The Meaning of Healthcare Providers on Promoting Health Literacy for Women with Gestational Diabetes
Keywords:
Gestational Diabetes, Health Literacy, Multidisciplinary Health Team, Qualitative StudyAbstract
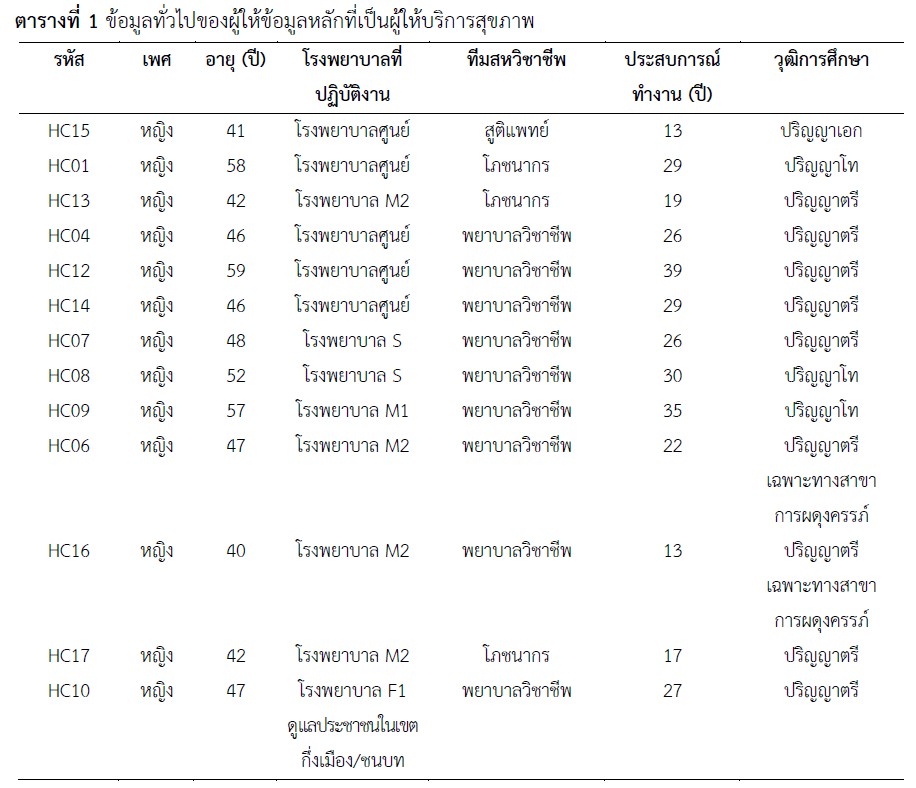
This qualitative study aimed to explore the meaning of healthcare providers on promoting health literacy for women with gestational diabetes. The study was conducted in nine hospitals within the Fourth Health Region of Thailand. Data were collected through in-depth interviews with 15 participants from a multidisciplinary team. The research instruments used were: 1) a general information collection form and 2) a set of questions on the perception of experiences in providing health literacy promotion services. Data were analyzed using content analysis.
The study found that the meaning of promoting health literacy from the perspective of healthcare providers was teaching to enhance health literacy, making pregnant women aware of the risks that affected their health and the health of their unborn babies. The teaching followed the guidelines of each hospital to reduce risks, and the best teaching method was individual instruction. Additionally, the characteristics of learners who were able to control their blood sugar levels well were those who were knowledgeable, interested, attentive, and inquisitive. The obstacles to teaching to promote health literacy included insufficient healthcare providers and inconsistent teaching methods. Therefore, supplementary teaching programs and a step-by-step review process during each appointment to monitor blood sugar control in pregnant women with diabetes were recommended.
References
ชนิกา ตู้จินดา และคณะ. (2560). แนวทางเวชปฏิบัติสำหรับโรคเบาหวาน 2560. ปทุมธานี: ร่มเย็น มีเดีย.
วนิรันตา ไชยพาน, สุจิตรา บุญกล้า, กฤษกร คนหาญ และเนตรชนก ไชยพาน. (2564). คู่มือกระบวนการสร้างความรอบรู้ด้านสุขภาพในการป้องกันควบคุมโรคและภัยสุขภาพ. นนทบุรี: สำนักสื่อสารความเสี่ยงและพัฒนาพฤติกรรมสุขภาพ กรมควบคุมโรค กระทรวงสาธารณสุข.
สำนักคณะกรรมการผู้ทรงคุณวุฒิ กรมอนามัย. (2565). กรอบการส่งเสริมความรอบรู้ทางสุขภาพสำหรับหญิงที่เป็นเบาหวานในระยะตั้งครรภ์. สืบค้นเมื่อ 20 ธันวาคม 2567 จาก https://shorturl.asia/6j4Yq.
Baharvand, P., Khatereh, A., & Masoud, A. (2022) Health literacy and its predictors among pregnant women: A cross-sectional study. Journal of Education and Community Health, 9(3), 170-175. https://doi.org/10.34172/jech.2022.25
Breuing, J., et al. (2021). Communication strategies in the prevention of type 2 diabetes and gestational diabetes in vulnerable groups: A scoping review. Systematic Reviews, 10, 1-17. https://doi.org/10.1186/s13643-021-01846-8.
Conard, S. (2019). Best practices in digital health literacy. International Journal of Cardiology, 292, 277-279. https://doi.org/10.1016/j.ijcard.2019.05.070
Dunn, P., & Hazzard, E. (2019). Technology approaches to digital health literacy. International Journal of Cardiology, 293, 294-296. https://doi.org/10.1016/j.ijcard.2019.06.039
Eumbunnapong, K., Wannapiroon, P., & Pornpongtechavanich, P. (2022). An intelligent digital learning platform to enhance digital health literacy. International Journal of Emerging Technologies in Learning, 17(4), 95-111. https://doi.org/10.3991/ijet.v17i04.27907
Farmanova, E., Luc, B., & Louise, B. (2018). Organizational health literacy: Review of theories, frameworks, guides, and implementation issues. INQUIRY. The Journal of Health Care, 55, 46958018757848. https://doi.org/10.1177/0046958018757848
Gharachourlo, M., Mahmoodi, Z., Kamrani, M. K., Tehranizadeh, M., & Kabir, K. (2018). The effect of a health literacy approach to counselling on the lifestyle of women with gestational diabetes: A clinical trial. F1000 Research, 7, 282. https://doi.org/10.12688/f1000research.13838.1
International Diabetes Federation. (2023). Gestational Diabetes. Retrived October 30, 2023 from http://idf.org/about- diabetes/gestational-diabetes/.
Karavasileiadou, S., Almegwely, W., Alanazi, A., Alyami, H., & Chatzimichailidou, S. (2022). Self-management and self-efficacy of women with gestational diabetes mellitus: A systematic review. Global Health Action, 15(1), 2087298. https://doi.org/10.1080/16549716.2022.2087298
Leblalta, B., Kebaili, H., Sim, R., & Lee, S. W. H. (2022). Digital health interventions for gestational diabetes mellitus: A systematic review and meta-analysis of randomised controlled trials. PLOS Digital Health, 1(2), e0000015. https://doi.org/10.1371/journal.pdig.0000015
Lloyd, J. E., Song, H. J., Dennis, S. M., Dunbar, N., Harris, E., & Harris, M. S. (2018). A paucity of strategies for developing health literate organizations: A systematic review. PLoS One, 13(4) 10-23. https://doi.org/10.1371/journal.pone.0195018
Martis, R., Brown, J., McAra-Couper, J., & Crowther, C. A. (2018). Enablers and barriers for women with gestational diabetes mellitus to achieve optimal glycaemic control - a qualitative study using the theoretical domains framework. BMC Pregnancy and Childbirth, 18(1), 91. https://doi.org/10.1186/s12884-018-1710-8
Meldgaard, M., Mads, G., & Helle, T. M. (2022). Health literacy in the prenatal phase: A systematic review. Sexual & Reproductive Healthcare, 15, 58-69. https://doi.org/10.1016/j.srhc.2022.100796
Mensah, G. P., Ten Ham-Baloyi, W., van Rooyen, D. R. M., & Jardien-Baboo, S. (2019). Guidelines for the nursing management of gestational diabetes mellitus: An integrative literature review. Nursing Open, 7(1), 78-90. https://doi.org/10.1002/nop2.324
Nejati, S., Törnbom, K., Hange, D., Björkelund, C., & Svenningsson, I. (2023). How can care managers strengthen health literacy among patients with common mental disorders? A qualitative study. Scandinavian Journal of Caring Sciences, 37(3), 842-850. https://doi.org/10.1111/scs.13170
Nesari, M., Olson, J. K., Nasrabadi, A. N., & Norris, C. (2019). Registered nurses' knowledge of and experience with health literacy. Health Literacy Research and Practice, 3(4), e268-e279. https://doi.org/10.3928/24748307-20191021-01
Nielsen, K., et al. (2020). Protocol for a randomized controlled trial of a co-produced, complex, health promotion intervention for women with prior gestational diabetes and their families: The Face-It Study. Trials, 21(1), 1-128. https://doi.org/10.1186/s13063-020- 4062-4
North, S., Crofts, C., & Caryn, Z. (2022). Health professionals' views and experiences around the dietary and lifestyle management of gestational diabetes in New Zealand. Nutrition & Dietetics, 79(2), 255-264. https://doi.org/10.1111/1747-0080.12719
Nutbeam, D. (2000). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259-267. https://doi.org/10.1093/heapro/15.3.259
Peat, G., Rodriguez, A. & Smith, J. (2019). Interpretive phenomenological analysis applied to healthcare research. Evidence-Based Nursing. 22(1), 7-9. https://doi.org/10.1136/ebnurs-2018-103017
Qutoshi, S. (2018). Phenomenology: A philosophy and method of inquiry. Journal of Education and Educational Development, 5(1), 215-222. https://doi.org/10.22555/JOEED.V5I1.2154
Tuffour, S. (2017). A critical overview of interpretative phenomenological analysis: A contemporary qualitative research approach. Journal of Healthcare Communications, 2(1), 1-3. https://doi.org/10.4172/2472-1654.100093
Wittenberg, E., Ferrell, B., Kanter, E., & Buller, H. (2018). Health literacy: Exploring nursing challenges to providing support and understanding. Clinical Journal of Oncology Nursing, 22(1), 53-61. https://doi.org/10.1188/18.CJON.53-61
Yang, Y. (2022). Effects of health literacy competencies on patient-centered care among nurses. BMC Health Services Research, 22(1), 1172. https://doi.org/10.1186/s12913-022-08550-w
Youngwanichsetha, S. & Sasitorn, P. (2017). Lived experience of blood glucose self-monitoring among pregnant women with gestational diabetes mellitus: Phenomenological research. Journal of Clinical Nursing, 26(19-20), 2915-2921. https://doi.org/10.1111/jocn.13571
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Journal of Nursing and Public Health Research

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
1. บทความหรือข้อคิดเห็นใด ๆ ที่ปรากฏในวารสารวิจัยการพยาบาลและการสาธารณสุข ที่เป็นวรรณกรรมของผู้เขียน บรรณาธิการไม่จำเป็นต้องเห็นด้วย
2. บทความที่ได้รับการตีพิมพ์ถือเป็นลิขสิทธิ์ของ วารสารวิจัยการพยาบาลและการสาธารณสุข








