosurgical nursing (8th ed.) China: Philadelphia: Wolters Kluwer.
Maas, A. I. R., et al. (2022). Traumatic brain injury: Progress and challenges in prevention, clinical care, and research. The Lancet Neurology, 21(11), 1004-1060. https://doi.org/10.1016/S1474-4422(22)00309-X
Melnyk, B. M. & Fineout-Overholt, E. (2002). Key steps in implementing evidence-based practice: Asking compelling, searchable questions and searching for the best evidence. Pediatric Nursing, 28(3), 262-266.
Nyholm, L., Steffansson, E., Fröjd, C., & Enblad, P. (2014). Secondary insults related to nursing interventions in neurointensive care: A descriptive pilot study. Journal of Neuroscience Nursing, 46(5), 285-291. https://doi.org/10.1097/JNN.0000000000000077
Pinto, V. L., Tadi, P., & Adeyinka, A. (2023). Increased Intracranial Pressure. In StatPearls. StatPearls Publishing.
Qu, X., et al. (2021). Targeted temperature management at 33 degrees celsius in patients with high-grade aneurysmal subarachnoid hemorrhage: A protocol for a multicenter randomized controlled study. Annals of Translational Medicine, 9(7), 581. https://doi.org/10.21037/atm-20-4719
Radwan, T. A., et al. (2021). Ischemia-modified albumin as a biomarker for prediction of poor outcome in patients with traumatic brain injury: An observational cohort study. Journal of Neurosurgical Anesthesiology, 33(3), 254-257. https://doi.org/10.1097/ANA.0000000000000647
Rienecker, C., Kiprillis, N., Jarden, R., & Connell, C. (2022). Effectiveness of interventions to reduce ventriculostomy-associated infections in adult and paediatric patients with an external ventricular drain: A systematic review. Australian Critical Care, 36(4), 650-668. https://doi.org/10.1016/j.aucc.2022.03.013
Schizodimos, T., Soulountsi, V., Iasonidou, C., & Kapravelos, N. (2020). An overview of management of intracranial hypertension in the intensive care unit. Journal of Anesthesia, 34(5), 741–757. https://doi.org/10.1007/s00540-020-02795-7
Smyth, R. L. (2011). Evidence-based practice manual for nurses-e-book: With pageburst online access. Elsevier Health Sciences.
Szabo, C. M., Grap, M. J., Munro, C. L., Starkweather, A., & Merchant, R. E. (2014). The effect of oral care on intracranial pressure in critically ill adults. Journal of the American Association of Neuroscience Nurses, 46(6), 321-329. https://doi.org/10.1097/JNN.0000000000000092
Tokutomi, T., Morimoto, K., Miyagi, T., Yamaguchi, S., Ishikawa, K., & Shigemori, M. (2003). Optimal temperature for the management of severe traumatic brain injury: Effect of hypothermia on intracranial pressure, systemic and intracranial hemodynamic and metabolism. Neurosurgery, 52(1), 102-112.
The Joanna Briggs Institute. (2000). Best practice: Evidence based practice information sheets for health professionals, Reproducido Del Best Practice, 4(2), 1-6.
Titler, M. G., et al. (2001). The IOWA model of evidence-based practice to promote quality care. Critical Care Nursing Clinics of North America, 13(4), 497-509. https://doi.org/10.1016/S0899-5885(18)30017-0
van den Berghe, G., et al. (2001). Intensive insulin therapy in critically ill patients. The New England Journal of Medicine, 345(19), 1359-1367. https://doi.org/10.1056/NEJMoa011300
Vieira, T. W., Sakamoto, V. T. M., Araujo, B. R., Pai, D. D., Blatt, C. R., & Caregnato, R. C. A. (2022). External ventricular drains: Development and evaluation of a nursing clinical practice guideline. Nursing Reports, 12(4), 933-944. https://doi.org/10.3390/nursrep12040090
Wallace, E., Sharkey, N., & Kerr, E. (2020). Critical care neurology for junior doctors; Four key management strategies. The Ulster Medical Journal, 89(1), 11-13.
Wu, M., et al. (2020). Effects of propofol on intracranial pressure and prognosis in patients with severe brain diseases undergoing endotracheal suctioning. BMC Neurology, 20(1), 394. https://doi.org/10.1186/s12883-020-01972-1
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Nursing and Public Health Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารวิจัยการพยาบาลและการสาธารณสุข ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารวิจัยการพยาบาลและการสาธารณสุข








