Effects of the Dietary Education Program in Conjunction with the Salt Meter on Reducing Sodium Intake, Blood Pressure Levels, and Glomerular Filtration Rate Among Uncontrolled Hypertension Patients
Keywords:
A Salt Meter, 24-Hour Urine Sodium, Glomerular Filtration Rate, Uncontrolled Hypertension PatientsAbstract
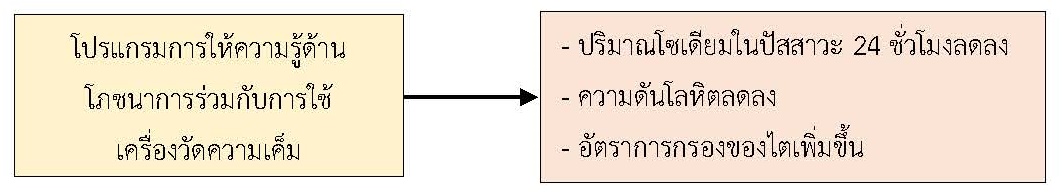
The objective of this quasi-experimental research was to examine the effects of the dietary education program in conjunction with the salt meter on reducing sodium intake, blood pressure levels, and glomerular filtration rate among uncontrolled hypertension patients. Participants were 50 uncontrolled hypertension patients who received services from the chronic non-communicable disease clinic, Ban Phue Hospital, and were divided into an experimental group of 25 people and a control group of 25 people. The experimental group received the dietary education program in conjunction with the salt meter for a period of 8 weeks. The control group received only the dietary education program. The research instrument was the dietary education program in conjunction with the salt meter. The data collection tools included a general data recording form, a blood pressure record form, and laboratory test results records, including 24-hour urine sodium content and glomerular filtration rate. The data were analyzed using descriptive statistics. Comparing the mean 24-hour urine sodium content, blood pressure level, and glomerular filtration rate with independent t-test statistics.
The results showed that the mean systolic blood pressure values between the experimental group and the control group before and after the program at the 8th week were statistically significantly different (p-value = 0.02). However, the mean 24-hour urine sodium content, the mean diastolic blood pressure, and the mean glomerular filtration rate between the experimental group and the control group before and after receiving the program at the 8th week showed no statistically significant differences. (p-value > 0.05). This research shows that this program can be used in patients with high blood pressure to promote healthy behaviors in order to control levels of blood pressure and prevent various complications that may occur in the future.
References
กรรณิกา สุวรรณา และคณะ (2564). ประสิทธิผลของโปรแกรมลดการบริโภคเกลือในอาหารต่อพฤติกรรมการบริโภคอาหารในกลุ่มเสี่ยงโรคความดันโลหิตสูง: กรณีศึกษาจังหวัดนครศรีธรรมราช. วารสารวิทยาศาสตร์สุขภาพแห่งประเทศไทย, 3(2), 1-13.
กลุ่มงานอายุรกรรม โรงพยาบาลบ้านผือ (2565). สถิติผู้ป่วยโรคความดันโลหิตสูง โรงพยาบาลบ้านผือ. อุดรธานี: โรงพยาบาลบ้านผือ.
กองโรคไม่ติดต่อ กรมคบคุมโรค. (2565). รายละเอียดตัวชี้วัดเพื่อกำกับติดตามคุณภาพบริการการดำเนินงานด้านโรคไม่ติดต่อ (โรคเบาหวานและโรคความดันโลหิตสูง) ประจำปีงบประมาณ พ.ศ. 2565. สืบค้นเมื่อ 18 กุมภาพันธ์ 2566 จาก http://www.thaincd.com/2016/media detail.php?id=14109&tid=&gid=1-015-005
วิชัย เอกพลากร. (2564). การสำรวจสุขภาพประชาชนไทยโดยการตรวจร่างกาย ครั้งที่ 6 พ.ศ. 2562-2563. กรุงเทพฯ: คณะแพทยศาสตร์โรงพยาบาลรามาธิบดี มหาวิทยาลัยมหิดล.
สกุณา กัณหาสุระ และพรพิมล ชูพานิช. (2566). พฤติกรรมการบริโภคอาหารที่มีโซเดียมสูงและปัจจัยที่สัมพันธ์กับการบริโภคอาหารที่มีโซเดียมสูงของผู้ใหญ่ในอำเภอเมือง จังหวัดอุดรธานี. วารสารวิชาการสาธารณสุขชุมชน, 9(4), 154-165.
Aliasgharzadeh, S., Tabrizi, J. S., Nikniaz, L., Ebrahimi-Mameghani, M., & Lotfi Yagin, N. (2022). Effect of salt reduction interventions in lowering blood pressure: A comprehensive systematic review and meta-analysis of controlled clinical trials. Plos One, 17(12), e0277929). https://doi.org/10.1371/journal.pone.0277929
Campbell, N. R. C., et al. (2019). The International Consortium for Quality Research on Dietary Sodium/Salt (TRUE) position statement on the use of 24-hour, spot, and short duration (<24 hours) timed urine collections to assess dietary sodium intake. The Journal of Clinical Hypertension, 21(6), 700-709. https://doi.org/10.1111/jch.13551
Chailimpamontree, W., et al. (2021). Estimated dietary sodium intake in Thailand: A nationwide population survey with 24-hour urine collections. Journal of Clinical Hypertension (Greenwich, Conn.), 23(4), 744-754. https://doi.org/10.1111/jch.14147
Cohen J. (1988). Statistical power analysis for the behavioral sciences. New York, NY: Routledge Academic.
Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175-191. https://doi.org/10.3758/bf03193146
Grillo, A., Salvi, L., Coruzzi, P., Salvi, P., & Parati, G. (2019). Sodium intake and hypertension. Nutrients, 11(9), 1970. https://doi.org/10.3390/nu11091970
He, F. J., Pombo-Rodrigues, S., & MacGregor, G. A. (2014). Salt reduction in England from 2003 to 2011: Its relationship to blood pressure, stroke and ischemic heart disease mortality. BMJ Open, 4(4), e004549. https://doi.org/10.1136/bmjopen-2013-004549
He, F. J., Tan, M., Ma, Y., & MacGregor, G. A. (2020). Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. Journal of the American College of Cardiology, 75(6), 632-647. https://doi.org/10.1016/j.jacc.2019.11.055
Irwan, A. M., Kato, M., Kitaoka, K., Ueno, E., Tsujiguchi, H., & Shogenji, M. (2016). Development of the salt-reduction and efficacy-maintenance program in Indonesia. Nursing & Health Sciences, 18(4), 519-532. https://doi.org/10.1111/nhs.12305
Nakano, M., et al. (2016). Effect of intensive salt-restriction education on clinic, home, and ambulatory blood pressure levels in treated hypertension patients during a 3-month education period. Journal of Clinical Hypertension, 18(5), 385-392. https://doi.org/10.1111/jch.12770
Nguyen, B., Bauman, A., & Ding, D. (2019). Association between lifestyle risk factors and incident hypertension among middle-aged and older Australians. Preventive Medicine, 118, 73-80. https://doi.org/10.1016/j.ypmed.2018.10.007
Wiriyatanakorn, S., Mukdadilok, A., Kantachuvesiri, S., Mekhora, C., & Yingchoncharoen, T. (2021). Impact of self-monitoring of salt intake by salt meter in hypertensive patients: A randomized controlled trial (SMAL-SALT). Journal of Clinical Hypertension (Greenwich, Conn.), 23(10), 1852-1861. https://doi.org/10.1111/jch.14344
Wu, J., et al. (2005). A summary of the effects of antihy-pertensive medications on measured blood pressure. American Journal of Hypertension, 18(7), 935-942. https://doi.org/10.1016/j.amjhyper.2005.01.011
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Journal of Nursing and Public Health Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารวิจัยการพยาบาลและการสาธารณสุข ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารวิจัยการพยาบาลและการสาธารณสุข








