Is Plasma Expander a Good Samaritan in Need?
Keywords:
Crystalloid Solution, Colloid Solution, Plasma ExpanderAbstract
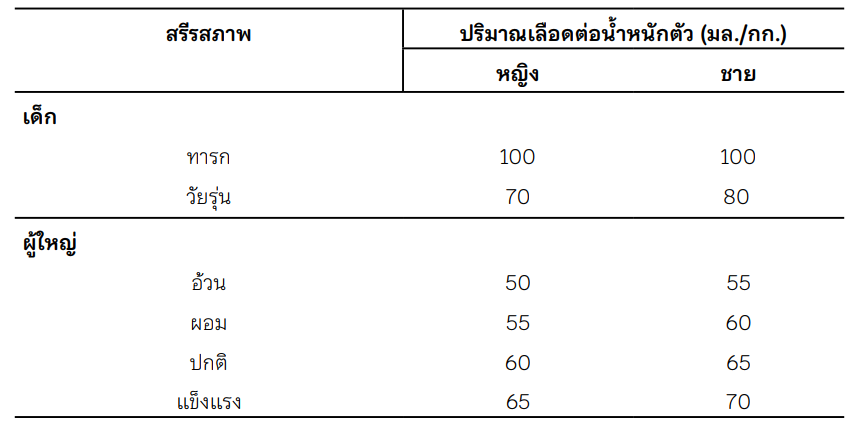
During admission of emergent patients with blood loss, medical personnel prefer to use crystalloid as prime solution to maintain blood circulation. However, in case of bleeding seems to fulfill all of criteria and blood bank processing takes time, a management with colloid solution or plasma expander is required to stabilize hemodynamic and preserve cellular oxygenation. The two kinds of plasma expander - natural e.g. albumin, fresh frozen plasma and artificial as gelatin, dextran and hydroxyethyl starch can markedly replenish tissue fluid and maintain hemodynamic status in equilibrium, as well as challenge unpredictability of pathological problems and diseases. Notwithstanding, the main concerns of colloid therapy are its molecular weight, colloidal osmotic pressure, plasma expansion volume, renal threshold, medical expenses, incidence of complications particularly coagulation disturbances, anaphylactoid and anaphylaxis as well.
Downloads
References
Butterworth IV JF, Mackey DC, Wasnick JD. Fluid Management & Blood Component Therapy. In: Morgan & Mikhail's Clinical Anesthesiology. 6th ed. McGraw-Hill Education; 2018. Accessed October 30, 2021. https://accessmedicine.mhmedical.com/content.aspx?bookid=2444§ionid=193557318
Sharma R, Sharma S. Physiology, Blood Volume. In: StatPearls. StatPearls Publishing; 2022. Accessed October 30, 2021. http://www.ncbi.nlm.nih.gov/books/NBK526077/
พงศ์ธารา วิจิตเวชไพศาล. A guide to parenteral nutrition. กรุงเทพฯ: ร้านค้าสโมสรแพทย์ศิร ิราช; 2534: 10-14.
Martino PL. Colloid and crystalloid resuscitation. In Martino PL, editor. The ICU Book. 3rd edition. Philadelphia: Churchill Livingstone; 2007. 233-254.
Raghunathan K, Murray PT, Beattie WS, Lobo DN, Myburgh J, Sladen R, et al. Choice of fluid in acute illness: what should be given? An international consensus. Br J Anaesth. 2014; 113 (5): 772-783. https://doi.org/10.1093/bja/aeu301
Williams EL, Hildebrand KL, McCormick SA, Bedel MJ. The effect of intravenous lactated Ringer's solution versus 0.9% sodium chloride solution on serum osmolality in human volunteers. Anesth Analg. 1999;88(5):999- 1003. https://doi.org/10.1097/00000539-199905000-00006
Prough DS, Bidani A. Hyperchloremic metabolic acidosis is a predictable consequence of intraoperative infusion of 0.9% saline. Anesthesiology. 1999;90(5):1247-1249. https://doi.org/10.1097/00000542-199905000-00003
Singh S, Kerndt CC, Davis D. Ringer's Lactate. In: StatPearls. StatPearls Publishing; 2021. Accessed October 30, 2021. http://www.ncbi.nlm.nih.gov/books/NBK500033/
Lactated Ringers - FDA prescribing information, side effects and uses. Drugs.com. Accessed November 11, 2021. https://www.drugs.com/pro/lactated-ringers.html
Mitra S, Khandelwal P. Are all colloids same? How to select the right colloid?. Indian J Anaesth. 2009;53(5):592-607.
Zhang S, Yang W, Chen H, Liu B, Lin B, Tao Y. Metabolic engineering for efficient supply of acetyl-CoA from different carbon sources in Escherichia coli. Microbial Cell Factories. 2019;18(1):130. https://doi.org/10.1186/s12934-019-1177-y
Vercueil A, Grocott MP, Mythen MG. Physiology, pharmacology, and rationale for colloid administration for the maintenance of effective hemodynamic stability in critically ill patients. Transfus Med Rev. 2005;19(2):93-109. https://doi.org/10.1016/j.tmrv.2004.11.006
Kaye AD, Kucera IJ. Intravascular fluid and electrolyte physiology. In: Miller RD, editor. Miller's Anesthesia. 6th edition. Philadelphia: Churchill Livingstone; 2005. 1763-1798.
Dubois MJ, Vincent JL. Colloid Fluids. In: Hahn RG, Prough DS, Svensen CH, editors. Perioperative Fluid Therapy. 1st edition. New York: Wiley; 2007. 153-611.
Barron ME, Wilkes MM, Navickis RJ. A systematic review of the comparative safety of colloids. Arch Surg. 2004;139(5):552-563. https://doi.org/10.1001/archsurg.139.5.552
Moman RN, Gupta N, Varacallo M. Physiology, Albumin. In: StatPearls. StatPearls Publishing; 2021. Accessed October 30, 2021. http:// www.ncbi.nlm.nih.gov/books/NBK459198/
Bentzer P, Thomas OD, Westborg J, Johansson PI, Schött U. The volume-expanding effects of autologous liquid stored plasma following hemorrhage. Scand J Clin Lab Invest.2012; 72(6):490-494. https://doi.org/10.3109/00365513.2012.699099
British Committee for Standards in Haematology C Blood Transfusion Task Force (J Duguid, O'Shaughnessy DF, Atterbury C, et al. Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br. J. Haematol. 2004;126(1):11-28. https://doi.org/10.1111/j.1365-2141.2004.04972.x
Structure and Function of Blood | Biology for Majors II. Accessed October 30, 2021. https://courses.lumenlearning.com/sunywmopen-biology2/chapter/introduction-tostructure-and-function-of-blood/
Khawar H, Kelley W, Stevens JB, Guzman N. Fresh Frozen Plasma (FFP). In: StatPearls. StatPearls Publishing; 2021. Accessed October 30, 2021. http://www.ncbi.nlm.nih.gov/books/NBK513347/
Laxenaire MC, Charpentier C, Feldman L. [Anaphylactoid reactions to colloid plasma substitutes: incidence, risk factors, mechanisms.A French multicenter prospective study]. Ann Fr Anesth Reanim. 1994;13(3):301-310. https://doi.org/10.1016/S0750-7658(94)80038-3
Miao KH, Guthmiller KB. Dextran. In:StatPearls. StatPearls Publishing; 2021. Accessed October 30, 2021. http://www.ncbi.nlm.nih.gov/books/ NBK557631/
Van der Linden P, Ickx BE. The effects of colloid solutions on hemostasis. Can J Anaesth. 2006;53(6 Suppl):S30-39. https://doi.org/10.1007/BF03022250
Nearman HS, Herman ML. Toxic effects of colloids in the intensive care unit. Crit Care Clin. 1991;7(3):713-723. https://doi.org/10.1016/S0749-0704(18)30302-6
Westphal M, James MF, Kozek-Langenecker S, Stocker R, Guidet B, Van Aken H. Hydroxyethyl starches: different products--different effects. Anesthesiology.2009;111(1):187-202.
https://doi.org/10.1097/ALN.0b013e3181a7ec82
Saunders CR, Carlisle L, Bick RL. Hydroxyethyl starch versus albumin in cardiopulmonary bypass prime solutions. Ann Thorac Surg. 1983;36(5):532-539.doi:10.1016/s0003-4975(10)60683-2
https://doi.org/10.1016/S0003-4975(10)60683-2
Perner A, Haase N, Winkel P, et al. Long-term outcomes in patients with severe sepsis randomised to resuscitation with hydroxyethyl starch 130/0.42 or Ringer's acetate. Intensive Care Med. 2014;40(7):927-934. https://doi.org/10.1007/s00134-014-3311-y
Davidson IJ. Renal impact of fluid management with colloids: a comparative review. Eur J Anaesthesiol. 2006;23(9):721-738. https://doi.org/10.1017/S0265021506000639
Hydroxyethyl Starch - an overview | ScienceDirect Topics. Accessed October 30, 2021. https://www.sciencedirect.com/topics/medicine-and-dentistry/hydroxyethyl-starch
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.