Impaired oral function in older adults with type 2 diabetes
Main Article Content
Abstract
Objective: This cross-sectional study aimed to identify the occurrence of impaired oral functions (the number of teeth present, subjective difficulties in eating tough food and swallowing, oral moisture, chewing ability, and oral diadochokinesis (ODK)) in community-dwelling older adults with type 2 diabetes.
Materials and Methods: One hundred participants aged 60 and above in Lop Buri province, Thailand, were enrolled in this study. Demographic data, clinical data, and oral status were collected using questionnaires, medical records, and clinical examination. Oral moisture was measured using an oral moisture-checking device. Color-changeable chewing gum and a color scale were used to evaluate chewing ability. To evaluate ODK, the participants were asked to repeat each single syllable /pa/, /ta/, /ka/ for 5 seconds. The number of repetitions per second was recorded using the pen-dotting method. The data were analyzed using Pearson’s chi-squared test, Fisher’s exact test, correlation test, independent sample t-test, and the Mann-Whitney test.
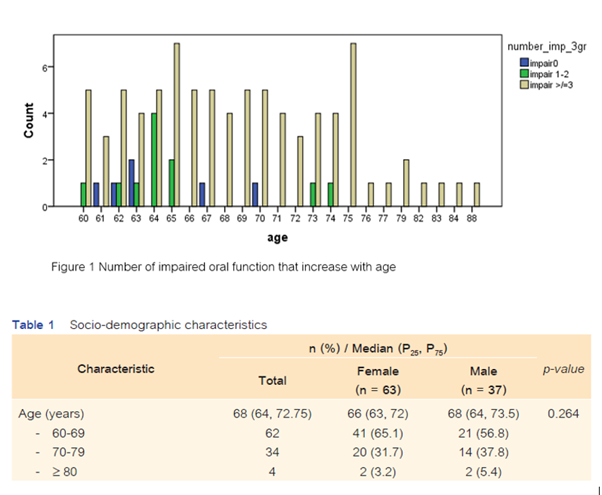
Results: The most common impaired oral function was decreased ODK (85%), followed closely by a decrease in the number of posterior occluding teeth (83%), subjective difficulties in eating tough food (72%), compromised chewing ability (35%), and impaired oral moisture (23%). Only 8% of the participants reported swallowing difficulties. Eighty-three participants (83%) experienced ≥3 impaired oral functions.
Conclusions: This study revealed the presence of impaired oral function in a group of diabetic older persons. The rapidity of lip and tongue movement, chewing ability, and oral moisture decreased in function. A decrease in oral function tended to correspond with increasing age and blood glucose level.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Ferrucci L, Cavazzini C, Corsi A, Bartali B, Russo C, Lauretani F, et al. Biomarkers of frailty in older persons. J Endocrinol Invest. 2002;25(10 Suppl):10-15.
Janto M, Iurcov R, Daina CM, Neculoiu DC, Venter AC, Badau D, et al. Oral health among elderly, impact on life quality, access of elderly patients to oral health services and methods to improve oral health: a narrative review. J Pers Med. 2022 Feb;12(3):372. doi: 10.3390/jpm12030372.
Iwasaki M, Yoshihara A, Sato M, Minagawa K, Shimada M, Nishimuta M, et al. Dentition status and frailty in community‐dwelling older adults: a 5‐year prospective cohort study. Geriatr Gerontol Int. 2018 Feb;18(2):256-262. doi: 10.1111/ggi.13170.
Iwasaki M, Yoshihara A, Sato N, Sato M, Minagawa K, Shimada M, et al. A 5‐year longitudinal study of association of maximum bite force with development of frailty in community‐dwelling older adults. J Oral Rehabil. 2018 Jan;45(1):17-24. doi: 10.1111/joor.12578.
Nishi T, Ohta M, Takano T, Ogami K, Ueda T, Sakurai K. Oral function is associated with the body and muscle mass indices of middle‐aged dental patients. Clin Exp Dent Res. 2022 Feb;8(1):217-224. doi: 10.1002/cre2.514.
Müller F, Shimazaki Y, Kahabuka F, Schimmel M. Oral health for an ageing population: the importance of a natural dentition in older adults. Int Dent J. 2017 Sep;67:7-13. doi: 10.1111/idj.12329.
Sheiham A, Steele JG, Marcenes W, Lowe C, Finch S, Bates CJ, et al. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res. 2001 Feb;80(2):408-413. doi: 10.1177/00220345010800020201.
Tanaka T, Takahashi K, Hirano H, Kikutani T, Watanabe Y, Ohara Y, et al. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci. 2018 Nov;73(12):1661-1667. doi: 10.1093/gerona/glx225.
Minakuchi S, Tsuga K, Ikebe K, Ueda T, Tamura F, Nagao K, et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology. 2018 Dec;35(4):317-324. doi: 10.1111/ger.12347.
Kugimiya Y, Watanabe Y, Ueda T, Motokawa K, Shirobe M, Igarashi K, et al. Rate of oral frailty and oral hypofunction in rural community‐dwelling older Japanese individuals. Gerodontology. 2020 Dec;37(4):342-352. doi: 10.1111/ger.12468.
Kamdem B, Seematter-Bagnoud L, Botrugno F, Santos-Eggimann B. Relationship between oral health and Fried’s frailty criteria in community-dwelling older persons. BMC Geriatr. 2017 Aug;17(1):174. doi: 10.1186/s12877-017-0568-3.
Tanaka T, Takahashi K, Hirano H, Kikutani T, Watanabe Y, Ohara Y, et al. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci. 2018 Nov;73(12):1661-1667. doi: 10.1093/gerona/glx225.
Shimazaki Y, Nonoyama T, Tsushita K, Arai H, Matsushita K, Uchibori N. Oral hypofunction and its association with frailty in community‐dwelling older people. Geriatr Gerontol Int. 2020 Oct;20(10):917-926. doi: 10.1111/ggi.14015.
Iwasaki M, Motokawa K, Watanabe Y, Shirobe M, Inagaki H, Edahiro A, et al. A two-year longitudinal study of the association between oral frailty and deteriorating nutritional status among community-dwelling older adults. Int J Environ Res Public Health. 2020 Dec;18(1):213. doi: 10.3390/ijerph18010213.
Okada K, Enoki H, Izawa S, Iguchi A, Kuzuya M. Association between masticatory performance and anthropometric measurements and nutritional status in the elderly. Geriatr Gerontol Int. 2010 Jan;10(1):56-63. doi: 10.1111/j.1447-0594.2009.00560.x.
Watanabe Y, Hirano H, Arai H, Morishita S, Ohara Y, Edahiro A, et al. Relationship between frailty and oral function in community‐dwelling elderly adults. J Am Geriatr Soc. 2017 Jan;65(1):66-76. doi: 10.1111/jgs.14355.
Musacchio E, Perissinotto E, Binotto P, Sartori L, Silva-Netto F, Zambon S, et al. Tooth loss in the elderly and its association with nutritional status, socio-economic and lifestyle factors. Acta Odontol Scand. 2007 Apr;65(2):78-86. doi: 10.1080/00016350601058069.
Yamazaki T, Yamori M, Asai K, Nakano-Araki I, Yamaguchi A, Takahashi K, et al. Mastication and risk for diabetes in a Japanese population: a cross-sectional study. PLoS One. 2013 Jun;8(6):e64113. doi: 10.1371/journal.pone.0064113.
Morley JE. Oral Frailty. J Nutr Health Aging. 2020;24(7):683-684. doi: 10.1007/s12603-020-1438-9.
Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, et al. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013 Oct;1(2):106-114. doi: 10.1016/S2213-8587(13)70046-9.
IDF Diabetes Atlas, 10th edn. Brussels, Belgium: International Diabetes Federation; 2021.
Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2007 Sep;138 Suppl:S15-S20. doi: 10.14219/jada.archive.2007.0358.
Chomkhakhai U, Thanakun S, Khovidhunkit S-oP, Khovidhunkit W, Thaweboon S. Oral health in Thai patients with metabolic syndrome. Diabetes Metab Syndr. 2009;3(4):192-197. doi:10.1016/j.dsx.2009.08.004.
Iwasaki M, Kimura Y, Sasiwongsaroj K, Kettratad‐Pruksapong M, Suksudaj S, Ishimoto Y, et al. Association between objectively measured chewing ability and frailty: A cross‐sectional study in central Thailand. Geriatr Gerontol Int. 2018 Jun;18(6):860-866. doi: 10.1111/ggi.13264.
Aekplakorn W. Thailand National Health Examination Surveys 6th. 2019-2020.
Daniel WW, Cross CL. Biostatistics: a foundation for analysis in the health sciences: Wiley; 2018.
Trongsakul S, Lambert R, Clark A, Wongpakaran N, Cross J. Development of the Thai version of Mini‐C og, a brief cognitive screening test. Geriatr Gerontol Int. 2015 May;15(5):594-600. doi: 10.1111/ggi.12318.
Dhatariya KK, Glaser NS, Codner E, Umpierrez GE. Diabetic ketoacidosis. Nat Rev Dis Primers. 2020 May;6(1):40. doi: 10.1038/s41572-020-0165-1.
Organization WH. Oral health surveys: basic methods: World Health Organization; 2013.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008 Dec;117(12):919-924. doi: 10.1177/000348940811701210.
Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10(2):61-63. doi: 10.3109/09638288809164103.
Wongpakaran N, Wongpakaran T, Kuntawong P. Evaluating hierarchical items of the geriatric depression scale through factor analysis and item response theory. Heliyon. 2019 Aug;5(8):e02300. doi: 10.1016/j.heliyon.2019.e02300.
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001 Jun;56(6):M366-M372. doi: 10.1093/gerona/56.6.m366.
Jitnarin N, Kosulwat V, Rojroongwasinkul N, Boonpraderm A, Haddock C, Poston W. Prevalence of overweight and obesity in Thai population: results of the National Thai Food Consumption Survey. Eat Weight Disord. 2011 Dec;16(4):e242-e249. doi: 10.1007/BF03327467.
Hildebrandt GH, Dominguez BL, Schork MA, Loesche WJ. Functional units, chewing, swallowing, and food avoidance among the elderly. J Prosthet Dent. 1997 Jun;77(6):588-595. doi: 10.1016/s0022-3913(97)70100-8.
Quandt SA, Chen H, Bell RA, Savoca MR, Anderson AM, Leng X, et al. Food avoidance and food modification practices of older rural adults: association with oral health status and implications for service provision. Gerontologist. 2010 Feb;50(1):100-111. doi: 10.1093/geront/gnp096.
Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967 Nov-Dec;38(6):610-616. doi: 10.1902/jop.1967.38.6.610.
Takahashi F, Koji T, Morita O. Oral dryness examinations: use of an oral moisture checking device and a modified cotton method. Prosthodont Res Prac. 2006;5(1):26-30.
Fukushima Y, Kokabu S, Kanaya A, Hori N, Takeyama T, Sato T, et al. Experimental examination of appropriate measurement method of oral moisture checking device. J Japanese Society for Oral Mucous Membrane. 2007;13(1):16-25.
Tarkowska A, Katzer L, Ahlers MO. Assessment of masticatory performance by means of a color-changeable chewing gum. J Prosthodont Res. 2017 Jan;61(1):9-19. doi: 10.1016/j.jpor.2016.04.004.
Ben-David BM, Icht M. The effect of practice and visual feedback on oral-diadochokinetic rates for younger and older adults. Lang Speech. 2018 Mar;61(1):113-134. doi: 10.1177/0023830917708808.
Clinical Practice Guideline for Diabetes 2023. Bangkok: Srimuang Printing; 2023. 263 p.
Cifu DX, Lew HL, Oh-Park M. Geriatric rehabilitation: Elsevier Health Sciences; 2018.
Hirano H, Ishiyama N, Watanabe I, Nasu I. Masticatory ability in relation to oral status and general health on aging. J Nutr Health Aging. 1999;3(1):48-52.
Özsürekci C, Kara M, Güngör AE, Ayçiçek GŞ, Çalışkan H, Doğu BB, et al. Relationship between chewing ability and malnutrition, sarcopenia, and frailty in older adults. Nutr Clin Pract. 2022 Dec;37(6):1409-1417. doi: 10.1002/ncp.10877.
Watanabe Y, Hirano H, Arai H, Morishita S, Ohara Y, Edahiro A, et al. Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc. 2017 Jan;65(1):66-76. doi: 10.1111/jgs.14355.
Dental Health Bureau. The 8th National oral health survey report, 2017. Bangkok: Samcharoen-panit Co.; 2018.
Speksnijder C, Abbink J, Van Der Glas H, Janssen N, Van Der Bilt A. Mixing ability test compared with a comminution test in persons with normal and compromised masticatory performance. Eur J Oral Sci. 2009 Oct;117(5):580-586. doi: 10.1111/j.1600-0722.2009.00675.x.
Komagamine Y, Kanazawa M, Minakuchi S, Uchida T, Sasaki Y. Association between masticatory performance using a colour‐changeable chewing gum and jaw movement. J Oral Rehabil. 2011 Aug;38(8):555-563. doi: 10.1111/j.1365-2842.2011.02204.x.
Hama Y, Hosoda A, Komagamine Y, Gotoh S, Kubota C, Kanazawa M, et al. Masticatory performance‐related factors in preschool children: establishing a method to assess masticatory performance in preschool children using colour‐changeable chewing gum. J Oral Rehabil. 2017 Dec;44(12):948-956. doi: 10.1111/joor.12553.
Matsui Y, Ohno K, Michi K, Hata H, Yamagata K, Ohtsuka S. The evaluation of masticatory function with low adhesive colour‐developing chewing gum. J Oral Rehabil. 1996 Apr;23(4):251-256. doi: 10.1111/j.1365-2842.1996.tb00849.x.
Moriya S, Notani K, Miura H, Inoue N. Relationship between masticatory ability and physical performance in community‐dwelling edentulous older adults wearing complete dentures. Gerodontology. 2014 Dec;31(4):251-259. doi: 10.1111/ger.12029.
Kamiyama M, Kanazawa M, Fujinami Y, Minakuchi S. Validity and reliability of a Self-Implementable method to evaluate masticatory performance: use of color-changeable chewing gum and a color scale. J Prosthodont Res. 2010 Jan;54(1):24-28. doi: 10.1016/j.jpor.2009.08.001.
Wang YY, Gao K, Zhao Y, Kuruvilla-Dugdale M, Lever TE, Bunyak F. DeepDDK: A Deep Learning based oral-diadochokinesis analysis software. IEEE EMBS Int Conf Biomed Health Inform. 2019;2019:1-4. doi: 10.1109/bhi.2019.8834506.
Morisaki N. Effects of oral exercise on oral function among Japanese dependent elderly individuals living in nursing facilities. Int J Nurs Clin Pract. 2018;5:301. doi: 10.15344/2394-4978/2018/301.
Konishi M. Can oral diadochokinesis be used as an assessment tool of oral function in older adults requiring care in nursing home? J Oral Rehabil. 2024 Feb;51(2):328-333. doi: 10.1111/joor.13594.
Hatanaka Y, Furuya J, Sato Y, Taue R, Uchida Y, Shichita T, et al. Regular oral health management improved oral function of outpatients with oral hypofunction in dental hospital: a longitudinal study. Int J Environ Res Public Health. 2022 Feb;19(4):2154. doi: 10.3390/ijerph19042154.