Effect of classical music and delta-wave music on sleep bruxism: a pilot study
Main Article Content
Abstract
Objectives: To determine the effects of classical music and delta-wave music on sleep bruxism, stress, and sleep quality.
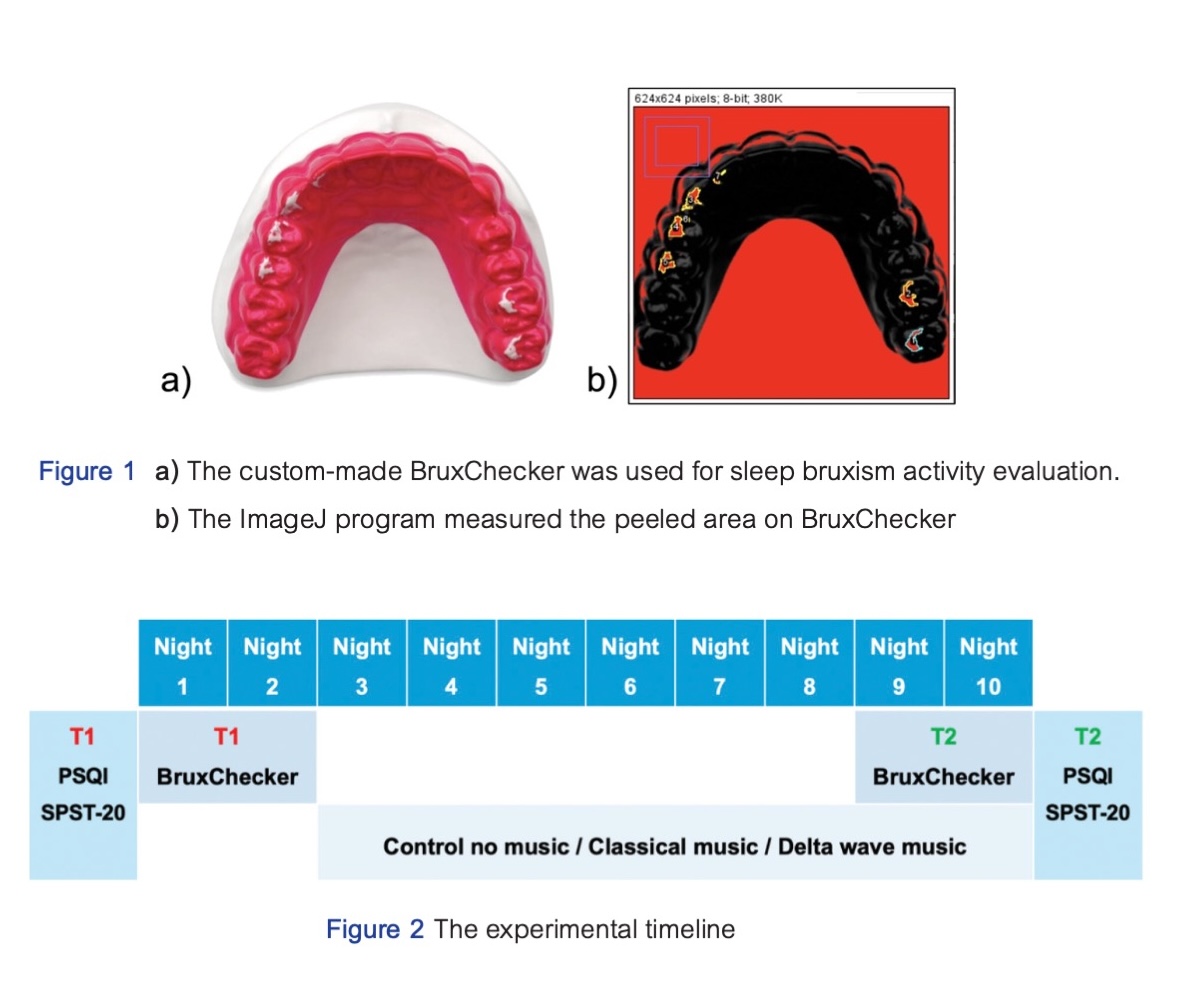
Materials and Methods: Eighteen pre-clinical dental student volunteers with self-reported sleep bruxism were recruited from the Faculty of Dentistry Mahidol University. Subjects were randomly and equally divided into 3 groups: control, classical music, and delta-wave music. All participants wore T1 BruxChecker during sleep on the 1st and 2nd night and T2 BruxChecker on the 9th and 10th night. During the 3rd to 10th experimental night, subjects in both music groups listened to the assigned music track for 1 hour before bedtime using headphones, while the control group did not listen to any music. All subjects took the Suanprung stress test (SPST-20) and Pittsburgh sleep quality (PSQI) questionnaires before and after the trial period. The peeled area on BruxChecker and scores from both questionnaires were analyzed using the Wilcoxon and Kruskal-Wallis tests.
Results: All experimental groups showed no statistically significant changes in the peeled area on BruxChecker during the trial. There was no statistically significant difference in the peeled area on BruxChecker among all groups. Only the classical music group showed decreasing stress levels after the trial, although not statistically significant. The delta-wave music group revealed almost statistically significant improved sleep quality (p=0.058).
Conclusion: Our pilot study is the first experiment to investigate the effect of classical and delta-wave music on sleep bruxism. Although the results are still inconclusive and neither type of music significantly reduced sleep bruxism activity, listening to classical music revealed a tendency toward relieving stress and reducing sleep bruxism, whereas delta-wave music showed a tendency toward sleep quality improvement.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Yap AU, Chua AP. Sleep bruxism: Current knowledge and contemporary management. J Conserv Dent. 2016 Sep-Oct;19(5):383-389. doi: 10.4103/0972-0707.190007.
Lobbezoo F, Rompre PH, Soucy JP, Iafrancesco C, Turkewicz J, Montplaisir JY, et al. Lack of associations between occlusal and cephalometric measures, side imbalance in striatal D2 receptor binding, and sleep-related oromotor activities. J Orofac Pain. 2001;15(1):64-71.
Fluerasu MI, Bocsan IC, Tig IA, Iacob SM, Popa D, Buduru S. The epidemiology of bruxism in relation to psychological factors. Int J Environ Res Public Health. 2022 Jan;19(2):691. doi: 10.3390/ijerph19020691.
Minakuchi H, Fujisawa M, Abe Y, Iida T, Oki K, Okura K, et al. Managements of sleep bruxism in adult: A systematic review. Jpn Dent Sci Rev. 2022 Nov;58:124-36. doi: 10.1016/j.jdsr.2022.02.004.
Guaita M, Hogl B. Current treatments of bruxism. Curr Treat Options Neurol. 2016 Feb;18(2):10. doi: 10.1007/s11940-016-0396-3.
Lal S.J., Sankari A., Weber DK. (2024) Bruxism Management. In: StatPearls. Treasure Island, FL: StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/pubmed/29494073 [Accessed 1 May 2024]
Chemelo VDS, Ne YGS, Frazao DR, de Souza-Rodrigues RD, Fagundes NCF, Magno MB, et al. Is there association between stress and bruxism? A systematic review and meta-analysis. Front Neurol. 2020 Dec;11:590779. doi: 10.3389/fneur.2020.590779.
Monti F, Tonetti L, Bitti PE. Effectiveness of psychological treatments delivered at a counseling service for students. Psychol Rep. 2013 Dec;113(3):955-968. doi: 10.2466/21.02.PR0.113x28z4.
Carlson LE, Toivonen K, Subnis U. Integrative approaches to stress management. Cancer J. 2019 Se-Oct;25(5):329-336. doi: 10.1097/PPO.0000000000000395.
de Witte M, Spruit A, van Hooren S, Moonen X, Stams GJ. Effects of music interventions on stress-related outcomes: a systematic review and two meta-analyses. Health Psychol Rev. 2020 Jun;14(2):294-324. doi 10.1080/17437199.2019.1627897.
Lavigne GJ, Kato T, Kolta A, Sessle BJ. Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med. 2003;14(1):30-46. doi: 10.1177/154411130301400104.
Gao D, Long S, Yang H, Cheng Y, Guo S, Yu Y, et al. SWS brain-wave music may improve the quality of sleep: An EEG study. Front Neurosci. 2020 Feb;14:67. doi: 10.3389/fnins.2020.00067.
Chen CK, Pei YC, Chen NH, Huang LT, Chou SW, Wu KP, et al. Sedative music facilitates deep sleep in young adults. J Altern Complement Med. 2014 Apr;20(4):312-317. doi: 10.1089/acm.2012.0050.
Darki C, Riley J, Dadabhoy DP, Darki A, Garetto J. The effect of classical music on heart rate, blood pressure, and mood. Cureus. 2022 Jul;14(7):e27348. doi: 10.7759/cureus.27348.
Dabiri R, Monazzam Esmaielpour MR, Salmani Nodoushan M, Khaneshenas F, Zakerian SA. The effect of auditory stimulation using delta binaural beat for a better sleep and post-sleep mood: A pilot study. Digit Health. 2022 May;8:20552076221102243. doi: 10.1177/20552076221102243.
Drake C, Roehrs T, Shambroom J, Roth T. Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. J Clin Sleep Med. 2013 Nov;9(11):1195-1200. doi: 10.5664/jcsm.3170.
Morssinkhof MWL, van Wylick DW, Priester-Vink S, van der Werf YD, den Heijer M, van den Heuvel OA, et al. Associations between sex hormones, sleep problems and depression: A systematic review. Neurosci Biobehav Rev. 2020 Nov;118:669-680. doi: 10.1016/j.neubiorev.2020.08.006.
Baker FC, Driver HS. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. 2007 Sep;8(6):613-622. doi: 10.1016/j.sleep.2006.09.011.
Onodera K, Kawagoe T, Sasaguri K, Protacio-Quismundo C, Sato S. The use of a bruxchecker in the evaluation of different grinding patterns during sleep bruxism. Cranio. 2006 Oct;24(4):292-299. doi: 10.1179/crn.2006.045.
Greven M, Onodera K, Sato S. The use of the BruxChecker in the evaluation and treatment of bruxism Beurteilung und Therapie des Bruxismus mit dem BruxChecker. Zeitschrift für Kraniomandibuläre Funktion. 2015;7(3):249-259.
Prommasen D, Chatchaiyan N, Mitrirattanakul S. Sensitivity of Brux checker® in grinding bruxer. J Dent Assoc Thai. 2023;73(1):37-44. doi: 10.14456/jdat.2023.5.
Mahatnirunkul S. Pumpisalchai W, Thapanya P. The construction of Suan Prung stress test for Thai population. Bulletin of Suan Prung. 1997;13(3):1-20.
Sitasuwan T, Bussaratid S, Ruttanaumpawan P, Chotinaiwattarakul W. Reliability and validity of the Thai version of the Pittsburgh Sleep Quality Index. J Med Assoc Thai. 2014 Mar;97 Suppl 3:S57-S67.
Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989 May;28(2):193-213. doi: 10.1016/0165-1781(89)90047-4.
Nilsson U. The anxiety- and pain-reducing effects of music interventions: a systematic review. AORN J. 2008 Apr;87(4):780-807. doi: 10.1016/j.aorn.2007.09.013.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339.
Zhao F, Sun Z, Niu W. Effect of ward noise reduction technology combined with music therapy on negative emotions in inpatients undergoing gastric cancer radiotherapy: A retrospective study. Noise Health. 2023 Oct-Dec;25(119):257-263. doi: 10.4103/nah.nah_72_23.
Carter C. Healthcare performance and the effects of the binaural beats on human blood pressure and heart rate. J Hosp Mark Public Relations. 2008;18(2):213-219. doi: 10.1080/15390940802234263.
Sundar S, Ramesh B, Anandraj R. Effect of relaxing music on blood pressure and heart rate in hospitalized pre-hypertensive women in 3rd trimester of pregnancy: a randomized control study. Asian J Pharm Clin Res. 2015;8(5):179-181.
Umbrello M, Sorrenti T, Mistraletti G, Formenti P, Chiumello D, Terzoni S. Music therapy reduces stress and anxiety in critically ill patients: a systematic review of randomized clinical trials. Minerva Anestesiol. 2019 Aug;85(8):886-898. doi: 10.23736/S0375-9393.19.13526-2.
Harmat L, Takacs J, Bodizs R. Music improves sleep quality in students. J Adv Nurs. 2008 May;62(3):327-335. doi: 10.1111/j.1365-2648.2008.04602.x
Pierce CJ, Gale EN. Methodological considerations concerning the use of Bruxcore Plates to evaluate nocturnal bruxism. J Dent Res. 1989 Jun;68(6):1110-1114. doi: 10.1177/00220345890680061101.
Piyawattanataworn W. Siritapetawee M, Chatrchaiwiwatana S, Paphangkorakit J. Validity of wear at the upper canine’s cusp tip in predicting sleep bruxism. J Med Assoc Thai. 2020;103(Suppl.1):7-12.
Levin YaI. "Brain music" in the treatment of patients with insomnia. Neurosci Behav Physiol. 1998 May-Jun;28(3):330-335. doi: 0.1007/BF02462965.
Ngo HV, Claussen JC, Born J, Molle M. Induction of slow oscillations by rhythmic acoustic stimulation. J Sleep Res. 2013 Feb;22(1):22-31. doi: 10.1111/j.1365-2869.2012.01039.x.
Basudan S, Binanzan N, Alhassan A. Depression, anxiety and stress in dental students. Int J Med Educ. 2017 May;8:179-186. doi: 10.5116/ijme.5910.b961.
Cavallo P, Carpinelli L, Savarese G. Perceived stress and bruxism in university students. BMC Res Notes. 2016 Dec;9(1):514. doi: 10.1186/s13104-016-2311-0.
Thoma MV, La Marca R, Bronnimann R, Finkel L, Ehlert U, Nater UM. The effect of music on the human stress response. PLoS One. 2013 Aug;8(8):e70156. doi: 10.1371/journal.pone.0070156.
Cordi MJ, Ackermann S, Rasch B. Effects of Relaxing Music on Healthy Sleep. Sci Rep. 2019 Jun;9(1):9079. doi: 10.1038/s41598-019-45608-y.
Saczuk K, Lapinska B, Wilmont P, Pawlak L, Lukomska-Szymanska M. Relationship between sleep bruxism, perceived stress, and coping strategies. Int J Environ Res Public Health. 2019 Sep;16(17):3193. doi: 10.3390/ijerph16173193.
Lastinger DL. The effect of background music on the perception of personality and demographics. J Music Ther. 2011;48(2):208-225. doi: 10.1093/jmt/48.2.208.