Fibroblast activation protein inhibitor (FAPI) PET/CT and PET/MRI: novel tracer for molecular imaging in oncology
Keywords:
Fibroblast activation protein inhibitor, molecular imaging, oncology, PET/CT, PET/MRIAbstract
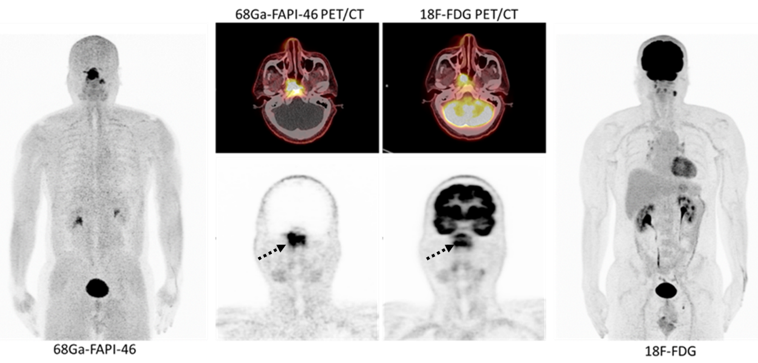
Fibroblast activation protein (FAP) is a type II membrane-bound glycoprotein that is overexpressed on cancer associated fibroblasts (CAFs), which plays a major role in all stages of cancer cells, including carcinogenesis, tumor growth, and metastasis. FAP is not normally found in normal adult tissues. On the other hand, high expression of this glycoprotein is found in wound healing process, chronic inflammation, arthritis, fibrosis, carcinoma, and sarcoma. Radiopharmaceutical specific to FAP, fibroblast activating protein inhibitor (FAPI), was initiated and developed by labeled with the 68Ga isotope and imaging with PET/CT. From the previous study using FPI PET/CT in patients with various types of cancer, 68Ga-FAPI has a high sensitivity for detection of primary tumors and metastases, which could change the course of treatment and provide additional information from the 18F-FDG PET/CT. FAPI tracer is also being developed further for use in diagnosis and treatment (theranostic).
Downloads
References
Pomper M, VanBrocklin H, Anderson C. What is molecular imaging? J Nucl Med. 2008;49(supplement 1):163P.
Kircher MF, Hricak H, Larson SM. Molecular imaging for personalized cancer care. Mol Oncol. 2012;6(2):182-195. https://doi.org/10.1016/j.molonc.2012.02.005
Weissleder R, Pittet MJ. Imaging in the era of molecular oncology. Nature. 2008;452(7187):580-589. https://doi.org/10.1038/nature06917
Brennen WN, Isaacs JT, Denmeade SR. Rationale behind targeting fibroblast activation protein-expressing carcinoma-associated fibroblasts as a novel chemotherapeutic strategy. Mol Cancer Ther. 2012;11(2):257-266. https://doi.org/10.1158/1535-7163.MCT-11-0340
Franco OE, Shaw AK, Strand DW, Hayward SW. Cancer associated fibroblasts in cancer pathogenesis. Semin Cell Dev Biol. 2010;21(1):33-39. https://doi.org/10.1016/j.semcdb.2009.10.010
Kratochwil C, Flechsig P, Lindner T, et al. 68Ga-FAPI PET/CT: Tracer Uptake in 28 Different Kinds of Cancer. J Nucl Med. 2019;60(6):801-805. https://doi.org/10.2967/jnumed.119.227967
Meyer C, Dahlbom M, Lindner T, et al. Radiation Dosimetry and Biodistribution of 68Ga-FAPI-46 PET Imaging in Cancer Patients. J Nucl Med Off Publ Soc Nucl Med. 2020;61(8):1171-1177. https://doi.org/10.2967/jnumed.119.236786
Chen H, Pang Y, Wu J, et al. Comparison of [68Ga]Ga-DOTA-FAPI-04 and [18F] FDG PET/CT for the diagnosis of primary and metastatic lesions in patients with various types of cancer. Eur J Nucl Med Mol Imaging. 2020;47(8):1820-1832. https://doi.org/10.1007/s00259-020-04769-z
Chen H, Zhao L, Ruan D, et al. Usefulness of [68Ga]Ga-DOTA-FAPI-04 PET/CT in patients presenting with inconclusive [18F]FDG PET/CT findings. Eur J Nucl Med Mol Imaging. 2021;48(1):73-86. https://doi.org/10.1007/s00259-020-04940-6
Koerber SA, Staudinger F, Kratochwil C, et al. The Role of 68Ga-FAPI PET/CT for Patients with Malignancies of the Lower Gastrointestinal Tract: First Clinical Experience. J Nucl Med Off Publ Soc Nucl Med. 2020;61(9):1331-1336. https://doi.org/10.2967/jnumed.119.237016
Alterio D, Marvaso G, Ferrari A, Volpe S, Orecchia R, Jereczek-Fossa BA. Modern radiotherapy for head and neck cancer. Semin Oncol. 2019;46(3):233-245. https://doi.org/10.1053/j.seminoncol.2019.07.002
Castaldi P, Leccisotti L, Bussu F, Miccichè F, Rufini V. Role of (18)F-FDG PET-CT in head and neck squamous cell carcinoma. Acta Otorhinolaryngol Ital Organo Uff Della Soc Ital Otorinolaringol E Chir Cerv-facc. 2013;33(1):1-8.
Hentschel M, Appold S, Schreiber A, et al. Serial FDG-PET on patients with head and neck cancer: implications for radiation therapy. Int J Radiat Biol. 2009;85(9):796-804. https://doi.org/10.1080/09553000903039180
Syed M, Flechsig P, Liermann J, et al. Fibroblast activation protein inhibitor (FAPI) PET for diagnostics and advanced targeted radiotherapy in head and neck cancers. Eur J Nucl Med Mol Imaging. 2020;47(12):2836-2845. https://doi.org/10.1007/s00259-020-04859-y
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87-108. https://doi.org/10.3322/caac.21262
Altekruse SF, Devesa SS, Dickie LA, McGlynn KA, Kleiner DE. Histological classification of liver and intrahepatic bile duct cancers in SEER registries. J Regist Manag. 2011;38(4):201-205.
Massarweh NN, El-Serag HB. Epidemiology of Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma. Cancer Control J Moffitt Cancer Cent. 2017;24(3):1073274817729245. https://doi.org/10.1177/1073274817729245
Bennett GL, Krinsky GA, Abitbol RJ, Kim SY, Theise ND, Teperman LW. Sonographic detection of hepatocellular carcinoma and dysplastic nodules in cirrhosis: correlation of pretransplantation sonography and liver explant pathology in 200 patients. AJR Am J Roentgenol. 2002;179(1):75-80. https://doi.org/10.2214/ajr.179.1.1790075
Lee YJ, Lee JM, Lee JS, et al. Hepatocellular carcinoma: diagnostic performance of multidetector CT and MR imaging-a systematic review and meta-analysis. Radiology. 2015;275(1):97-109. https://doi.org/10.1148/radiol.14140690
Kim CK, Lim JH, Lee WJ. Detection of hepatocellular carcinomas and dysplastic nodules in cirrhotic liver: accuracy of ultrasonography in transplant patients. J Ultrasound Med Off J Am Inst Ultrasound Med. 2001;20(2):99-104. https://doi.org/10.7863/jum.2001.20.2.99
Bruix J, Reig M, Rimola J, et al. Clinical decision making and research in hepatocellular carcinoma: pivotal role of imaging techniques. Hepatol Baltim Md. 2011;54(6):2238-2244. https://doi.org/10.1002/hep.24670
Ho CL, Yu SCH, Yeung DWC. 11C-acetate PET imaging in hepatocellular carcinoma and other liver masses. J Nucl Med Off Publ Soc Nucl Med. 2003;44(2):213-221.
Iwata Y, Shiomi S, Sasaki N, et al. Clinical usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose in the diagnosis of liver tumors. Ann Nucl Med. 2000;14(2):121-126. https://doi.org/10.1007/BF02988591
Khan MA, Combs CS, Brunt EM, et al. Positron emission tomography scanning in the evaluation of hepatocellular carcinoma. J Hepatol. 2000;32(5):792-797. https://doi.org/10.1016/s0168-8278(00)80248-2
Trojan J, Schroeder O, Raedle J, et al. Fluorine-18 FDG positron emission tomography for imaging of hepatocellular carcinoma. Am J Gastroenterol. 1999;94(11):3314-3319. https://doi.org/10.1111/j.1572-0241.1999.01544.x
Mertens JC, Rizvi S, Gores GJ. Targeting cholangiocarcinoma. Biochim Biophys Acta Mol Basis Dis. 2018;1864(4 Pt B):1454-1460. https://doi.org/10.1016/j.bbadis.2017.08.027
Zou B, Liu X, Zhang B, et al. The Expression of FAP in Hepatocellular Carcinoma Cells is Induced by Hypoxia and Correlates with Poor Clinical Outcomes. J Cancer. 2018;9(18):3278-3286. https://doi.org/10.7150/jca.25775
Guo W, Pang Y, Yao L, et al. Imaging fibroblast activation protein in liver cancer: a single-center post hoc retrospective analysis to compare [68Ga]Ga-FAPI-04 PET/CT versus MRI and [18F]-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2021;48(5):1604-1617. https://doi.org/10.1007/s00259-020-05095-0
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7-34. https://doi.org/10.3322/caac.21551
Leppänen J, Lindholm V, Isohookana J, et al. Tenascin C, Fibronectin, and Tumor-Stroma Ratio in Pancreatic Ductal Adenocarcinoma. Pancreas. 2019;48(1):43-48. https://doi.org/10.1097/MPA.0000000000001195
Spill F, Reynolds DS, Kamm RD, Zaman MH. Impact of the physical microenvironment on tumor progression and metastasis. Curr Opin Biotechnol. 2016;40:41-48. https://doi.org/10.1016/j.copbio.2016.02.007
Valkenburg KC, de Groot AE, Pienta KJ. Targeting the tumour stroma to improve cancer therapy. Nat Rev Clin Oncol. 2018;15(6):366-381. https://doi.org/10.1038/s41571-018-0007-1
von Ahrens D, Bhagat TD, Nagrath D, Maitra A, Verma A. The role of stromal cancer-associated fibroblasts in pancreatic cancer. J Hematol OncolJ Hematol Oncol. 2017;10:76. https://doi.org/10.1186/s13045-017-0448-5
Röhrich M, Naumann P, Giesel FL, et al. Impact of 68Ga-FAPI PET/CT Imaging on the Therapeutic Management of Primary and Recurrent Pancreatic Ductal Adenocarcinomas. J Nucl Med Off Publ Soc Nucl Med. 2021;62(6):779-786. https://doi.org/10.2967/jnumed.120.253062
Loktev A, Lindner T, Burger EM, et al. Development of Fibroblast Activation Protein-Targeted Radiotracers with Improved Tumor Retention. J Nucl Med Off Publ Soc Nucl Med. 2019;60(10):1421-1429. https://doi.org/10.2967/jnumed.118.224469
Watabe T, Liu Y, Kaneda-Nakashima K, et al. Theranostics Targeting Fibroblast Activation Protein in the Tumor Stroma: 64Cu- and 225Ac-Labeled FAPI-04 in Pancreatic Cancer Xenograft Mouse Models. J Nucl Med Off Publ Soc Nucl Med. 2020;61(4):563-569. https://doi.org/10.2967/jnumed.119.233122
Lindner T, Loktev A, Altmann A, et al. Development of Quinoline-Based Theranostic Ligands for the Targeting of Fibroblast Activation Protein. J Nucl Med Off Publ Soc Nucl Med. 2018;59(9):1415-1422. https://doi.org/10.2967/jnumed.118.210443
Downloads
Published
How to Cite
Issue
Section
License
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


