Correlation between vertical facial configuration and skeletal relapse at different time points after single-jaw BSSO mandibular setback in skeletal class III patients
Main Article Content
Abstract
Objective: To evaluate the correlation between MPA and skeletal stability after mandibular setback surgery in skeletal class III patients at the short-term and long-term post-operative time points.
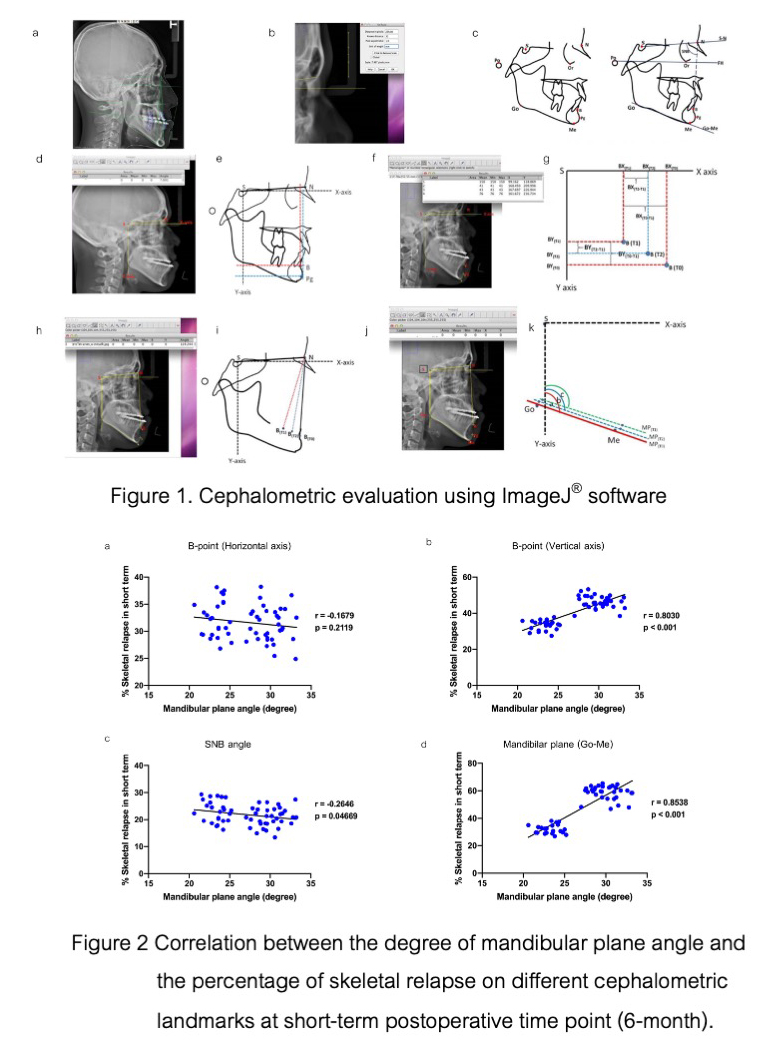
Materials and Methods: Fifty-eight skeletal class III with mandibular prognathism patients who underwent the single-jaw mandibular setback surgery using bilateral sagittal split ramus osteotomy approach were divided into two subgroups based on their vertical skeletal configuration. The subjects were twenty-five patients with normal mandibular plane angle (21.22° ± 4.86°) and thirty-three patients with the high MPA (> 28.06°). To analyze the influence of two facial patterns on post-operative stability, the digital lateral cephalograms were computerized and analyzed on three cephalometric anatomical landmarks including B-point, SNB-angle, and mandibular plane (MP). The correlation between the amount of MPA and the percentage of skeletal relapse was analyzed with the Pearson Correlation Coefficient.
Results: The mean MPA in the hyperdivergent group (30.02° ± 1.65°) was significantly higher than in the normodivergent group (23.65° ± 1.16°). The correlation analysis found that there was a positive correlation between MPA and the percentage of skeletal relapse on the B-point in vertical axis and Mandibular plane (MP) at short-term follow-up. This positive correlation was also further shown on B-point in horizontal axis, SNB-angle, and MP at long-term follow-up.
Conclusions and Relevance: The skeletal relapse after mandibular setback surgery was positively correlated to the mandibular plane angle in skeletal Class III patients. An adjunctive surgical procedure may be needed to achieve the long-term successful outcome after orthognathic surgery in skeletal Class III malocclusion with high MPA.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Yan A, Chen YR. Orthognathic surgery to enhance the smile. Clin Plast Surg. 2023 Jan;50(1):81-89. doi: 10.1016/j.cps.2022.07.001.
Ngan P, Moon W. Evolution of Class III treatment in orthodontics. Am J Orthod Dentofacial Orthop. 2015 Jul;148(1):22-36. doi: 10.1016/j.ajodo.2015.04.012.
Proffit WR, Phillips C, Dann C 4th. Who seeks surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 1990;5(3):153-160.
Mousoulea S, Tsolakis I, Ferdianakis E, Tsolakis AI. The Effect of Chin-cup Therapy in Class III Malocclusion: A Systematic Review. Open Dent J. 2016 Dec;10:664-679. doi: 10.2174/1874210601610010664.
Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy setback surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg. 2008 Aug;66(8):1634-1643. doi: 10.1016/j.joms.2008.01.046.
Cho HJ. Long-Term Stability of Surgical Mandibular Setback. Angle Orthod. 2007 Sep;77(5):851-856. doi: 10.2319/052306-209.1.
Proffit WR, Phillips C, Turvey TA. Stability after surgical-orthodontic corrective of skeletal Class III malocclusion. 3. Combined maxillary and mandibular procedures. Int J Adult Orthodon Orthognath Surg. 1991;6(4):211-225.
Choi TH, Kim SH, Yun PY, Kim YK, Lee NK. Factors related to relapse after mandibular setback surgery with minimal presurgical orthodontics. J Oral Maxillofac Surg. 2019 May;77(5):1072.e1-1072.e9. doi: 10.1016/j.joms.2018.12.030.
Tseng YC, Wu JH, Chen CM, Hsu KJ. Correlation between change of tongue area and skeletal stability after correction of mandibular prognathism. Kaohsiung J Med Sci. 2017 Jun;33(6):302-307. doi: 10.1016/j.kjms.2017.03.008.
Wolford LM, Karras SC, Mehra P. Considerations for orthognathic surgery during growth, Part 1: Mandibular deformities. Am J Orthod Dentofacial Orthop. 2001 Feb;119(2):95-101. doi: 10.1067/mod.2001.111401.
Chatkupt S SI, Patanaporn V, Bundech A, Apisariyakul S, Jotikasthira D. Cephalometric study in Northern Thai people. Research submitted to the Faculty of Dentistry, Chiang Mai: Chiang Mai University. 1987:1-84;
Kim JH, Gansukh O, Amarsaikhan B, Lee SJ, Kim TW. Comparison of cephalometric norms between Mongolian and Korean adults with normal occlusions and well-balanced profiles. Korean J Orthod. 2011 Feb;41(1):42-50. doi: 10.4041/kjod.2011.41.1.42.
Tweed CH. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am J Orthod Oral Surg. 1946 Apr;32(4):175-230. doi: 10.1016/0096-6347(46)90001-4.
Linjawi AI, Afify AR, Baeshen HA, Birkhed D, Zawawi KH. Mandibular symphysis dimensions in different sagittal and vertical skeletal relationships. Saudi J Biol Sci. 2021 Jan;28(1):280-285. doi: 10.1016/j.sjbs.2020.09.062
Burstone CJ, James RB, Legan H, Murphy G, Norton LA. Cephalometrics for orthognathic surgery. J Oral Surg. 1978 Apr;36(4):269-277.
Athanasiou AE. Orthodontic Cephalometry: Mosby-Wolfe; 1995.
Espeland L, Stenvik A. Long-term outcome of orthognathic surgery. Naretto DS, editor: In Tech; 2011. 584p. doi: 10.5772/22574.
Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007 Apr;3:21. doi: 10.1186/1746-160X-3-21.
Houston WJ. The analysis of errors in orthodontic measurements. Am J Orthod. 1983 May;83(5):382-390. doi: 10.1016/0002-9416(83)90322-6.
Kuo JJ, Lin CH, Ko EW. Relapse patterns of two-jaw surgical correction in patients with skeletal Class III malocclusion and different vertical facial types. Int J Oral Maxillofac Surg. 2022 Dec;51(12):1587-1595. doi: 10.1016/j.ijom.2022.05.016.
Joss CU, Thüer UW. Stability of the hard and soft tissue profile after mandibular advancement in sagittal split osteotomies: a longitudinal and long-term follow-up study. Eur J Orthod. 2008 Feb;30(1):16-23. doi: 10.1093/ejo/cjm080.
Phillips C, Zaytoun HS Jr, Thomas PM, Terry BC. Skeletal alterations following TOVRO or BSSO procedures. Int J Adult Orthodon Orthognath Surg.1986 Summer;1(3):203-213.
Franco JE, Van Sickels JE, Thrash WJ. Factors contributing to relapse in rigidly fixed mandibular setbacks. J Oral Maxillofac Surg. 1989 May;47(5):451-456. doi: 10.1016/0278-2391(89)90276-0.
Proffit WR, White RP. Surgical-orthodontic treatment: Mosby-Year Book; 1991.
Schatz JP, Tsimas P. Cephalometric evaluation of surgical-orthodontic treatment of skeletal Class III malocclusion. Int J Adult Orthodon Orthognath Surg. 1995;10(3):173-180.
de Villa GH, Huang CS, Chen PK, Chen YR. Bilateral sagittal split osteotomy for correction of mandibular prognathism: long-term results. J Oral Maxillofac Surg. 2005 Nov;63(11):1584-1592. doi: 10.1016/j.joms.2005.03.031.
Halvorsen ET, Beddari IY, Schilbred Eriksen E, Boe OE, Wisth PJ, Loes S, et al. Relapse and Stability After Mandibular Setback Surgery One Year Postoperatively: A Retrospective Study. J Oral Maxillofac Surg. 2014 Jun;72(6):1181.e1-1181e11. doi: 10.1016/j.joms.2014.02.033.
Moore KE, Gooris PJ, Stoelinga PJ. The contributing role of condylar resorption to skeletal relapse following mandibular advancement surgery: Report of five cases. J Oral Maxillofac Surg. 1991 May;49(5):448-460. doi: 10.1016/0278-2391(91)90166-J.
Jakobsone G, Stenvik A, Sandvik L, Espeland L. Three-year follow-up of bimaxillary surgery to correct skeletal Class III malocclusion: stability and risk factors for relapse. Am J Orthod Dentofacial Orthop. 2011 Jan;139(1):80-89. doi: 10.1016/j.ajodo.2009.03.050.
Morrill LR, Baumrind S, Miller D. Surgical correction of mandibular prognathism: I. A cephalometric report. Am J Orthod. 1974 May;65(5):503-518. doi: 10.1016/0002-9416(74)90032-3.
Kim MJ, Kim SG, Park YW. Positional stability following intentional posterior ostectomy of the distal segment in bilateral sagittal split ramus osteotomy for correction of mandibular prognathism. J Oral Maxillofac Surg. 2002 Feb;30(1):35-40. doi: 10.1054/jcms.2001.0272.
Kim CH, Lee JH, Cho JY, Lee JH, Kim KW. Skeletal stability after simultaneous mandibular angle resection and sagittal split ramus osteotomy for correction of mandible prognathism. J Oral Maxillofac Surg. 2007 Feb;65(2):192-197. doi: 10.1016/j.joms.2005.12.064.