The Development of an Assessment System on Clinical Deterioration Monitoring Using Phachomklao Modified Early Warning Sign Scores (PCK MEWS Scores) among Intracerebral Hemorrhage Patients
Keywords:
Assessment System, Clinical Deterioration Monitoring, Early Warning Signs, Intracerebral HemorrhageAbstract
This research and development study aimed to develop an assessment system on clinical deterioration monitoring using Phrachomklao (PCK) Modified Early Warning Scores (MEWS) among intracerebral hemorrhage patients. There were four phases in this research procedure. Phase 1 was to analyze situations and problems by reviewing medical records and conducting semi-structured focus group interviews. Participants in this process consisted of 12 workers, including physicians, head nurses and registered nurses. Phase 2 was to develop the assessment system based on the evidence-based practice. Phase 3 was to conduct a quasi-experimental research to trial the assessment system among 37 intracranial hemorrhage patients per groups. Phase 4 was to evaluate the outcomes after applying the assessment system. This phase was evaluated by 44 registered nurses. Research instruments in a qualitative process were a semi-structured interview and a focus group discussion. Research instruments in a quantitative process were the satisfaction assessment form and the feasibility assessment form for using the system. Content analysis was used to analyze qualitative data. Frequencies and means were used to analyze quantitative data.
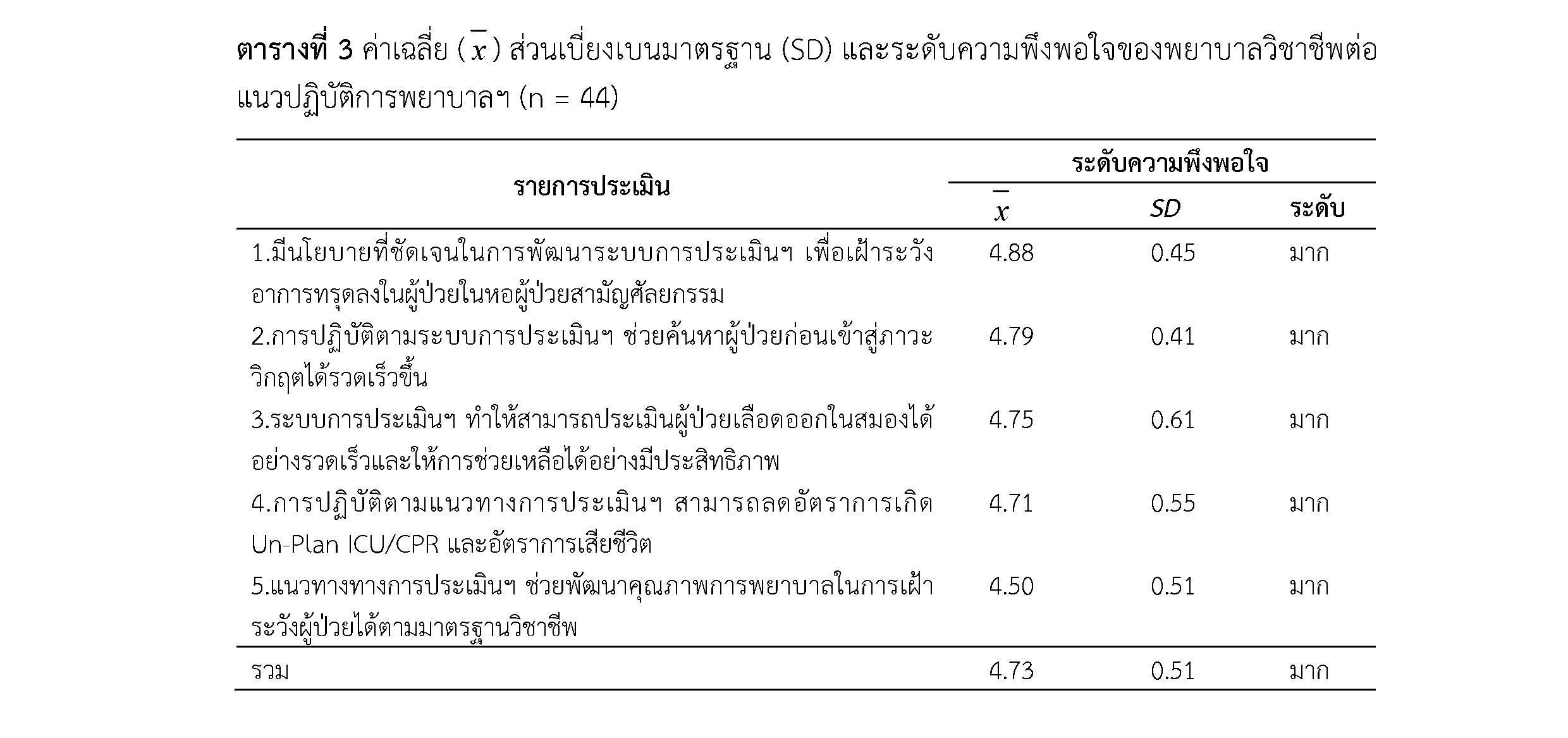
The results showed that the assessment system on clinical deterioration monitoring based on the PCK MEWS included: 1) collaborative planning; 2) clearly define roles and responsibilities; 3) effective communication; and 4) controlling, regulating, and monitoring the practice. After applying the assessment system on clinical deterioration monitoring, it was found that the percentage of unplanned transfers to the intensive care unit dropped from 27.28% in the control group and 9.09 % in the experimental group. The opinion of registered nurses on the feasibility of using the assessment system was at a high level (= 4.43). The satisfaction of registered nurses after using this system was also at a high level (
= 4.73). This research results suggested that nurses or other health care providers can be applied this assessment on the clinical deterioration monitoring in patients with other diseases in order to improve a quality of patient care.
References
Abidin, Z., Sila, N. A., Revai, A., & Liputo, G. P. (2017). Modified early warning system (Mews), indicator of changes in patient’s condition in the general wards: A systematic review. In 8th International Nursing Conference on Education, Practice and Research Development in Nursing, 3(1), 51-55.
Cohen, J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98-101.
Diana, M., Prayoga, D. H., & Wijayanti, D. P. (2021). Implementation of Early Warning System In Nursing Ward: A Literature Review. Nurse and Health: Journal Keperawatan, 10(1), 126-134.
Downey, C. L., Tahir, W., Randell, R., Brown, J. M., & Jayne, D. G. (2017). Strengths and limitations of early warning scores: A systematic review and narrative synthesis. International Journal of Nursing Studies, 76, 106-119.
Drower, D., McKeany, R., Jogia, P., & Jull, A. (2013). Evaluating the impact of implementing an early warning score system on incidence of in-hospital cardiac arrest. New zealand Medical Journal, 126(1385), 26-34.
Hester, J., Youn, T. S., Trifilio, E., Robinson, C. P., Babi, M. A., Ameli, P., ... & Busl, K. M. (2021). The Modified Early Warning Score: A Useful Marker of Neurological Worsening but Unreliable Predictor of Sepsis in the Neurocritically Ill—A Retrospective Cohort Study. Critical Care Explorations, 3(5), 1-11.
Karsy, M., Couldwell, W. T., Stanford, M., Breviu, A., & Horton, D. (2020). Using the Modified Early Warning Score (mEWS) to Improve Prediction of Outcome in Neurosurgical Patients. Neurosurgery, 67(Supplement_1), nyaa447_501.
Kim, D. K., Lee, D. H., Lee, B. K., Cho, Y. S., Ryu, S. J., Jung, Y. H., ... & Han, J. H. (2021). Performance of Modified Early Warning Score (MEWS) for predicting in-hospital mortality in traumatic brain injury patients. Journal of Clinical Medicine, 10(9), 1915.
Kirshner, H., & Schrag, M. (2021). Management of Intracerebral Hemorrhage: Update and Future Therapies. Current Neurology and Neuroscience Reports, 21(10), 1-5.
Kyriacos, U., Jelsma, J., James, M., & Jordan, S. (2015). Early warning scoring systems versus standard observations charts for wards in South Africa: A cluster randomized controlled trial. Trials, 16(1), 1-15.
Lagadec,L. M. D., Dwyer, T., & Browne, M. (2020). The efficacy of twelve early warning systems for potential use in regional medical facilities in Queensland, Australia. Australian Critical Care, 33(1), 47-53.
Le Lagadec, M. D., & Dwyer, T. (2017). Scoping review: the use of early warning systems for the identification of in-hospital patients at risk of deterioration. Australian Critical Care, 30(4), 211-218.
Le Lagadec, M. D., Dwyer, T., & Browne, M. (2020). The efficacy of twelve early warning systems for potential use in regional medical facilities in Queensland, Australia. Australian Critical Care, 33(1), 47-53.
Merriel, A., van der Nelson, H., Merriel, S., Bennett, J., Donald, F., Draycott, T., & Siassakos, D. (2016). Identifying deteriorating patients through multidisciplinary team training. American Journal of Medical Quality, 31(6), 589-595.
Nishijima, I., Oyadomari, S., Maedomari, S., Toma, R., Igei, C., Kobata, S., ... & Iha, K. (2016). Use of a modified early warning score system to reduce the rate of in-hospital cardiac arrest. Journal of Intensive Care, 4(1), 1-6.
O’Neill, S. M., Clyne, B., Bell, M., Casey, A., Leen, B., Smith, S. M., ... & O’Neill, M. (2021). Why do healthcare professionals fail to escalate as per the early warning system (EWS) protocol? A qualitative evidence synthesis of the barriers and facilitators of escalation. BMC Emergency Medicine, 21(1), 1-19.
Pimentel, M. A., Redfern, O. C., Malycha, J., Meredith, P., Prytherch, D., Briggs, J., ... & Watkinson, P. J. (2021). Detecting deteriorating patients in hospital: development and validation of a novel scoring system. American Journal of Respiratory and Critical Care Medicine, 204(1), 44-52.
Polit, D. F. B & Beck, CT (2014). Essentials of Nursing Research: Appraising Evidence for Nursing Practice. London, Lippincott.
Spencer, W., Smith, J., Date, P., de Tonnerre, E., & Taylor, D. M. (2019). Determination of the best early warning scores to predict clinical outcomes of patients in the emergency department. Emergency Medicine Journal, 36(12), 716-721.
Wang, A. Y., Fang, C. C., Chen, S. C., Tsai, S. H., & Kao, W. F. (2016). Periarrest Modified Early Warning Score (MEWS) predicts the outcome of in-hospital cardiac arrest. Journal of the Formosan Medical Association, 115(2), 76-82.
Downloads
Published
How to Cite
Issue
Section
License
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารวิจัยการพยาบาลและการสาธารณสุข ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารวิจัยการพยาบาลและการสาธารณสุข








