Effect of threshold configuration on accuracy in upper airway analysis using cone-beam computed tomography
Main Article Content
Abstract
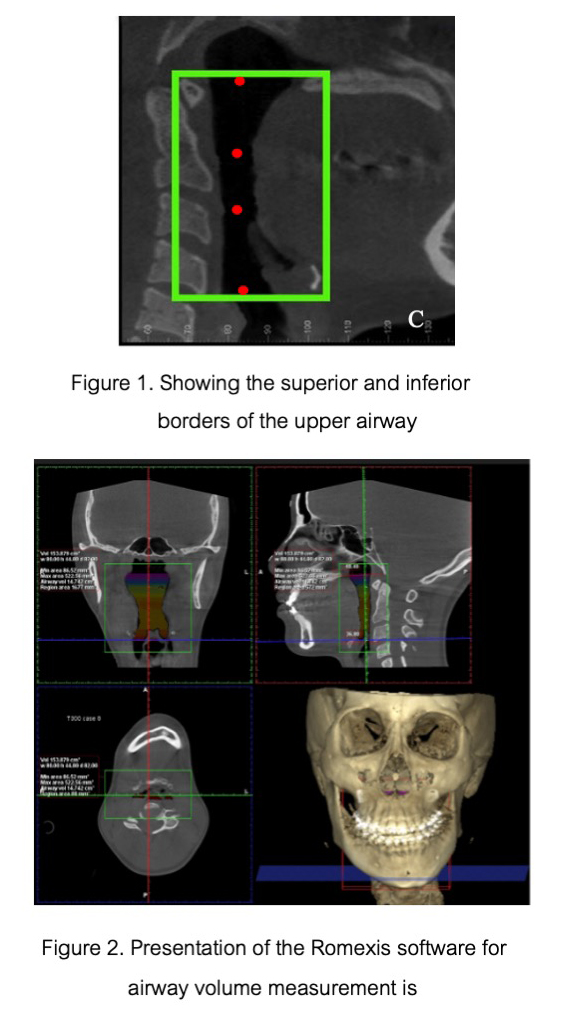
Objective: To determine the optimal threshold of Romexis software for the airway volume and minimum cross-sectional area (MCA) analysis using image J as a gold standard.
Materials and Methods: A total of ten CBCT images were collected. The airway volume and MCA of each patient were analyzed using the automatic airway segmentation function in the CBCT DICOM viewer (Romexis). Airway volume and MCA measurements were conducted on each CBCT sagittal view with fifteen different threshold values from the Romexis software, ranging from 300 to 1000. Duplicate DICOM files, in axial view, were imported into ImageJ for concurrent airway volume and MCA analysis as the gold standard. The airway volume and MCA measured from Romexis and ImageJ were compared using a t-test with Bonferroni correctio, and statistical significance was set at p<0.003.
Results: Concerning airway volume, thresholds of 600 to 850, as well as 1000, exhibited results that were not significantly distinct from those obtained through ImageJ. Regarding MCA, employing thresholds from 400 to 850 within Romexis Viewer showed no variance from ImageJ. Notably, within the threshold range of 600 to 850, there were no statistically significant differences observed in both airway volume and MCA analyses, in comparison to ImageJ.
Conclusion: This study demonstrates that the utilization of Planmeca Romexis Viewer 6.4.3.3. within the threshold range of 600 to 850 yields airway volume and MCA measurements that exhibit no statistically significant variance in comparison to measurements obtained through ImageJ. This outcome holds implications for diagnosing upper airway obstructions and post-orthodontic surgical monitoring.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Strohl KP, Butler JP, Malhotra A. Mechanical properties of the upper airway. Compr Physiol. 2012 Jul;2(3):1853-72. doi:10.1002/cphy.c110053.
Schwab RJ, Goldberg AN. Upper airway assessment: radiographic and other imaging techniques. Otolaryngol Clin North Am. 1998 Dec;31(6):931-68. doi: 10.1016/s0030-6665(05)70100-6.
Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffman EA, Pack AI. Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med. 1995 Nov;152(5 Pt 1):1673-89. doi: 10.1164/ajrccm.152.5.7582313.
van Lunteren E. Muscles of the pharynx: structural and contractile properties. Ear nose Throat J .1993 Jan;72(1):27-29, 33.
El H, Palomo JM. Measuring the airway in 3 dimensions: a reliability and accuracy study. Am J Orthod Dentofacial Orthop. 2010 Apr;137(4 Suppl):S50 e1-9; discussion S50-S52. doi: 10.1016/j.ajodo.2010.01.014.
Abbott MB, Donnelly LF, Dardzinski BJ, Poe SA, Chini BA, Amin RS. Obstructive sleep apnea: MR imaging volume segmentation analysis. Radiol. 2004 Sep;232(3):889-895. doi:10.1148/radiol.2323031581.
Donnelly LF, Surdulescu V, Chini BA, Casper KA, Poe SA, Amin RS. Upper airway motion depicted at cine MR imaging performed during sleep: comparison between young Patients with and those without obstructive sleep apnea. Radiol. 2003 Apr;227(1):239-245. doi:10.1148/radiol.2271020198.
Guilleminault C, Hill MH, Simmons FB, Powell N, Riley R, Stoohs R. Passive constriction of the upper airway during central apneas: fiberoptic and EMG investigations. Respir Physiol. 1997 Apr;108(1):11-22. doi: 10.1016/s0034-5687(97)02529-2.
Armstrong JJ, Leigh MS, Sampson DD, Walsh JH, Hillman DR, Eastwood PR. Quantitative upper airway imaging with anatomic optical coherence tomography. Am J Respir Crit Care Med. 2006 Jan;173(2):226-33. doi: 10.1164/rccm.200507-1148OC.
Guijarro-Martinez R, Swennen GR. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011 Nov;40(11):1227-1237. doi: 10.1016/j.ijom.2011.06.017.
Zimmerman JN, Lee J, Pliska BT. Reliability of upper pharyngeal airway assessment using dental CBCT: a systematic review. Eur J Orthod. 2017 Oct;39(5):489-496. doi: 10.1093/ejo/cjw079.
Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009 Apr;135(4):468-479.doi:10.1016/j.ajodo.2007.04.043.
Yamashina A, Tanimoto K, Sutthiprapaporn P, Hayakawa Y. The reliability of computed tomography (CT) values and dimensional measurements of the oropharyngeal region using cone beam CT: comparison with multidetector CT. Dentomaxillofac Radiol. 2008 Jul;37(5):245-251. doi: 10.1259/dmfr/45926904.
Kamaruddin N, Daud F, Yusof A, Aziz ME, Rajion ZA. Comparison of automatic airway analysis function of Invivo5 and Romexis software. PeerJ. 2019 Jan;7:e6319. doi: 10.7717/peerj.6319.
Haskell JA, McCrillis J, M, Haskell BS, Scheetz JP, Scarfe WC, Farman AG. Effects of mandibular advancement device (MAD) on airway dimensions assessed with cone-beam computed tomography. Semin Orthod. 2009 Jun;15(2):132-158.
Zinsly SR, Moraes LC, Moura P, Ursi W. Assessment of pharyngeal airway space using Cone-Beam Computed Tomography. Dental Press J Orthod. 2010 Sep-Oct;15(5):150-158.
Alves M, Jr., Baratieri C, Nojima LI, Nojima MC, Ruellas AC. Three-dimensional assessment of pharyngeal airway in nasal- and mouth-breathing children. Int J Pediatr Otorhinolaryngol. 2011 Sep;75(9):1195-1199. doi: 10.1016/j.ijporl.2011.06.019.
Alves M, Jr., Baratieri C, Mattos CT, Brunetto D, Fontes Rda C, Santos JR, et al. Is the airway volume being correctly analyzed?.Am J Orthod Dentofacial Orthop. 2012 May;141(5):657-661. doi:10.1016/j.ajodo.2011.11.019.
Chow SC, Shao J, Wang H. (2003). Sample size calculations in clinical research (2nd ed.). Chapman & Hall/CRC., 51 P.
Ngamjarus C., Chongsuvivatwong V. (2014). n4Studies: Sample size and power calculations for ios. The Royal Golden Jubilee Ph.D Program - The Thailand Research Fund&Prince of Songkla University.
Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nature Methods. 2012 Jul;9(7):671-5. doi:10.1038/nmeth.2089.
Fadili A, Alehyane N, Halimi A., ZaouiF. An alternative approach to assessing volume-of-interest accuracy using CBCT and ImageJ software: In vitro study. Hindawi Publishing Corporation. Adv Radiol. 2015;2015:329720. doi: 10.1155/2015/329720.
Lenza MG, Lenza de O. MM, Dalstra M, Melsen B, Cattaneo PM: An analysis of different approaches to the assessment of upper airway morphology: a CBCT study. Orthod Craniofac Res. 2010 May;13(2):96–105. doi: 10.1111/j.1601-6343.2010.01482.x.
Ghoneima A, Kula K. Accuracy and reliability of cone-beam computed tomography for airway volume analysis. Eur J Orthod. 2013 Apr;35(2):256–261. doi: 10.1093/ejo/cjr099.
Alsufyani N, Noga ML, Witmans M, Major P. Upper airway imaging in sleep-disordered breathing: role of cone-beam computed tomography. Oral Radiol. 2017 Mar;33(3):161–169. doi:10.1007/s11282-017-0280-1.