Promoting exercise and nutrition in patients with diabetes in the situation of the Covid-19 pandemic
Keywords:
Health promotion for patients with diabetes, COVID-19 pandemic, Exercise and nutritionAbstract
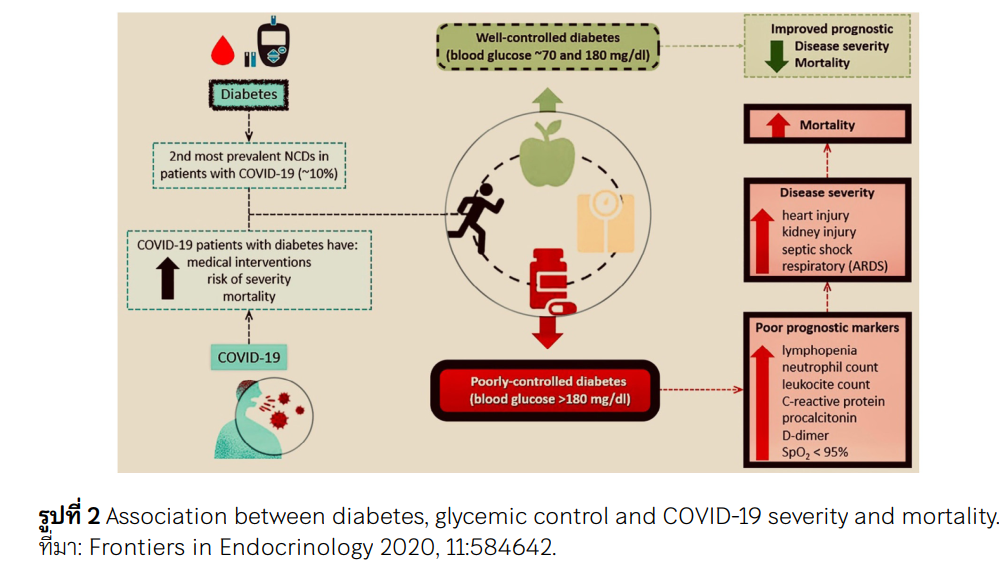
Health promotion for patients with diabetes in the situation of the Covid-19 pandemic with exercise and nutrition. The objective was to recommend for patients with diabetes from the pandemic situation of COVID-19. According to the effects of physiological and pathological conditions of the COVID-19 in patients with diabetes, the coronavirus (SARS-CoV-2) was more easily to captured into the lung epithelial cells in large numbers.As a result of a viral infection, it was more difficult to control blood sugar level. Which weakened the immune system, making it easier for the virus grow up, it could potentially result in severe symptoms. Therefore, the health of patients with diabetes should be promoted to prevent disease.
Both aerobic and resistance exercise were significant improved insulin sensitivity. Home-based exercise programs and workout in a hospital were effective to diabetes control. The nutrition should contain complex carbohydrates which low glycemic index, essential fatty acids containing EPA and DHA, and rich source of protein from fish and chicken. A Mediterranean eating pattern rich in monounsaturated and polyunsaturated fats may be considered to improve glucose metabolism and lower cardiovascular disease risk, according to ADA standard guidelines.
Downloads
References
World health organization. WHO Coronavirus (COVID-19) Dashboard. Accessed May 2, 2022. https://covid19.who.int
Pak A, Adegboye OA, Adekunle AI, Rahman KM, McBryde ES, Eisen DP. Economic Consequences of the COVID-19 Outbreak: the Need for Epidemic Preparedness. Front Public Health. 2020;8:241. https://doi.org/10.3389/fpubh.2020.00241 PMid:32574307 PMCid:PMC7273352
Chee YJ, Tan SK, Yeoh E. Dissecting the interaction between COVID-19 and diabetes mellitus. J Diabetes Investig. 2020;11(5): 1104-1114. https://doi.org/10.1111/jdi.13326 PMid:32558211 PMCid:PMC7323255
Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17(9):543-558. https://doi.org/10.1038/s41569-020-0413-9 PMid:32690910 PMCid:PMC7370876
World health organization. Coronavirus disease (COVID-19) questions and answers (general). Accessed May 1, 2022. https://www.who.int/thailand/emergencies/novel-coronavirus- 2019/q-a-on-covid-19/q-a-on-covid-19-general
CDC. People with Certain Medical Conditions. Centers for Disease Control and Prevention. Accessed May 1, 2022. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
Department of disease control. Department of disease control advises diabetic patients to control blood sugar with medication and vaccination against COVID-19 Accessed May 1, 2022. https://ddc.moph.go.th/brc/news.php?news=20276&deptcode=brc
Thai Health Project. 2021. COVID-19 Disaster Shakes the World. Nakhon Pathom: Institute for Population and Social Research, Mahidol University. Accessed May 1, 2022. https://www.hiso.or.th/hiso/picture/reportHealth/report/ThaiHealth2021e.pdf
Brufsky A. Hyperglycemia, hydroxychloroquine, and the COVID-19 pandemic. J Med Virol. 2020;92(7):770-775. https://doi.org/10.1002/jmv.25887 PMid:32293710 PMCid:PMC7262330
Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020; 8(4):420-422. https://doi.org/10.1016/S2213-2600(20)30076-X PMid:32085846
Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648 PMid:32091533
Fadaka AO, Sibuyi NRS, Adewale OB, et al. Understanding the epidemiology, pathophysiology, diagnosis and management of SARS-CoV-2. J Int Med Res. 2020;48(8): 300060520949077. https://doi.org/10.1177/0300060520949077 PMid:32842818 PMCid:PMC7453465
Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARSCoV-2 by full-length human ACE2. Science. 2020;367(6485):1444-1448. https://doi.org/10.1126/science.abb2762 PMid:32132184 PMCid:PMC7164635
Verma AK, Beg MMA, Bhatt D, et al. Assessment and Management of Diabetic Patients During the COVID-19 Pandemic. Diabetes Metab Syndr Obes. 2021;14:3131-3146. https://doi.org/10.2147/DMSO.S285614 PMid:34262317 PMCid:PMC8275137
Bode B, Garrett V, Messler J, et al. Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States [published correction appears in J Diabetes Sci Technol. 2020 Jun 10;: 1932296820932678]. J Diabetes SciTechnol. 2020;14(4):813-821. https://doi.org/10.1177/1932296820924469 PMid:32389027 PMCid:PMC7673150
Raveendran AV, Misra A. Post COVID-19 Syndrome ("Long COVID") and Diabetes: Challenges in Diagnosis and Management. Diabetes Metab Syndr. 2021;15(5):102235. https://doi.org/10.1016/j.dsx.2021.102235 PMid:34384972 PMCid:PMC8317446
Department of disease control. Guideline for preventing Coronavirus disease 2019 or COVID-19 for general and high risk patient. Department of disease control. Accessed May 1, 2022. https://ddc.moph.go.th/viralpneumonia/int_protection.php
Marçal IR, Fernandes B, Viana AA, Ciolac EG. The Urgent Need for Recommending Physical Activity for the Management of Diabetes During and Beyond COVID-19 Outbreak. Front Endocrinol(Lausanne).2020;11:584642. https://doi.org/10.3389/fendo.2020.584642 PMid:33250859 PMCid:PMC7673403
Zhu L, She ZG, Cheng X, et al. Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 2020;31(6): 1068-1077.e3.
https://doi.org/10.1016/j.cmet.2020.04.021 PMid:32369736 PMCid:PMC7252168
Bando H. Recommended adequate exercise for diabetic patients in response to new lifestyle manner with corona era for Global health. MOJ Public Health. 2020;9(4):113-115. https://doi.org/10.15406/mojph.2020.09.00333
American Diabetes Association. American Diabetes Association Standards of Medical Care in Diabetes 2019. Diabetes Care. Accessed May 1, 2022. https://www.sharphealthplan.com/docs/default-source/providers/clinical-resources/2019-ada-standardsof-medical-care-in-diabetes.pdf.
Riebe D, Ehrman JK, Liguori G, Magal M. Acsm's Guidelines for Exercise Testing and Prescription. 10th ed. Philadelphia: Wolters Kluwer Health Publishers; 2018. P.293-297.
Gray A, Threlkeld RJ. Nutritional Recommendations for Individuals with Diabetes. In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext. South Dartmouth (MA): MDText. com, Inc.; October 13, 2019.
Maiorino MI, Bellastella G, Longo M, Caruso P, Esposito K. Mediterranean Diet and COVID-19: Hypothesizing Potential Benefits in People With Diabetes. Front Endocrinol (Lausanne). 2020;11:574315. https://doi.org/10.3389/fendo.2020.574315 PMid:33042027 PMCid:PMC7525209
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


