Clinical outcomes of calcium silicate-based cements with or without calcium chloride as an orthograde apical barrier: a randomised controlled clinical trial
Main Article Content
Abstract
Objective: Calcium chloride has been used as an accelerator to reduce the setting time, dissolution, and leakage of calcium silicate-based cement materials. Its use has increased successful treatment outcomes. The aim of this study was to evaluate and compare the treatment outcomes of two calcium silicate-based cements with or without calcium chloride (Bio-MA or ProRoot® MTA) as orthograde apical barrier materials in teeth with open apices.
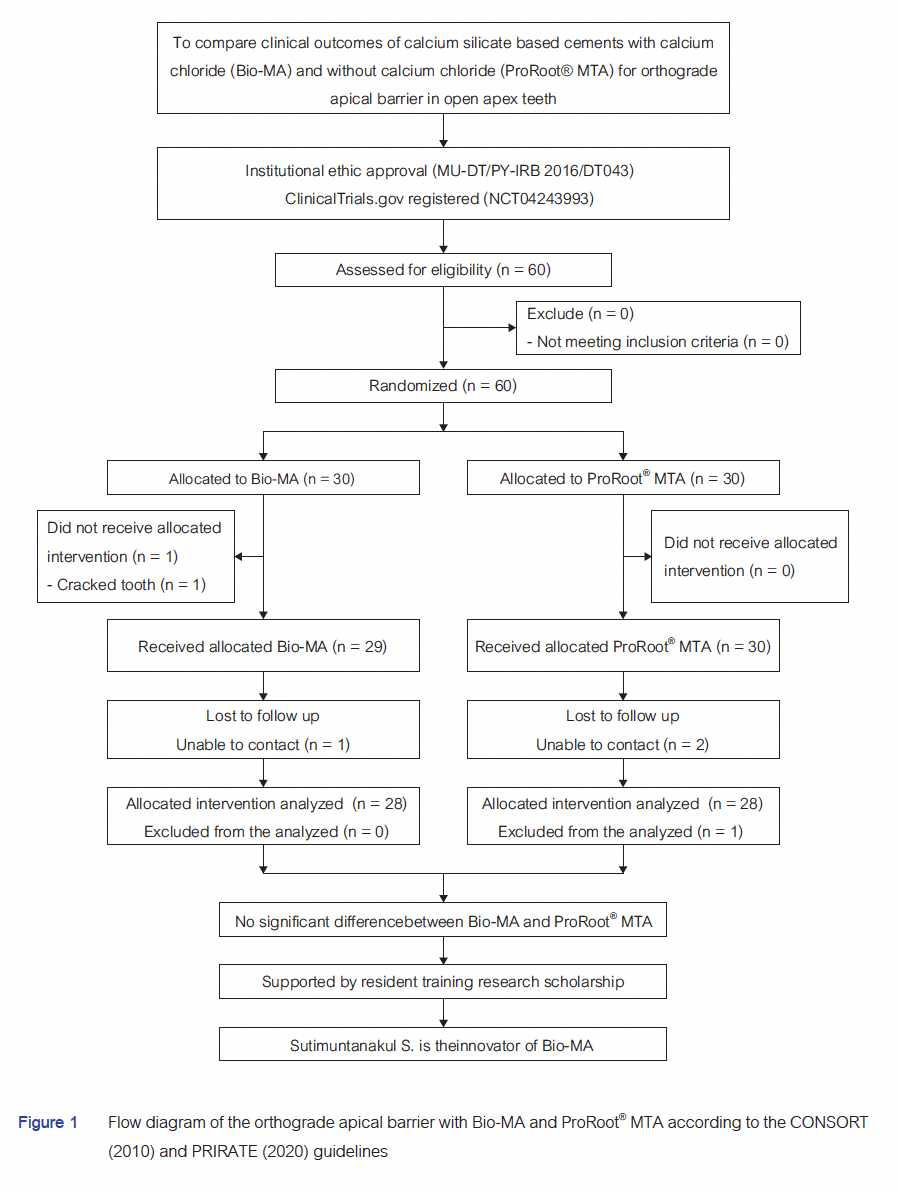
Materials and Methods: Sixty teeth in patients (8–67 years old) were recruited at the Endodontic Clinics of Dental Hospital, Faculty of Dentistry (Phayathai Campus) and Mahachakri Sirindhorn Dental Hospital (Salaya Campus), Mahidol University, Bangkok, Thailand. The teeth were randomly divided into two groups, i.e., Bio-MA or ProRoot® MTA material; the apical barrier was created using standard treatment protocols. Patients were recalled least 6 months after treatment. The treatment outcome was assessed as healed, healing, or disease, based on the clinical and radiographic evaluations. Healed and healing cases were grouped as success. The outcomes of the two materials were analysed and compared using the chi-square test and risk ratio for non-inferiority test.
Results: Fifty-five of 60 teeth, 28 in the Bio-MA group and 27 in the ProRoot® MTA group, were recalled, with a 94.9% recall rate and a median recall period of 17 months (range 6–38 months). Overall, healed and healing cases were 76.4% and 23.6%, respectively with no disease found. The Bio-MA group demonstrated 78.6% healed and 21.4% healing. Whereas, 74.1% healed and 25.9% healing were reported in the ProRoot® MTA group. There was no significant difference in the outcomes between Bio-MA and ProRoot® MTA used as an orthograde apical barrier (p>0.05). The non-inferiority analysis indicated that Bio-MA tended to be non-inferior, but the risk ratio was inconclusive.
Conclusion: Clinical outcomes of calcium silicate-based cements with or without calcium chloride in an orthograde apical barrier were highly successful with no significant difference between the materials.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Rafter M. Apexification: a review. Dent Traumatol. 2005 Feb;21(1):1-8. doi: 10.1111/j.1600-9657.2004.00284.x.
Mente J, Hage N, Pfefferle T, Koch MJ, Dreyhaupt J, Staehle HJ, et al. Mineral trioxide aggregate apical plugs in teeth with open apical foramina: a retrospective analysis of treatment outcome. J Endod. 2009 Oct;35(10):1354-1358. doi: 10.1016/j.joen.2009.05.025.
American Association of Endodontists Special Committee to Revise the Glossary. Glossary of Endodontic Terms: American Association of Endodontists; [Available from: https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms/.
Sheehy EC, Roberts GJ. Use of calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: a review. Br Dent J. 1997 Oct;183(7):241-246. doi: 10.1038/sj.bdj.4809477.
Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin North Am. 2010 Apr;54(2):313-324. doi: 10.1016/j.cden.2009.12.006.
Andreasen JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol. 2006 Jun;22(3):154-156. doi: 10.1111/j.1600-9657.2006.00419.x.
Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review--Part I: chemical, physical, and antibacterial properties. J Endod. 2010 Jan;36(1):16-27. doi: 10.1016/j.joen.2009.09.006.
Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review--part II: leakage and biocompatibility investigations. J Endod. 2010 Feb;36(2):190-202. doi: 10.1016/j.joen.2009.09.010.
Kandemir Demirci G, Kaval ME, Güneri P, Çalışkan MK. Treatment of immature teeth with nonvital pulps in adults: a prospective comparative clinical study comparing MTA with Ca(OH)(2). Int Endod J. 2020 Jan;53(1):5-18. doi: 10.1111/iej.13201.
Chala S, Abouqal R, Rida S. Apexification of immature teeth with calcium hydroxide or mineral trioxide aggregate: systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 Oct;112(4):e36-42. doi: 10.1016/j.tripleo.2011.03.047
Lin JC, Lu JX, Zeng Q, Zhao W, Li WQ, Ling JQ. Comparison of mineral trioxide aggregate and calcium hydroxide for apexification of immature permanent teeth: A systematic review and meta-analysis. J Formos Med Assoc. 2016 Jul;115(7):523-530. doi: 10.1016/j.jfma.2016.01.010.
Chng HK, Islam I, Yap AU, Tong YW, Koh ET. Properties of a new root-end filling material. J Endod. 2005 Sep;31(9):665-668. doi: 10.1097/01.don.0000157993.89164.be.
Settawacharawanich S, Sutimuntanakul S, Phuvaravan S, Plang-ngern S. The chemical compositions and physicochemical properties of a Thai white Portland cement [M.Sc. Project Report]. Mahidol University; 2006.
Warotamawichaya S, Sutimuntanakul S. Effect of calcium chloride on setting time of Thai white Portland cement [Postgraduated Project Report]. Mahidol University; 2011.
Kongpreecha T, Sutimuntanakul S. Cytotoxicity evaluation of Thai white Portland Cement with setting accelerator using MTT assay [Postgraduated Project Report]. Mahidol University; 2015.
Karnchanawarut Y, Sutimuntanakul S. Microleakage of 3 formulae of Thai white Portland cement and MTA when used as retrograde material [M.Sc. Project Report]. Mahidol University; 2009.
Saratta P, Sutimuntanakul S, Srisatjaluk R. Apical leakage of white Portland cement added with different amount of calcium chloride [Postgraduated Project Report]. Mahidol University; 2013.
Pisalchaiyong N, Sutimuntanakul S, Korsuwannawong S, Vajrabhaya L. Evaluating cytotoxicity of Thai white Portland cement in cell culture using MTT assay. M Dent J. 2010(30):17-26.
Chaimanakarn C, Sutimuntanakul S, Jantarat J. Subcutaneous tissue response to calcium silicate-based cement [M.Sc. Project Report]. Mahidol University; 2014.
Trongkij P, Sutimuntanakul S, Lapthanasupkul P, Chaimanakarn C, Wong R, Banomyong D. Effects of the exposure site on histological pulpal responses after direct capping with 2 calcium-silicate based cements in a rat model. Restor Dent Endod. 2018 Aug;43(4):e36. doi: 10.5395/rde.2018.43.e36.
Bortoluzzi EA, Broon NJ, Bramante CM, Felippe WT, Tanomaru Filho M, Esberard RM. The influence of calcium chloride on the setting time, solubility, disintegration, and pH of mineral trioxide aggregate and white Portland cement with a radiopacifier. J Endod. 2009 Apr;35(4):550-554. doi: 10.1016/j.joen.2008.12.018.
Tungsuksomboon N, Sutimuntanakul S, Banomyong D. Clinical outcomes of Bio-MA and ProRoot® MTA in orthograde apical barrier and root perforation repair: a preliminary phase of randomized controlled trial study. M Dent J. 2021;41(1):19-34.
Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010 Mar;8:18. doi: 10.1186/1741-7015-8-18.
Nagendrababu V, Duncan HF, Bjørndal L, Kvist T, Priya E, Jayaraman J, et al. PRIRATE 2020 guidelines for reporting randomized trials in Endodontics: a consensus-based development. Int Endod J. 2020 Jun;53(6):764-773. doi: 10.1111/iej.13294.
Song M, Kim E. A prospective randomized controlled study of mineral trioxide aggregate and super ethoxy-benzoic acid as root-end filling materials in endodontic microsurgery. J Endod. 2012 Jul;38(7):875-879. doi: 10.1016/j.joen.2012.04.008.
Friedman S, Mor C. The success of endodontic therapy--healing and functionality. J Calif Dent Assoc. 2004 Jun;32(6):493-503.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. Mar 1977;33(1):159-174.
Mente J, Leo M, Panagidis D, Ohle M, Schneider S, Lorenzo Bermejo J, et al. Treatment outcome of mineral trioxide aggregate in open apex teeth. J Endod. 2013 Jan;39(1):20-26. doi: 10.1016/j.joen.2012.10.007.
Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod. 2012 Oct;38(10):1330-1336. doi: 10.1016/j.joen.2012.06.028
Berman LH, Kuttler S. Fracture necrosis: diagnosis, prognosis assessment, and treatment recommendations. J Endod. 2010 Mar;36(3):442-446. doi: 10.1016/j.joen.2009.12.018.
Lertmalapong P, Jantarat J, Srisatjaluk RL, Komoltri C. Bacterial leakage and marginal adaptation of various bioceramics as apical plug in open apex model. J Investig Clin Dent. 2019 Feb;10(1):e12371. doi: 10.1111/jicd.12371.
Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995 Jul;21(7):349-353. doi: 10.1016/S0099-2399(06)80967-2.
Darvell BW, Wu RC. "MTA"-an Hydraulic Silicate Cement: review update and setting reaction. Dent Mater. 2011 May;27(5):407-422. doi: 10.1016/j.dental.2011.02.001.
Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical study. Endod Dent Traumatol. 1992 Apr;8(2):45-55. doi: 10.1111/j.1600-9657.1992.tb00228.x.
Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002 Jun;18(3):134-137. doi: 10.1034/j.1600-9657.2002.00097.x.
Pradhan DP, Chawla HS, Gauba K, Goyal A. Comparative evaluation of endodontic management of teeth with unformed apices with mineral trioxide aggregate and calcium hydroxide. J Dent Child (Chic). 2006 May-Aug;73(2):79-85.
Kratchman SI. Perforation repair and one-step apexification procedures. Dent Clin North Am. 2004 Jan;48(1):291-307. doi: 10.1016/j.cden.2003.12.003.
Camilleri J, Pitt Ford TR. Mineral trioxide aggregate: a review of the constituents and biological properties of the material. Int Endod J. 2006 Oct;39(10):747-754. doi: 10.1111/j.1365-2591.2006.01135.x.
Shabahang S, Torabinejad M, Boyne PP, Abedi H, McMillan P. A comparative study of root-end induction using osteogenic protein-1, calcium hydroxide, and mineral trioxide aggregate in dogs. J Endod. 1999 Jan;25(1):1-5. doi: 10.1016/S0099-2399(99)80388-4.
Orstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J. 1996 May;29(3):150-155. doi: 10.1111/j.1365-2591.1996.tb01361.x.