Update on Demodex Blepharitis
Keywords:
Demodex blepharitis, cylindrical dandruff, tea tree oilAbstract
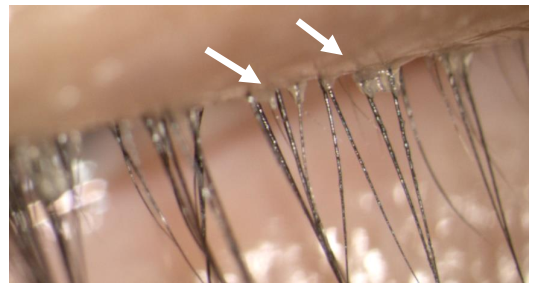
Although Demodex mites are commonly found on normal human eyelids, these mites can cause anterior and posterior blepharitis. Underdiagnosis and undertreatment often occur because the symptoms of Demodex blepharitis considerably overlap with those of other anterior segment disorders. The presence of cylindrical dandruff around the base of the eyelashes and microscopic observation of the mites may support definitive diagnosis. Various treatments have been attempted, but specific eyelid cleansers with long-term eyelid scrubs are generally necessary to control Demodex infestation, improve clinical signs, and ameliorate patient symptoms. This article summarizes the pathogenesis, risk factors, clinical manifestations, diagnostic criteria, and clinical management of Demodex blepharitis.
Downloads
References
Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505-510. https://doi.org/10.1097/ACI.0b013e32833df9f4
Gao Y-Y, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089-3094. https://doi.org/10.1167/iovs.05-0275
Nicholls SG, Oakley CL, Tan A, Vote BJ. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303-312. https://doi.org/10.1007/s10792-016-0249-9
Forton F, Germaux M-A, Brasseur T, et al. Demodicosis and rosacea: epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005;52(1):74-87. https://doi.org/10.1016/j.jaad.2004.05.034
Salem DA-B, El-Shazly A, Nabih N, El-Bayoumy Y, Saleh S. Evaluation of the efficacy of oral ivermectin in comparison with ivermectin-metronidazole combined therapy in the treatment of ocular and skin lesions of Demodex folliculorum. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2013;17(5):e343-347. https://doi.org/10.1016/j.ijid.2012.11.022
Luo X, Li J, Chen C, Tseng S, Liang L. Ocular Demodicosis as a Potential Cause of Ocular Surface Inflammation. Cornea. 2017;36 Suppl 1:S9-S14. https://doi.org/10.1097/ICO.0000000000001361
Gao Y-Y, Di Pascuale MA, Elizondo A, Tseng SCG. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea. 2007;26(2):136-143. https://doi.org/10.1097/01.ico.0000244870.62384.79
English FP, Cohn D, Groeneveld ER. Demodectic mites and chalazion. Am J Ophthalmol. 1985;100(3):482-483. https://doi.org/10.1016/0002-9394(85)90522-7
Liang L, Ding X, Tseng SCG. High prevalence of demodex brevis infestation in chalazia. Am J Ophthalmol. 2014;157(2):342-348.e1. https://doi.org/10.1016/j.ajo.2013.09.031
English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91(3):362-372. https://doi.org/10.1016/0002-9394(81)90291-9
Yam JCS, Tang BSF, Chan T-M, Cheng ACK. Ocular demodicidosis as a risk factor of adult recurrent chalazion. Eur J Ophthalmol. 2014;24(2):159-163. https://doi.org/10.5301/ejo.5000341
Bevins CL, Liu F-T. Rosacea: skin innate immunity gone awry? Nat Med. 2007;13(8):904-906. https://doi.org/10.1038/nm0807-904
Wilkin JK. Oral thermal-induced flushing in erythematotelangiectatic rosacea. J Invest Dermatol. 1981;76(1):15-18. https://doi.org/10.1111/1523-1747.ep12524458
Bernstein JE. Rosacea flushing. Int J Dermatol. 1982;21(1):24. https://doi.org/10.1111/j.1365-4362.1982.tb00483.x
Kulac M, Ciftci IH, Karaca S, Cetinkaya Z. Clinical importance of Demodex folliculorum in patients receiving phototherapy. Int J Dermatol. 2008;47(1):72-77. https://doi.org/10.1111/j.1365-4632.2007.03336.x
Li J, O’Reilly N, Sheha H, et al. Correlation between Ocular Demodex Infestation and Serum Immunoreactivity to Bacillus Proteins in Patients with Facial Rosacea. Ophthalmology. 2010;117(5):870-877.e1. https://doi.org/10.1016/j.ophtha.2009.09.057
Liang L, Safran S, Gao Y, Sheha H, Raju VK, Tseng SCG. Ocular demodicosis as a potential cause of pediatric blepharoconjunctivitis. Cornea. 2010;29(12):1386-1391. https://doi.org/10.1097/ICO.0b013e3181e2eac5
Kheirkhah A, Casas V, Li W, Raju VK, Tseng SCG. Corneal manifestations of ocular demodex infestation. Am J Ophthalmol. 2007;143(5):743-749. https://doi.org/10.1016/j.ajo.2007.01.054
Hom MM, Mastrota KM, Schachter S. Demodex: Clinical Cases and Diagnostic Protocol. Optom Vis Sci. 2013;90(7):e198-e205.
Kheirkhah A, Blanco G, Casas V, Tseng SCG. Fluorescein dye improves microscopic evaluation and counting of demodex in blepharitis with cylindrical dandruff. Cornea. 2007;26(6):697-700. https://doi.org/10.1097/ICO.0b013e31805b7eaf
Gao Y-Y, Di Pascuale MA, Li W, et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol. 2005;89(11):1468-1473. https://doi.org/10.1136/bjo.2005.072363
Norn MS. Demodex folliculorum. Incidence and possible pathogenic role in the human eyelid. Acta Ophthalmol Suppl. 1970;108:7-85.
Mills C, Cleary BJ, Gilmer JF, Walsh JJ. Inhibition of acetylcholinesterase by Tea Tree oil. J Pharm Pharmacol. 2004;56(3):375-379. https://doi.org/10.1211/0022357022773
Tighe S, Gao Y-Y, Tseng SCG. Terpinen-4-ol is the Most Active Ingredient of Tea Tree Oil to Kill Demodex Mites. Transl Vis Sci Technol. 2013;2(7). https://doi.org/10.1167/tvst.2.7.2
Leibowitz HM, Capino D. Treatment of chronic blepharitis. Arch Ophthalmol Chic Ill 1960. 1988;106(6):720. https://doi.org/10.1001/archopht.1988.01060130790006
Navel V, Mulliez A, Benoist d’Azy C, et al. Efficacy of treatments for Demodex blepharitis: A systematic review and meta-analysis. Ocul Surf. 2019;17(4):655-669. https://doi.org/10.1016/j.jtos.2019.06.004
Fulk GW, Murphy B, Robins MD. Pilocarpine gel for the treatment of demodicosis--a case series. Optom Vis Sci Off Publ Am Acad Optom. 1996;73(12):742-745. https://doi.org/10.1097/00006324-199612000-00004
Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular Surface Discomfort and Demodex: Effect of Tea Tree Oil Eyelid Scrub in Demodex Blepharitis. J Korean Med Sci. 2012;27(12):1574-1579. https://doi.org/10.3346/jkms.2012.27.12.1574
Filho PAN, Hazarbassanov RM, Grisolia ABD, Pazos HB, Kaiserman I, Gomes JÁP. The efficacy of oral ivermectin for the treatment of chronic blepharitis in patients tested positive for Demodex spp. Br J Ophthalmol. 2011;95(6):893-895. https://doi.org/10.1136/bjo.2010.201194
Schachter OS. A different approach to treating demodex blepharitis. optometrytimes.com. Published 2014. https://www.optometrytimes.com/view/different-approach-treating-demodex-blepharitis
Ngo W, Jones L, Bitton E. Short-Term Comfort Responses Associated With the Use of Eyelid Cleansing Products to Manage Demodex folliculorum. Eye Contact Lens. 2018;44 Suppl 2:S87-S92. https://doi.org/10.1097/ICL.0000000000000415
Murphy O, O’Dwyer V, Lloyd-McKernan A. The efficacy of tea tree face wash, 1, 2-Octanediol and microblepharoexfoliation in treating Demodex folliculorum blepharitis. Contact Lens Anterior Eye J Br Contact Lens Assoc. 2018;41(1):77-82. https://doi.org/10.1016/j.clae.2017.10.012
Downloads
Published
How to Cite
Issue
Section
License
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


