Effects of Using Isan Folk Music on the Quality of Sleep in Infants
Keywords:
Infants, Isan Folk Music, Sleep QualityAbstract
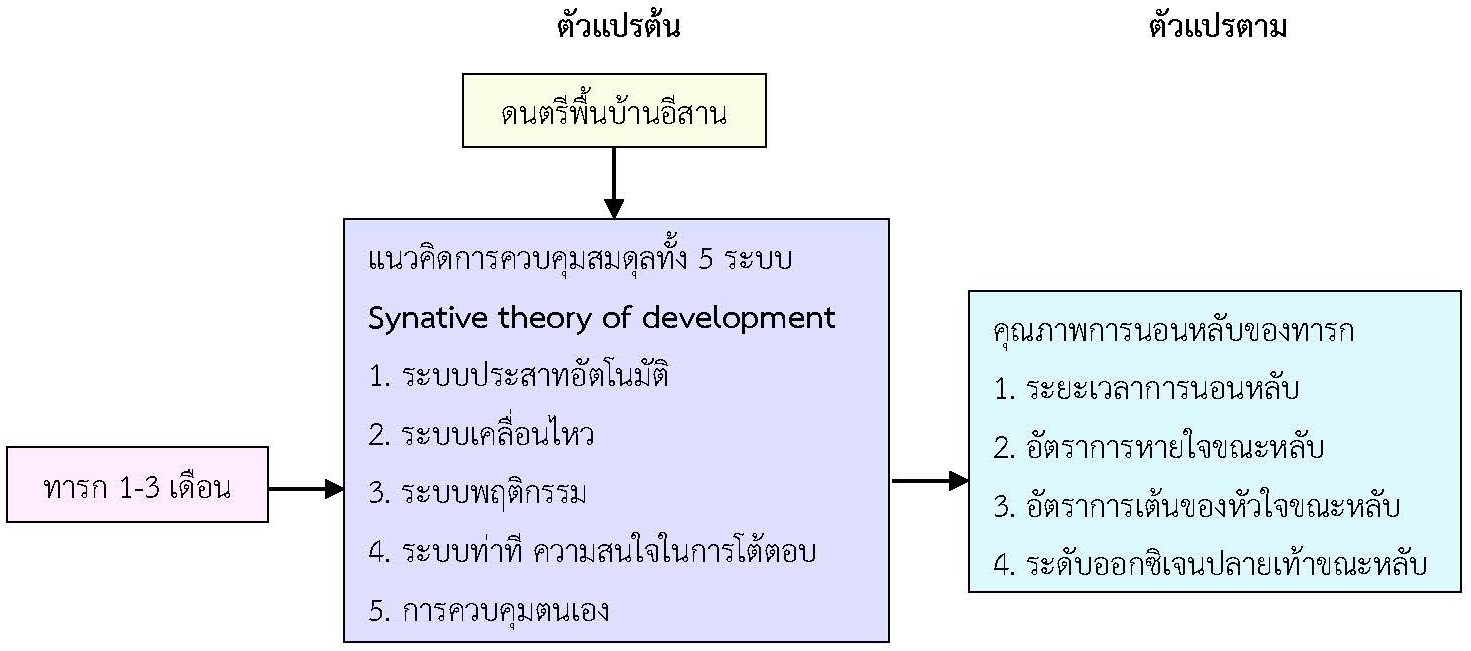
The objective of this quasi-experimental study was to examine the effects of using Isan folk music on the sleep quality of infants. Participants consisted of healthy infants aged between 1-3 months, whose mothers received postpartum check-ups at a community hospital in Nakhon Ratchasima province. A purposive sampling method was used to select 40 participants, divided into a control group of 20 infants who did not receive Isan folk music and an experimental group of 20 infants who were exposed to Isan folk music for 20 minutes per session. The research instruments included Isan folk music, a general information recording form for the mothers and infants, and an infant sleep recording form. The infants' sleep was recorded at home using video between June and August 2023. General data were analyzed using descriptive statistics, and the mean sleep quality outcomes of the experimental and control groups were compared using the Independent t-test and Mann-Whitney U Test.
The research results found that Isan folk music had effects on quality of sleep as follows: 1) the average sleep duration of the experimental group was significantly longer than the control group (p-value < 0.001); 2) the average respiratory rate during sleep of the experimental group was significantly lower than the control group (p-value < 0.01); 3) the average heart rate during sleep of the experimental group did not differ from the control group (p-value = 0.07); and 4) the average peripheral oxygen saturation levels during sleep of the experimental group did not differ from the control group (p-value = 0.40). Therefore, families or caregivers should be encouraged to use Isan folk music to help promote better sleep quality in infants. Moreover, this study provides a basis for further review and development of using Isan folk music to promote sleep quality in infants with colic and sleep problems.
References
ทิพวัลย์ ศรีเฉลิม, ทิพวัลย์ ดารามาศ และศรีสมร ภูมนสกุล. (2554). ผลของดนตรีต่อภาวะหลับตื่นของทาราคลอดก่อนกำหนดในหอผู้ป่วยบำบัดวิกฤตทารกแรกเกิด. รามาธิบดีพยาบาลสาร, 17(2), 178-190.
นันทพร ปรากฏชื่อ, นุจรี ไชยมงคล และยุนี พงศ์จตุรวิทย์. (2554). ผลของการฟังดนตรีไทยบรรเลงต่อพฤติกรรมอารมณ์และระยะเวลาการนอนหลับของทารก. วารสารคณะพยาบาลศาสตร์ มหาวิทยาลัยบูรพา, 19(5), 50-61.
พรพรรณ แก่นอัพรพันธ์. (2564). เส้นทางสู่ดนตรีบำบัดในประเทศไทย. ขอนแก่น: คณะศิลปกรรมศาสตร์ มหาวิทยาลัยขอนแก่น.
พรรณพิไล ศรีอาภรณ์, นุชนาต สุนทรลิ้มศิริ, กนกพร จันทราทิตย์, จิราวรรณ ดีเหลือ, จิราภรณ์ นันท์ชัย และพฤกษลดา เขียวคำ. (2558). ปัจจัยที่เกี่ยวข้องกับภาวะซึมเศร้าหลังคลอดของมารดาและบิดาที่มีบุตรคนแรก. พยาบาลสาร, 42(3), 37-50.
สิริลักษณ์ ศรีเศวต, ทิพวัลย์ ดารามาศ และเรณู พุกบุญมี. (2556). ผลของเสียงเพลงโมสาร์ทต่ออัตราการเต้นของหัวใจ อัตราการหายใจ ค่าความอิ่มตัวของออกซิเจนในเลือด และระยะเวลาการนอนหลับในทารกเกิดก่อนกำหนด. รามาธิบดีพยาบาลสาร, 19(2), 221-234.
อัญชลี ชุ่มบัวทอง, จันทนา ยิ้มน้อย และชษาพิมพ์ สัมมา. (2560). ดนตรีบำบัด. วารสารวิทยาศาสตร์และเทคโนโลยีหัวเฉียวเฉลิมพระเกียรติ, 3(2), 77-87.
อัศลี แสงอารี. (2554). คุณภาพการนอนหลับและการจัดการของผู้ดูแลในการส่งเสริมการนอนหลับของทารกคลอดก่อนกำหนด. วิทยานิพนธ์ปริญญาพยาบาลศาสตรมหาบัณฑิต บัณฑิตวิยาลัยมหาวิทยาลัยสงขลานครินทร์.
Akiyama, et al., (2021). The effect of music and white noise on electroencephalographic (EEG) functional connectivity in neonates in the neonatal intensive care unit. Journal of Child Neurology, 36(1), 38-47. https://doi.org/10.1177/0883073820947894
Als, H. (1986). A Synactive model of neonatal behavioral organization: Framework for the assessment of neurobehavioral development in the premature infant and for support of infants and parents in the neonatal intensive care environment. Physical & Occupational Therapy in Pediatrics, 6(3), 3-53). https://doi.org/10.1300/j006v06n03_02
Altimier, L. & Phillips, R. (2016). The Neonatal Integrative Developmental Care Model: Advanced clinical applications of the seven core measures for neuroprotective family-centered developmental care. Newborn and Infant Nursing Reviews, 16(4), 230-244. https://doi.org/10.1053/j.nainr.2016.09.030
Anzak, S., Sultana, A., & Zulfiqar, S. (2019). Folk traditions of lullabies: Functional analysis. Global Sociological Review, IV, 10-17. https://doi.org/10.31703/gsr.2019(iv-i).02
Camerota, M., Propper, C., B., & Teti, D., M. (2019). Intrinsic and extrinsic factors predicting infant sleep: Moving beyond main effects. Developmental Review, 53, 100871. https://doi.org/10.1016/j.dr.2019.100871
Caparros-Gonzalez, R. A., de la Torre-Luque, A., Diaz-Piedra, C., Vico, F. J., & Buela-Casal, G. (2018). Listening to relaxing music improves physiological responses in premature infants: A randomized controlled trial. Advances in Neonatal Care: Official Journal of the National Association of Neonatal Nurses, 18(1), 58-69. https://doi.org/10.1097/ANC.0000000000000448
Chaput, J. P., et al. (2017). Systematic review of the relationships between sleep duration and health indicators in the early years (0-4 years). BMC Public Health, 17(Suppl 5), 855. https://doi.org/10.1186/s12889-017-4850-2
Dickson, G., & Schubert, E. (2019). How does music aid sleep? Literature review. Sleep Medicine, 63, 142-150. https://doi.org/10.1016/j.sleep.2019.05.016
Hiscock, H., & Davey, M. J. (2018). Sleep disorders in infants and children. Journal of Paediatrics and Child Health, 54(9), 941-944. https://doi.org/10.1111/jpc.12033
Hong, H., Maloney, M. A., Keens, T. G., & Perez, I. A. (2018). Sleep in infants. American Journal of Respiratory and Critical Care Medicine, 198(8), 15-16. https://doi.org/10.1164/rccm.1988P15
Hoogen, A., Teunis, C., Shellhaas, R., Pillen, S., Benders, M., & Dudink, J. (2017). How to improve sleep in a neonatal intensive care unit: A systematic review. Early Human Development, 113, 78-86. https://doi.org/10.1016/j.earlhumdev.2017.07.002
Kondi, B. (2019). LULLABY. The SAGE International Encyclopedia of Music and Culture. Retrieved August 23, 2022 from https://www.researchgate.net/publication/330450233_LULLABY.
Malltese, A., et al. (2017). The synactive theory of development: The keyword for neurodevelopmental disorders. [JD]. Acta Medica Mediterranea, 2S/2017, 1257-1263. https://doi.org/10.19193/0393-6384_2017_2s_194
Mindell, J. A., Leichman, E. S., Composto, J., Lee, C., Bhullar, B., & Walters, R. M. (2016). Development of infant and toddler sleep patterns: Real-world data from a mobile application. Journal of Sleep Research, 25(5), 508-516. https://doi.org/10.1111/jsr.12414
Nurhusna, Ekawaty, F., & Sulistiawan, A. (2020). The effect of murottal alquran therapy on heart rate, respiration rate, saturation oxygen of premature infants using mechanical ventilation in the neonatal intensive care unit. Presented at the 2nd Sriwijaya International Conference of Public Health (SICPH 2019), Atlantis Press, 25, 353-361. https://doi.org/10.2991/ahsr.k.200612.049
Shafiei, E., Ameri, Z., Sheikhbardsiri, H., Yaseri, M., & Baniasadi, H. (2020). The effect of mother’s lullaby on preterm infants’ physiological parameters. The Journal of Pediatric Research, 7(1), 46-51. https://doi.org/10.4274/jpr.galenos.2019.88942
Shimko A. N. (2019). Sleep in infancy: A concept analysis. Journal of Pediatric Nursing, 47, 100-105. https://doi.org/10.1016/j.pedn.2019.05.001
Standford Medicine Children’s Health. (2021). What are an infant's sleep needs?. Retrieved August 23, 2022 from https://www.stanfordchildrens.org/en/topic/default?id=infant-sleep-90-P02237#:~:text=Generally%2C%20newborns%20sleep%20about%208,weigh% 2012%20to%2013%20pounds.
Standley J. M. (2002). A meta-analysis of the efficacy of music therapy for premature infants. Journal of Pediatric Nursing, 17(2), 107-113. https://doi.org/10.1053/jpdn.2002.124128
Tham, E. K., Schneider, N., & Broekman, B. F. (2017). Infant sleep and its relation with cognition and growth: a narrative review. Nature and science of sleep, 9, 135-149. https://doi.org/10.2147/NSS.S125992
van der Heijden, M. J., Oliai Araghi, S., Jeekel, J., Reiss, I. K., Hunink, M. G., & van Dijk, M. (2016). Do hospitalized premature infants benefit from music interventions? A systematic review of randomized controlled trials. PloS One, 11(9), e0161848. https://doi.org/10.1371/journal.pone.0161848
Yue, W., Han, X., Luo, J., Zeng, Z., & Yang, M. (2021). Effect of music therapy on preterm infants in neonatal intensive care unit: Systematic review and meta-analysis of randomized controlled trials. Journal of Advanced Nursing, 77(2), 635-652. https://doi.org/10.1111/jan.14630
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Nursing and Public Health Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารวิจัยการพยาบาลและการสาธารณสุข ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารวิจัยการพยาบาลและการสาธารณสุข








