Comprehensive geriatric assessment for oral health care: a perspective from non-dental health professionals
Main Article Content
Abstract
Objective: To describe the opinions from healthcare professionals on the comprehensive geriatric assessment for Thai dentists to provide oral health care in older adults and special needs patients.
Materials and Methods: A literature review was conducted to describe common medical conditions associated with older adults and appropriate assessment methods used by multidisciplinary healthcare professions. Expert opinions of multiple medical professions were collected by a focus group. Data were captured via audio/visual recordings, analyzed using content and thematic analysis, and reported.
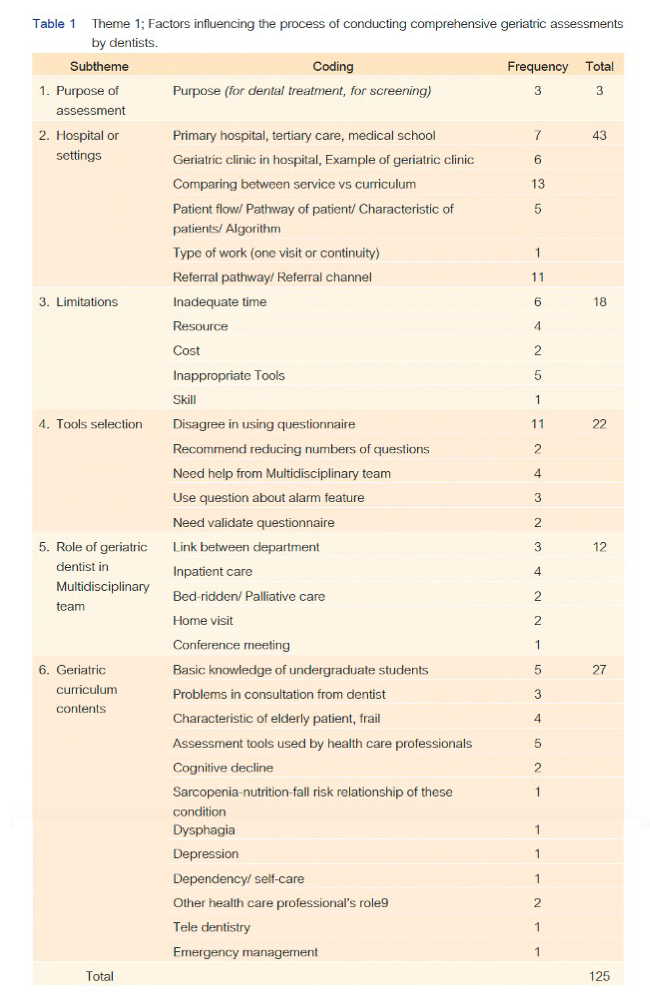
Results: Time and other resources were mentioned as limitations for solving older adults’ health problems. Dentists as a part of the multidisciplinary team should be aware of the unique needs of older patients and familiarize themselves with geriatric conditions and assessment tools. Key factors such as patient profiles, dependency levels, social support, family history, comorbidities, and medications must be properly considered. Multidisciplinary collaboration is crucial to support healthcare professionals for holistic care. To facilitate the referral process, initial assessments should be conducted by targeted questions to differentiate patients’ problems and direct patients to the specialized care they need. Consideration of urgency and context-specific referral channels is important. Mental health can be assessed using simple questions, and specific tools or questions can be employed to evaluate dysphagia, malnutrition, and fall risk. Comprehensive cognitive assessments may not be essential, but an evaluation of decision-making capacity is important for dental professionals.
Conclusion: The findings provide key considerations for comprehensive assessment in older adults, and emphasize the importance of multidisciplinary team collaboration, context-specific referral channels, and essential tools in patient assessments.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
World population ageing 1950-2050. 2002, UN: New York :.
Petersen, P.E., et al. Global oral health of older people--call for public health action. Community Dent Health. 2010 Dec;27(4 Suppl 2):257-67. doi: 10.1922/CDH_2711Petersen11.
Berkey, D.B. and F.A. Scannapieco. Medical considerations relating to the oral health of older adults. Spec Care Dentist. 2013 Jul-Aug;33(4):164-76. doi: 10.1111/scd.12027.
Presley, C.J., et al. Implementing a multidisciplinary approach for older adults with Cancer: geriatric oncology in practice. BMC Geriatr. 2020 2020/07/06;20(1):231. doi: 10.1186/s12877-020-01625-5.
Nitschke, I., et al. On the Necessity of a Geriatric Oral Health Care Transition Model: Towards an Inclusive and Resource-Oriented Transition Process. IRJPEH. 2022 19(10):6148. doi: 10.3390/ijerph19106148.
Parker, S.G., et al. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing. 2018 Jan 1;47(1):149-155. doi: 10.1093/ageing/afx166.
รายงานผลการสำรวจสภาวะสุขภาพช่องปากแห่งชาติ ครั้งที่ 8 ประเทศไทย พ.ศ. 2560.--นนทบุรี :
สำนักทันตสาธารณสุข กรมอนามัย กระทรวงสาธารณสุข, 2561.
Glaser, B.G. and A.L. Strauss, The Discovery of Grounded Theory: Strategies for Qualitative Research. 1967: Aldine Transaction.
Strauss, A. and J.M. Corbin, Basics of qualitative research: Grounded theory procedures and techniques. Basics of qualitative research: Grounded theory procedures and techniques. 1990, Thousand Oaks, CA, US: Sage Publications, Inc. 270-270.
Ettinger, R.L. Rational dental care: part 1. Has the concept changed in 20 years? J Can Dent Assoc. 2006 Jun;72(5):441-5.
Marchini, L. and R.L. Ettinger. The Prevention, Diagnosis, and Treatment of Rapid Oral Health Deterioration (ROHD) among Older Adults. J Clin Med. 2023 Mar 28;12(7). doi: 10.3390/jcm12072559.
Pretty, I.A., et al. The Seattle Care Pathway for securing oral health in older patients. Gerodontology. 2014 Feb;31 Suppl 177-87. doi: 10.1111/ger.12098.
Ettinger, R.L. Treatment planning concepts for the ageing patient. Aust Dent J. 2015 Mar;60 Suppl 171-85. doi: 10.1111/adj.12286.
Zeng, L.N., et al. Oral health in patients with dementia: A meta-analysis of comparative and observational studies. Int J Geriatr Psychiatry. 2021 Apr;36(4):467-478. doi: 10.1002/gps.5453.
Cademartori, M.G., et al. Is depression associated with oral health outcomes in adults and elders? A systematic review and meta-analysis. Clin Oral Investig. 2018 Nov;22(8):2685-2702. doi: 10.1007/s00784-018-2611-y.
Chen, X. and J.J. Clark. Assessment of dentally related functional competency for older adults with cognitive impairment--a survey for special-care dental professionals. Spec Care Dentist. 2013 Mar-Apr;33(2):48-55. doi: 10.1111/scd.12005.
Nitschke, I., et al. Considerations for the Prosthetic Dental Treatment of Geriatric Patients in Germany. J Clin Med. 2021 Jan 15;10(2). doi: 10.3390/jcm10020304.
Chávez, E.M., et al. Dental Care for Geriatric and Special Needs Populations. Dent Clin North Am. 2018 Apr;62(2):245-267. doi: 10.1016/j.cden.2017.11.005.
Weinstock, R.J. and M.P. Johnson. Review of Top 10 Prescribed Drugs and Their Interaction with Dental Treatment. Dent Clin North Am. 2016 Apr;60(2):421-34. doi: 10.1016/j.cden.2015.11.005.
Margaix Muñoz, M., et al. Cardiovascular diseases in dental practice. Practical considerations. Med Oral Patol Oral Cir Bucal. 2008 May 1;13(5):E296-302.
Teoh, L., G. Moses, and M.J. McCullough. A review of drugs that contribute to bleeding risk in general dental practice. Aust Dent J. 2020 2020/06/01;65(2):118-130. doi: 10.1111/adj.12751.
Di Fede, O., et al. The Dental Management of Patients at Risk of Medication-Related Osteonecrosis of the Jaw: New Paradigm of Primary Prevention. Biomed Res Int. 2018 20182684924. doi: 10.1155/2018/2684924.
Das, P. and S. Challacombe. Dry Mouth and Clinical Oral Dryness Scoring Systems. Prim Dent J. 2016 02/01;577-79. doi: 10.1177/205016841600500110.
Villa, A., et al. World Workshop on Oral Medicine VI: a systematic review of medication-induced salivary gland dysfunction: prevalence, diagnosis, and treatment. Clin Oral Investig. 2015 2015/09/01;19(7):1563-1580. doi: 10.1007/s00784-015-1488-2.
Awano, S., et al. Oral Health and Mortality Risk from Pneumonia in the Elderly. J Dent Res. 2008 05/01;87334-9. doi: 10.1177/154405910808700418.
Cao, J., et al. Factors associated with death in bedridden patients in China: A longitudinal study. PLoS One. 2020 15(1):e0228423. doi: 10.1371/journal.pone.0228423.
van der Maarel-Wierink, C.D., et al. Meta-analysis of dysphagia and aspiration pneumonia in frail elders. J Dent Res. 2011 Dec;90(12):1398-404. doi: 10.1177/0022034511422909.
Fávaro-Moreira, N.C., et al. Risk Factors for Malnutrition in Older Adults: A Systematic Review of the Literature Based on Longitudinal Data. Adv Nutr. 2016 May;7(3):507-22. doi: 10.3945/an.115.011254.
Logemann, J.A., et al. Aging effects on oropharyngeal swallow and the role of dental care in oropharyngeal dysphagia. Oral Dis. 2013 Nov;19(8):733-7. doi: 10.1111/odi.12104.
Walsh, K., J. Roberts, and G. Bennett. Mobility in old age. Gerodontology. 1999 Dec;16(2):69-74. doi: 10.1111/j.1741-2358.1999.00069.x.
Hatta, K. and K. Ikebe. Association between oral health and sarcopenia: A literature review. J Prosthodont Res. 2021 Jun 30;65(2):131-136. doi: 10.2186/jpr.JPOR_2019_567.
Wiseman, M.A. Palliative care dentistry. Gerodontology. 2000 Jul;17(1):49-51. doi: 10.1111/j.1741-2358.2000.00049.x.
Saini, R., et al. Dental expression and role in palliative treatment. Indian J Palliat Care. 2009 Jan;15(1):26-9. doi: 10.4103/0973-1075.53508.