Effect of Slow Deep Breath on Chest Expansion, Pulmonary Function, and Heart Rate Recovery in Obese Persons Aged between 18 and 35 Years
Keywords:
Obesity, Force Vital Capacity, Heart Rate Recovery, Slow Deep BreathingAbstract
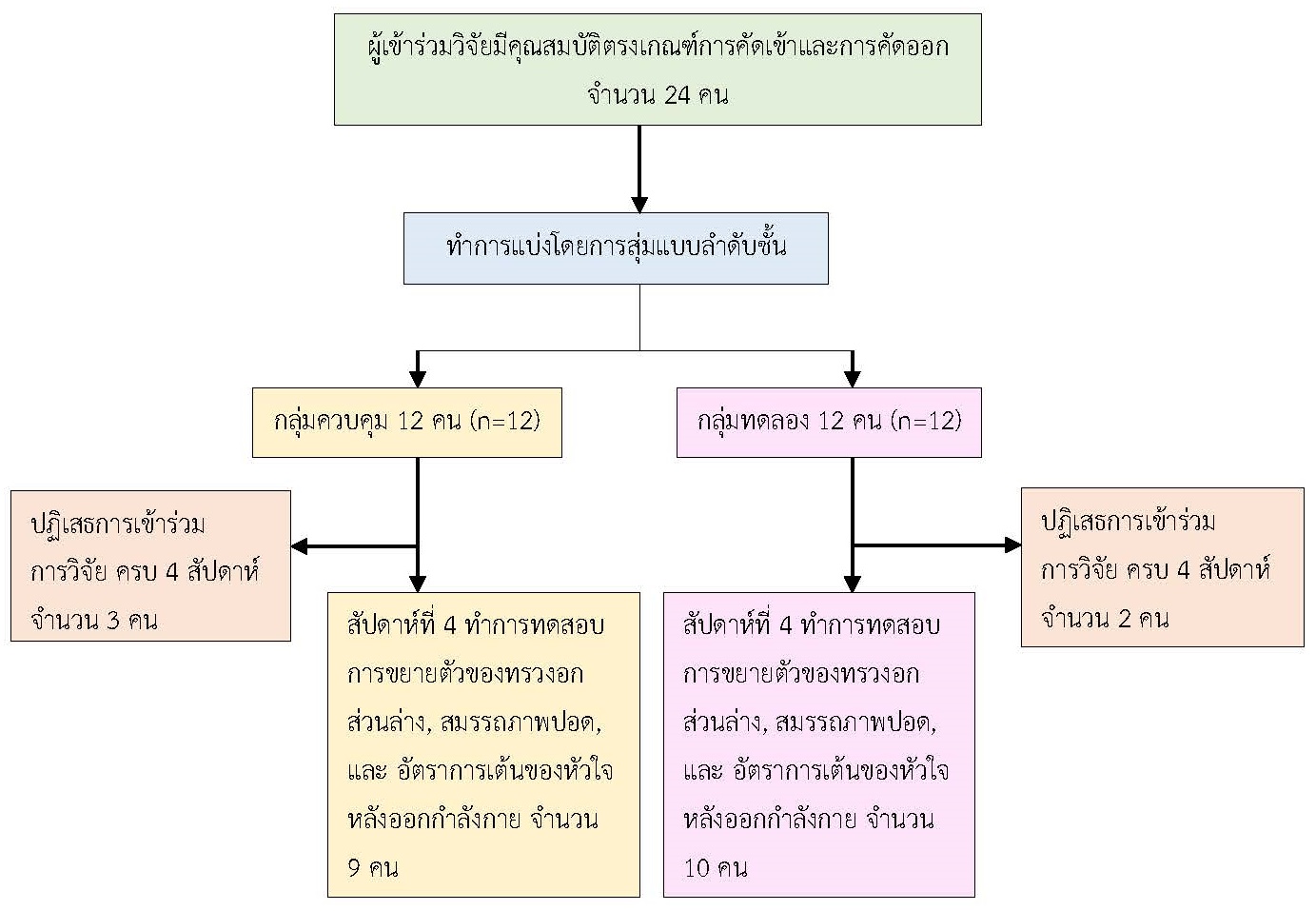
The objective of this randomized control trial research was to examine the change in chest expansion, pulmonary function, and heart rate recovery among obese persons after four weeks of diaphragmatic breathing exercise training. Participants were 19 obese persons, aged 18-35 years old, divided into two groups using stratified sampling. The control group included nine participants who were required to maintain daily health behaviors for four weeks. The intervention group consisted of 10 participants who practiced diaphragmatic breathing exercise training (DBE) six times in one minute, rested one minute, practiced 10 minutes per time, and practiced every day for four weeks. Both groups measured the change in chest expansion, predicted forced vital capacity (FVC), predicted forced expiratory volume in one second (FEV1), predicted ratio of the forced expiratory volume in one second to the forced vital capacity (FEV1/FVC), predicted maximum voluntary ventilation (MVV), and heart rate recovery (HRR) before and after the experiment. The data were analyzed using a two-way analysis of variance (Two-way ANOVA).
The results showed that when comparing the results before and after the 4-week experiment, the intervention group had a statistically significant increase in the mean chest expansion (before the experiment: Mean ± SEM=2.2 ± 0.32 cm, after the experiment: Mean ± SEM= 2.95 ± 0.24 cm, p-value = 0.001). The control group had a statistically significant decrease in %predicted FVC (before the experiment: Mean ± SEM=101± 3.45, after the experiment: Mean ± SEM= 96.70 ± 3.32, p-value = 0.001). There were no statistically significant differences in the changes in %predicted FEV1/FVC, predicted MVV, and HRR values in both the experimental and control groups. It was concluded that practicing diaphragmatic breathing exercises for four weeks effectively enhanced chest expansion without changing pulmonary function and autonomic imbalance in obese persons in early adulthood.
References
Ansari, S., Haboubi, H., & Haboubi, N. (2020). Adult obesity complications: Challenges and clinical impact. Therapeutic Advances in Endocrinology and Metabolism, 11, 204201882093495. https://doi.org/10.1177/2042018820934955
Barbosa Lins, T. C., Valente, L. M., Sobral Filho, D. C., & Barbosa e Silva, O. (2015). Relation between heart rate recovery after exercise testing and body mass index. Revista Portuguesa de Cardiologia, 34(1), 27-33. https://doi.org/10.1016/j.repc.2014.07.006
Barcelar J. dem., et al. (2014). The expansion of the pulmonary rib cage during breath stacking is influenced by age in obese women. PLoS One, 9(11), e110959. https://doi.org/10.1371/journal.pone.0110959
Bhaskaran, K., Dos-Santos-Silva, I., Leon, D. A., Douglas, I. J., & Smeeth, L. (2018). Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol, 6(12), 944-953. https://doi.org/10.1016/s2213-8587(18)30288-2
Chlif, M., Keochkerian, D., Choquet, D., Vaidie, A., & Ahmaidi, S. (2009). Effects of obesity on breathing pattern, ventilatory neural drive and mechanics. Respiratory Physiology & Neurobiology, 168(3), 198-202. https://doi.org/10.1016/j.resp.2009.06.012
Dixon, A. E., & Peters, U. (2018). The effect of obesity on lung function. Expert Review of Respiratory Medicine, 12(9), 755-767. https://doi.org/10.1080/17476348.2018.1506331
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/bf03193146
Gallagher, D., et al. (2000). Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. The American Journal of Clinical Nutrition, 72(3), 694-701. https://doi.org/10.1093/ajcn/72.3.694
González, Y., et al., (2022). Pulmonary function test in obese patients. European Respiratory Journal, 60(suppl 66), 3060. https://doi.org/10.1183/13993003.congress-2022.3060
Hirakawa, Y., et al. (2016). The impact of body mass index on the associations of lipids with the risk of coronary heart disease in the Asia Pacific region. Preventive Medicine Reports, 3, 79-82. https://doi.org/10.1016/j.pmedr.2015.12.012
Hough. (2014). Physiotherapy in Respiratory and Cardiac Care: A problem-solving approach to respiratory and cardiac management (2 ed.). Oxford Singular Publishing Group.
Jerath, R., Edry, J. W., Barnes, V. A., & Jerath, V. (2006). Physiology of long pranayamic breathing: Neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Medical Hypotheses, 67(3), 566-571. https://doi.org/10.1016/j.mehy.2006.02.042
Kinlen, D., Cody, D., & O'Shea, D. (2018). Complications of obesity. QJM: An International Journal of Medicine, 111(7), 437-443. https://doi.org/10.1093/qjmed/hcx152
Mafort, T. T., Rufino, R., Costa, C. H., & Lopes, A. J. (2016). Obesity: Systemic and pulmonary complications, biochemical abnormalities, and impairment of lung function. Multidisciplinary Respiratory Medicine, 11, 28. https://doi.org/10.1186/s40248-016-0066-z
Mehari, A., et al. (2015). Obesity and Pulmonary Function in African Americans. PLoS One, 10(10), e0140610. https://doi.org/10.1371/journal.pone.0140610
Melo, L. C., Silva, M. A., & Calles, A. C. (2014). Obesity and lung function: A systematic review. Einstein (Sao Paulo), 12(1), 120-125. https://doi.org/10.1590/s1679-45082014rw2691
Mendonça, J., Pereira, H., Xará, D., Santos, A., & Abelha, F. J. (2014). Obese patients: Respiratory complications in the post-anesthesia care unit. Revista Portuguesa de Pneumologia, 20(1), 12-19. https://doi.org/10.1016/j.rppneu.2013.04.002
Olsén, M. F., Lönroth, H., & Bake, B. (1999). Effects of breathing exercises on breathing patterns in obese and non-obese subjects. Clinical Physiology and Biochemistry, 19(3), 251-257. https://doi.org/10.1046/j.1365-2281.1999.00167.x
Pal, G. K., Velkumary, S., & Madanmohan. (2004). Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian Journal of Medical Research, 120(2), 115-121.
Paprika, D., Gingl, Z., Rudas, L., & Zöllei, E. (2014). Hemodynamic effects of slow breathing: Does the pattern matter beyond the rate? Acta Physiologica Hungarica, 101(3), 273-281. https://doi.org/10.1556/aphysiol.101.2014.3.2
Shah, N. M., & Kaltsakas, G. (2023). Respiratory complications of obesity: From early changes to respiratory failure. Breathe (Sheff), 19(1), 220263. https://doi.org/10.1183/20734735.0263-2022
Zammit, C., Liddicoat, H., Moonsie, I., & Makker, H. (2010). Obesity and respiratory diseases. International Journal of General Medicine, 3, 335-343. https://doi.org/10.2147/ijgm.s11926
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Journal of Nursing and Public Health Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารวิจัยการพยาบาลและการสาธารณสุข ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารวิจัยการพยาบาลและการสาธารณสุข








