Efficacy of curcuminoids on postoperative pain control after third molar surgery: multicenter double-blind randomized control trial
Main Article Content
Abstract
Objective: To compare the efficacy of turmeric extract (curcuminoids) to ibuprofen on postoperative pain control after lower third molar surgery.
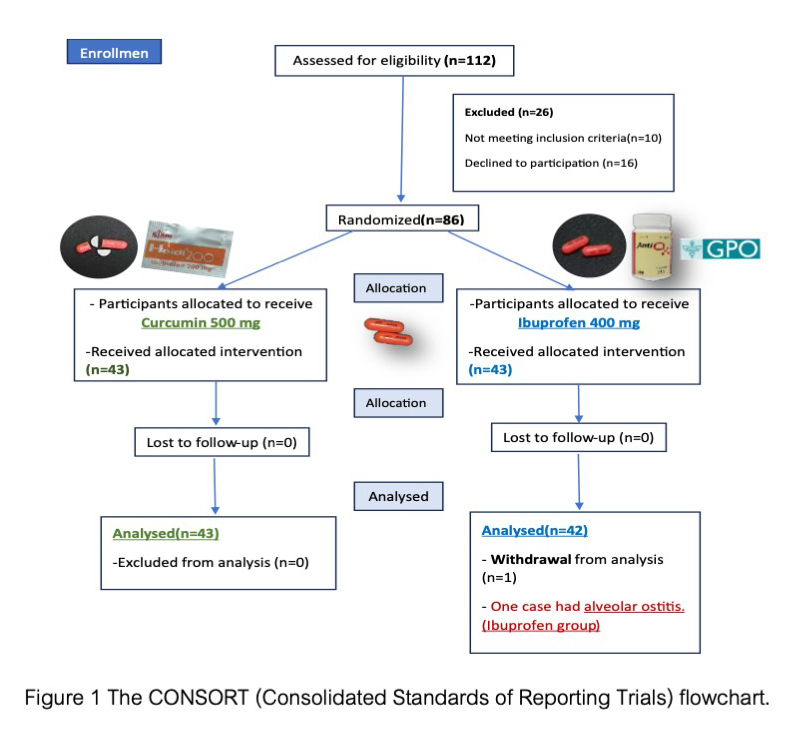
Materials and Methods: Eighty-six patients requiring lower third-molar surgery with moderate difficulty from three centers were randomly assigned to two groups: one receiving 500 mg of curcuminoids and the other 400 mg of ibuprofen three times daily for three days. Pain intensity was assessed using a visual analog scale (VAS) at 1, 2, 6, 12, 24, 48, 72 hours, and 7 days after surgery. If necessary, the rescue analgesic drug was paracetamol 325 mg with tramadol 37.5 mg. Statistical analyses were conducted using independent t-tests and the Chi-square test.
Results: There were 43 patients in the curcuminoids group and 43 in the ibuprofen group. One participant in the ibuprofen group withdrew from the study due to severe postoperative pain with alveolar osteitis. The baseline characteristics did not statistically differ between the two groups. At 6 hours post-operation, the mean pain intensity score of the curcuminoids group (5.33±2.71) reached its highest peak, which was statistically significantly higher (p<0.05) than that of the ibuprofen group (2.74±2.06). The highest peak in the ibuprofen group occurred at 2 hours post-operation, with a score of 2.96±2.60. The need for rescue analgesics was significantly higher in the curcuminoids group (32.6%) compared to the ibuprofen group (14.3%) (p<0.05).
Conclusions: The efficacy of pain control in the low dose of turmeric extract (curcuminoids) 1500 mg per day was lower than ibuprofen 1200 mg per day after lower third molar surgery with moderate difficulty levels. The low dose of curcuminoids could be used in tooth extraction and other minor oral surgery with mild pain or in the condition that NSAIDs are not indicated. The higher dose of curcuminoids can be used for proper pain control in further study.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
References
Ayaz H. Post-operative complications associated with impacted mandibular third molar removal. Pak Oral Dental J. 2012 Dec;32(3):389-392.
Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc. 2007 May;73(4):325:325a-325e.
Khan A KU, Khan MT. Mandibular third molars: pattern of presentation and postoperative complications. Pak Oral Dental J. 2010 Dec;30(2):307-312.
Bushra R, Aslam N. An overview of clinical pharmacology of Ibuprofen. Oman Med J. 2010 Jul;25(3):155-161. doi: 10.5001/omj.2010.49.
Priyadarsini KI. The chemistry of curcumin: From extraction to therapeutic agent. Molecules. 2014 Dec;19(12):20091–20112. doi: 10.3390/molecules191220091.
Gupta SC, Patchva S, Aggarwal BB. Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J. 2013 Jan;15(1):195–218. doi: 10.1208/s12248-012-9432-8.
Lestari ML, Indrayanto G. Curcumin. Profiles Drug Subst Excip Relat Methodol. 2014 May;39:113–204. doi: 10.1016/B978-0-12-800173-8.00003-9.
Mahady GB, Pendland SL, Yun G, Lu ZZ. Turmeric (Curcuma longa) and curcumin inhibit the growth of Helicobacter pylori, a group 1 carcinogen. Anticancer Res. 2002 Nov-Dec;22(6C):4179–4181.
Reddy RC, Vatsala PG, Keshamouni VG, Padmanaban G, Rangarajan PN. Curcumin for malaria therapy. Biochem Biophys Res Commun. 2005 Jan;326(2):472–474. doi: 10.1016/j.bbrc.2004.11.051.
Wright LE, Frye JB, Gorti B, Timmermann BN, Funk JL. Bioactivity of turmeric-derived curcuminoids and related metabolites in breast cancer. Curr Pharm Des. 2013;19(34): 6218–6225. doi: 10.2174/1381612811319340013.
Phoolcharoen N, Oranratanaphan S, Ariyasriwatana C, Worasethsin P. Efficacy of curcuminoids for reducing postoperative pain after laparoscopic gynecologic surgery: A pilot randomized trial. J Complement Integr Med. 2019 May;16(4):0224-0229. doi: 10.1515/jcim-2018-0224.
Huang MT, Lysz T, Ferraro T, Abidi TF, Laskin JD, Conney AH. Inhibitory effects of curcumin on in vitro lipoxygenase and cyclooxygenase activities in mouse epidermis. Cancer Res.1991 Feb;51(3):813–819.
Lantero A, Tramullas M, Díaz A, Hurlé MA. Transforming growth factor-beta in normal nociceptive processing and pathological pain models. Mol Neurobiol. 2012 Feb;45(1):76–86. doi: 10.1007/s12035-011-8221-1.
He Y, Yue Y, Zheng X, Zhang K, Chen S, Du Z. Curcumin, inflammation, and chronic diseases: how are they linked? Molecules. 2015 May;20(5):9183-9213. doi: 10.3390/molecules20059183.
Koeberle A, Werz O. Multi-target approach for natural products in inflammation. Drug Discov Today. 2014 Dec;19(12):1871-1882. doi: 10.1016/j.drudis.2014.08.006.
Maulina T, Diana H, Cahyanto A, Amaliya A. The efficacy of curcumin in managing acute inflammation pain on the post-surgical removal of impacted third molars patients: A randomised controlled trial. J Oral Rehabil. 2018 Sep;45(9):677-683. doi: 10.1111/joor.12679.
Yoysungnoen-Chintana P, Bhattarakosol P, Patumraj S. Antitumor and antiangiogenic activities of curcumin in cervical cancer xenografts in nude mice. Biomed Res Int. 2014;2014:817972. doi: 10.1155/2014/817972.
Nurullahoglu KE, Okudan N, Belviranli M, Oz M. The comparison of preemptive analgesic effects of curcumin and diclofenac. Bratisl Lek Listy. 2014;115(12):757–760. doi: 10.4149/bll_2014_146.
Nagaraju GP, Zhu S, Ko JE, Ashritha N, Kandimalla R, Snyder JP, et al. Antiangiogenic effects of a novel synthetic curcumin analog in pancreatic cancer. Cancer Lett. 2015 Feb;357(2):557-565. doi: 10.1016/j.canlet.2014.12.007.
Chainani-Wu N. Safety and anti-inflammatory activity of curcumin: a component of tumeric (Curcuma longa). J Altern Complement Med. 2003 Feb;9(1):161-168. doi: 10.1089/107555303321223035.
Kuptniratsaikul V, Thanakhumtorn S, Chinswangwatanakul P, Wattanamongkonsil L, Thamlikitkul V. Efficacy and safety of curcuma domestica extracts in patients with knee osteoarthritis. J Altern Complement Med. 2009 Aug;15(8):891-897. doi: 10.1089/acm.2008.0186.
Daily JW, Yang M, Park S. Efficacy of turmeric extracts and curcumin for alleviating the symptoms of ioint arthritis: A Systematic review and meta-analysis of randomized clinical trials. J Med Food. 2016 Aug;19(8):717–729. doi: 10.1089/jmf.2016.3705.
Chandran B, Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother Res. 2012 Nov;26(11):1719-1725. doi: 10.1002/ptr.4639.
Kuptniratsaikul V, Dajpratham P, Taechaarpornkul W, Buntragulpoontawee M, Lukkanapichonchut P, Chootip C, et al. Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: a multicenter study. Clin Interv Aging. 2014 Mar;9:451-458. doi: 10.2147/CIA.S58535.
Kim JC, Choi SS, Wang SJ, Kim SG. Minor complications after mandibular third molar surgery: type, incidence, and possible prevention. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Aug;102(2):e4-11. doi: 10.1016/j.tripleo.2005.10.050.
Isola G, Matarese M, Ramaglia L, Iorio-Siciliano V, Cordasco G, Matarese G. Efficacy of a drug composed of herbal extracts on postoperative discomfort after surgical removal of impacted mandibular third molar: a randomized, triple-blind, controlled clinical trial. Clin Oral Investig. 2019 May;23(5):2443-2453. doi: 10.1007/s00784-018-2690-9.
Nørholt SE, Aagaard E, Svensson P, Sindet-Pedersen S. Evaluation of trismus, bite force, and pressure algometry after third molar surgery: a placebo-controlled study of ibuprofen. J Oral Maxillofac Surg. 1998 Apr;56(4):420-427; discussion 427-429. doi: 10.1016/s0278-2391(98)90705-4.
Fisher SE, Frame JW, Rout PG, McEntegart DJ. Factors affecting the onset and severity of pain following the surgical removal of unilateral impacted mandibular third molar teeth. Br Dent J. 1988 Jun;164(11):351-354. doi: 10.1038/sj.bdj.4806453.
Di Pierro F, Rapacioli G, Di Maio EA, Appendino G, Franceschi F, Togni S. Comparative evaluation of the pain-relieving properties of a lecithinized formulation of curcumin (Meriva®), nimesulide, and acetaminophen. J Pain Res. 2013 Mar;6:201-205. doi: 10.2147/JPR.S42184.
Agarwal KA, Tripathi CD, Agarwal BB, Saluja S. Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study. Surg Endosc. 2011 Dec;25(12):3805-3810. doi: 10.1007/s00464-011-1793-z.
Fransen M, Bridgett L, March L, Hoy D, Penserga E, Brooks P. The epidemiology of osteoarthritis in Asia. Int J Rheum Dis. 2011 May;14(2):113-121. doi: 10.1111/j.1756-185X.2011.01608.x.
Moore PA, Hersh EV. Celecoxib and rofecoxib. The role of COX-2 inhibitors in dental practice. J Am Dent Assoc. 2001 Apr;132(4):451-456. doi: 10.14219/jada.archive.2001.0207.