Effect of Low-Dose Heparinized Saline (LDHS) on Arterial Line Patency Patients with Severe COVID-19 Disease
Keywords:
Arterial line, COVID-19, Critical care, HeparinAbstract
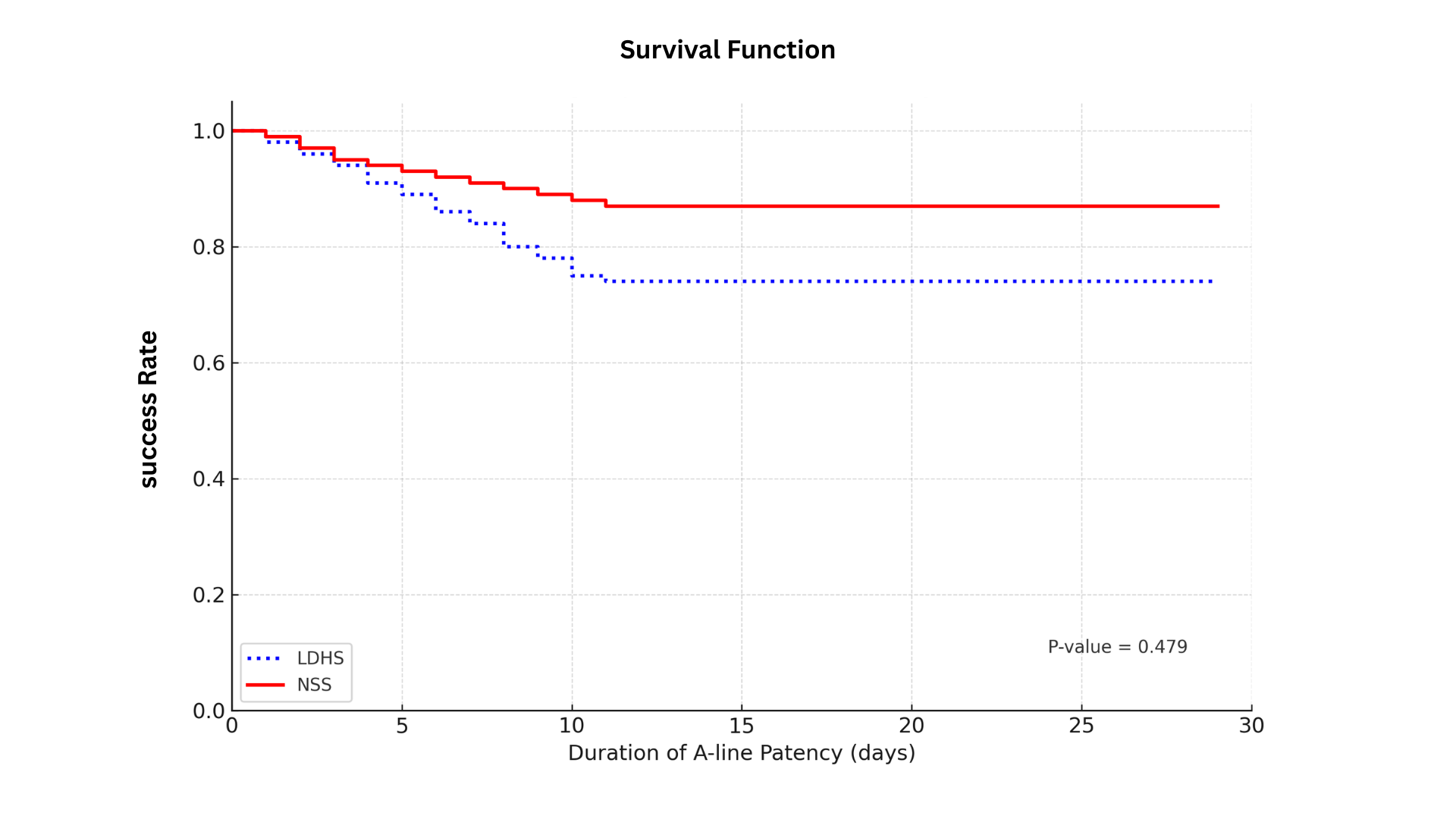
Introduction: In critically ill COVID-19 patients, arterial line (A-line) occlusion occurs more frequently than in general ICU patients when 0.9% NSS is used as a flushing solution. Objective: To evaluate the effectiveness of low-dose heparinized saline (LDHS), consisting of 2 units of heparin per 1 mL of 0.9% NSS, in maintaining arterial line (A-line) patency in critically ill COVID-19 patients. Methods: This randomized controlled trial included 61 critically ill COVID-19 patients, an experimental group (n=31) receiving LDHS and a control group (n=30) receiving NSS. Both solutions were administered under continuous pressure using a pressure bag inflated to 400 mmHg. Data collection tools included: 1) experimental instruments and 2) data recording forms. Data Analysis: The proportion of functional arterial lines and complication rates were compared between groups using Pearson’s chi-square test. Duration of line patency was analyzed using Kaplan–Meier survival analysis and the log-rank test. Results: LDHS and NSS demonstrated comparable effectiveness in preventing arterial line occlusion, with mean patency durations of 22.47 days and 26.36 days, respectively (p = .479). Conclusion: In critically ill COVID-19 patients, 0.9% NSS can be effectively used as an arterial line flushing solution when combined with a pressure bag inflated to 400 mmHg, thereby extending line patency without the need for heparin.
Downloads
References
Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2020;18(7):1559-1561. doi:10.1111/jth.14849.
Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18(5):1023-1026. doi:10.1111/jth.14810.
Everson M, Webber L, Penfold C, Shah S, Freshwater-Turner D. Finding a solution: Heparinised saline versus normal saline in the maintenance of invasive arterial lines in intensive care. J Intensive Care Soc. 2016;17(4):284-289. doi:10.1177/1751143716653763.
Zhong L, Wang HL, Xu B, et al. Normal saline versus heparin for patency of central venous catheters in adult patients - a systematic review and meta-analysis. Crit Care. 2017;21(1):5. doi:10.1186/s13054-016-1585-x.
Ziyaeifard M, Ferasat-Kish R, Azarfarin R, et al. Comparison of the effect of heparinized normal saline solution versus saline solutions in arterial and central venous catheters on complete blood count after cardiac surgery. Anesth Pain Med. 2022;12(4):e113345. doi:10.5812/aapm-113345.
Robertson-Malt S, Malt GN, Farquhar V, Greer W. Heparin versus normal saline for patency of arterial lines. Cochrane Database Syst Rev. 2014;2018(5):CD007364. doi:10.1002/14651858.CD007364.pub2.
Ishii Y, Mishima S, Aida K, Oda J. Comparison of normal saline and heparinized solutions for the maintenance of arterial catheter pressure waves: A randomized pilot study. Signa Vitae. 2021 Feb;17(1):51-5. doi:10.22514/sv.2020.16.0088.
Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089-1098. doi:10.1007/s00134-020-06062-x.
Nadkarni GN, Lala A, Bagiella E, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76(16):1815-1826. doi:10.1016/j.jacc.2020.08.041.
Maurer LR, Luckhurst CM, Hamidi A, et al. A low dose heparinized saline protocol is associated with improved duration of arterial line patency in critically ill COVID-19 patients. J Crit Care. 2020;60:253-259. doi:10.1016/j.jcrc.2020.08.025.
Hamad AA, Ahmed SK. Understanding the lower and upper limits of sample sizes in clinical research. Cureus. 2025;17(1):e76724. doi:10.7759/cureus.76724.
P. Hanrahan N, Letourneau L, Batty R. Nurse management of radial arterial lines: Quality & Safety. Am J Nurs Res. 2022;10(1):7-15. doi:10.12691/ajnr-10-1-2.
Atef Fathi Moosa Elkholy M, Faltas Marzouk S, Ahmed Elhaweet E. Nurses’ compliance with safety measures of arterial line. Egyptian Journal of Health Care. 2024;15(4):49-61. doi:10.21608/ejhc.2024.383810.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Chulabhorn Royal Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright and Disclaimer
Articles published in this journal are the copyright of Chulabhorn Royal Academy.
The opinions expressed in each article are those of the individual authors and do not necessarily reflect the views of Chulabhorn Royal Academy or any other faculty members of the Academy. The authors are fully responsible for all content in their respective articles. In the event of any errors or inaccuracies, the responsibility lies solely with the individual authors.


