Comparison of bond strength between two resin cement systems used in modified tube technique for separated endodontic instruments removal
Main Article Content
Abstract
Objective: The aim of this study was to compare bond strength between two resin cements including Super Bond Universal and RelyX U200 used for separated instrument removal with modified tube technique
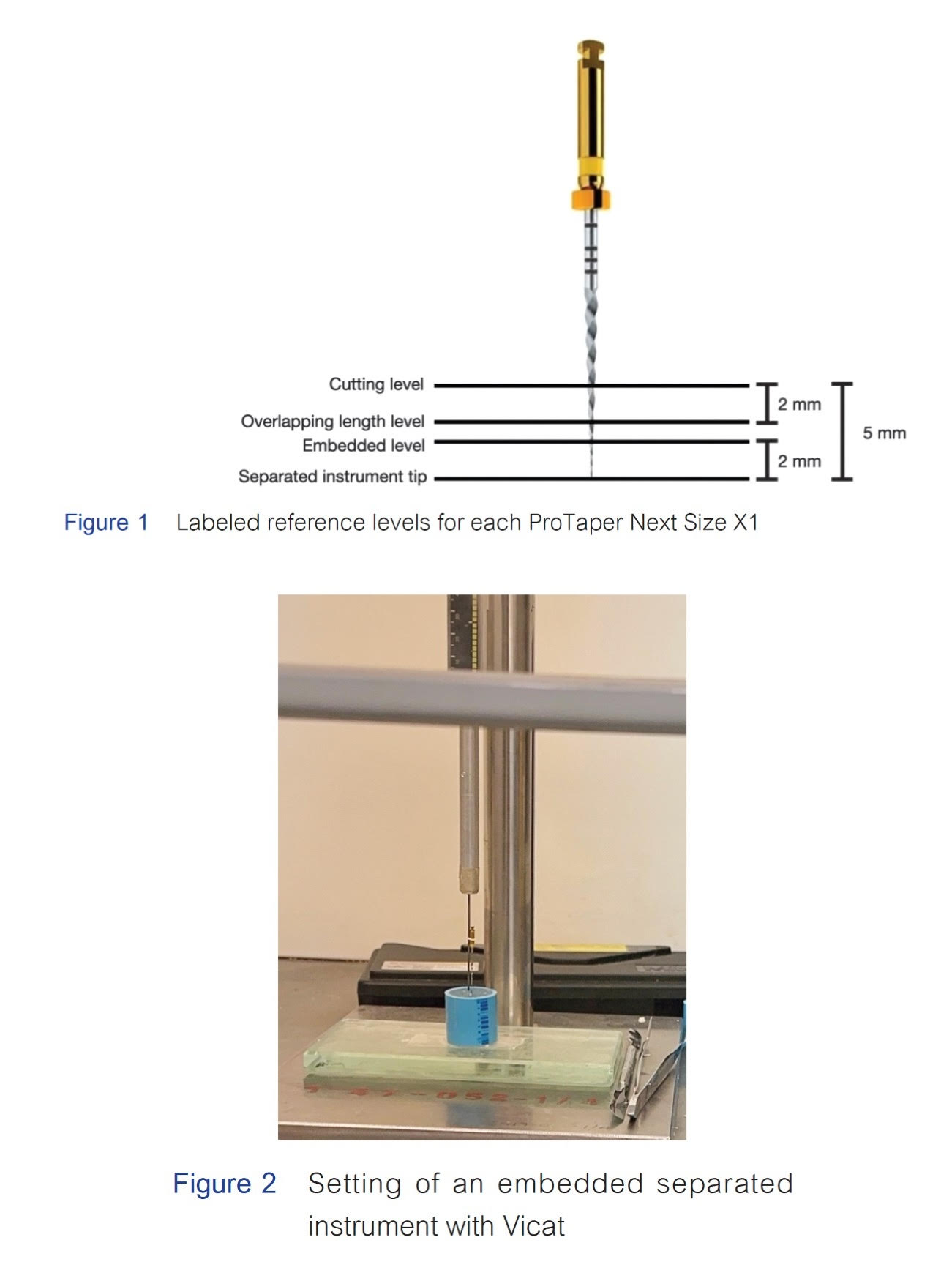
Materials and Methods: Thirty ProTaper Next X1 NiTi rotary files were embedded into the fixing mold then cut at 5 mm from the instrument tip in order to simulate the separated instrument engaged in the root canal. The samples were divided into 2 experimental groups according to chemical agents for adhesion in tube and glue technique, Group 1: Super Bond Universal, and Group 2: RelyX U200 (n = 15/group). Resin cements were prepared and loaded into the hypodermic tube before insertion onto each separated instrument at 2 mm overlapping length. After the complete setting of the material, all samples were subjected to pull-out test at a constant speed of 2 mm/min. using the Universal Testing Machine. The failure load of each sample was recorded and the data was analyzed using Shapiro-Wilk Test and Levene’s Test to confirm the normality and homogeneity of variance following by an independent samples t-test for group comparison.
Results: Mean failure loads of group 1 and group 2 were 1.62 N and 15.50 N. The bond strength of RelyX U200 was significantly higher than Super Bond Universal (p<0.001).
Conclusion: Due to the compositions affected the molecular structure of this resin cement together with convenient application, the bond strength of RelyX U200 is significantly superior over that of Super Bond Universal.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Byström A, Byström A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Eur J Oral Sci. 1981 Aug 1;89(4):321–328. doi: 10.1111/j.1600-0722.1981.tb01689.x.
Ruddle, CJ. Micro-endodontic non-surgical retreatment. Dent Clin North Am. 1997 Jul;41(3):429-454. doi: 9248684
Crump MC, Natkin E. Relationship of broken root canal instruments to endodontic case prognosis: a clinical investigation. J Am Dent Assoc. 1970 Jun;80(6):1341–1347. doi: 10.14219/jada.archive.
0259.
Strindberg L. The dependence of the results of pulp therapy on certain factors. An analytic study based on radiographic and clinical follow up examination. Acta Odontol Scand Suppl. 1956;14 Suppl21:S.176-S177.
Madarati AA, Hunter MJ, Dummer PM. Management of intracanal separated instruments. J Endod. 2013 May 1;39(5):569–581. doi: 10.1016/j.joen.2012.12.033.
Spili P, Parashos P, Messer HH. The impact of instrument fracture on outcome of endodontic treatment. J Endod. 2005 Dec;31(12):845–850. doi: 10.1097/01.don.0000164127.62864.7c.
Panitvisai P, Parunnit P, Sathorn C, Messer HH. Impact of a retained instrument on treatment Outcome: A Systematic review and Meta-analysis. J Endod. 2010 May;36(5):775–780. doi: 10.1016/j.joen.2009.12.029.
Suter B, Lussi A, Sequeira P. Probability of removing fractured instruments from root canals. Int Endod J. 2005 Feb;38(2):112–123. doi: 10.1111/j.1365-2591.2004.00916.x.
Ruddle CJ. Nonsurgical retreatment. J Endod. 2004 Dec;30(12):827–845. doi: 10.1097/01.don.0000145033.15701.2d.
Ruddle CJ. Broken instrument removal. The endodontic challenge. Dent Today. 2002 Jul;21(7):70-72, 74, 76 passim.
Eleazer PD, O’Connor RP. Innovative uses for hypodermic needles in endodontics. J Endod. 1999 Mar;25(3):190–191. doi: 10.1016/S0099-2399(99)80140-X.
Wefelmeier M, Eveslage M, Bürklein S, Ott K, Kaup M. Removing Fractured Endodontic Instruments with a Modified Tube Technique Using a Light-curing Composite. J Endod. 2015 May;41(5):733–736 doi: 10.1016/j.joen.2015.01.018.
Le PT, Weinstein M, Borislow AJ, Braitman LE. Bond failure and decalcification: a comparison of a cyanoacrylate and a composite resin bonding system in vivo. Am J Orthod Dentofacial Orthop. 2003 Jun;123(6):624–627. doi: 10.1016/s0889-5406(03)00196-3.
Bishara SE, VonWald L, Olsen ME, Laffoon JF. Effect of time on the shear bond strength of glass ionomer and composite orthodontic adhesives. Am J Orthod Dentofacial Orthop. 1999 Dec;116(6):616–620. doi: 10.1016/s0889-5406(99)70195-2.
Olczak K, Grabarczyk J, Szymański W. Removing Fractured Endodontic Files with a Tube Technique—The Strength of the Glued Joint: Tube-Endodontic File Setup. Materials (Basel). 2023 May;16(11):4100. doi: 10.3390/ma16114100.
Stamatacos C, Simon JF. Cementation of indirect restorations: an overview of resin cements. Compend Contin Educ Dent. 2013 Jan;34(1):42-44, 46.
Bürklein S, Donnermeyer D, Wefelmeier M, Schäfer E, Urban K. Removing fractured endodontic NiTi instruments with a tube technique: influence of pre-treatment with various agents on adhesive forces In vitro. Materials (Basel). 2019 Dec;13(1):144. doi: 10.3390/ma13010144.
Chang JC, Hurst TL, Hart DA, Estey AW. 4-META use in dentistry: A literature review. J Prosthet Dent. 2002 Feb;87(2):216–224. doi: 10.1067/mpr.2002.121584.
Camargo FSAS, González AHM, Alonso RCB, Di Hipólito V, D’Alpino PHP. Effects of polymerization mode and interaction with hydroxyapatite on the rate of pH neutralization, mechanical properties, and depth of cure in self-adhesive cements. Eur J Dent. 2019 May;13(02):178–186. doi: 10.1055/s-0039-1696057.
Baroudi K, Rodrigues JC. Flowable resin composites: A systematic review and clinical considerations. J Clin Diagn Res. 2015 Jun;9(6):ZE18-24. doi: 10.7860/JCDR/2015/12294.6129.
Kim HC, Kwak SW, Cheung GS, Ko DH, Chung SM, Lee W. Cyclic fatigue and torsional resistance of two new nickel-titanium instruments used in reciprocation motion: Reciproc versus WaveOne. J Endod. 2012 Apr;38(4):541–544. doi: 10.1016/j.joen.2011.11.014.
Castelló-Escrivá R, Alegre-Domingo T, Faus-Matoses V, Román-Richon S, Faus-Llácer VJ. In vitro comparison of cyclic fatigue resistance of ProTaper, WaveOne, and Twisted Files. J Endod. 2012 Nov;38(11):1521–1524. doi: 10.1016/j.joen.2012.07.010.
Dagna A, Poggio C, Beltrami R, Colombo M, Chiesa M, Bianchi S. Cyclic fatigue resistance of OneShape, Reciproc, and WaveOne: An in vitro comparative study. J Conserv Dent. 2014 Jan;17(3):250–254. doi: 10.4103/0972-0707.131788.
Gomes MS, Vieira RM, Böttcher DE, Plotino G, Celeste RK, Rossi‐Fedele G. Clinical fracture incidence of rotary and reciprocating NiTi files: A systematic review and meta‐regression. Aust Endod J. 2021 Aug;47(2):372–385. doi: 10.1111/aej.12484.
Ertas H, Capar ID. An in vitro analysis of separation of multi‐use ProTaper Universal and ProTaper Next instruments in extracted mandibular molar teeth. Scanning. 2015 Jul-Aug;37(4):270–276. doi: 10.1002/sca.21209.
Racovita AD. Titanium dioxide: structure, impact, and toxicity. Int J Environ Res Public Health. 2022 May;19(9):5681. doi: 10.3390/ijerph19095681.
Tomov T, Tsoneva I. Are the stainless steel electrodes inert? Bioelectrochemistry. 2000 Jun;51(2):207–209. doi: 10.1016/s0302-4598(00)00069-6.
Gao Y, Zhang J, Liang J, Yuan D, Zhao W. Research progress of poly (methyl methacrylate) microspheres: Preparation, functionalization and application. Eur Polym J. 2022 Jul;175:111379. doi: 10.1016/j.eurpolymj.2022.111379.
Kaur H, Thakur A. Applications of poly(methyl methacrylate) polymer in dentistry: A review. Mater Today Proc. 2022 Jan;50:1619–1625. doi: 10.1016/j.matpr.2021.09.125.
Awaja F, Zhang S, Tripathi M, Nikiforov A, Pugno N. Cracks, microcracks and fracture in polymer structures: Formation, detection, autonomic repair. Prog Mater Sci. 2016 Oct;83:536–573. doi:10.1016/J.PMATSCI.
07.007.
Liu W, Meng H, Sun Z, Jiang R, Dong C, Zhang C. Phosphoric and carboxylic methacrylate esters as bonding agents in self-adhesive resin cements. Exp Ther Med. 2018 May;15(5):4531–4537. doi: 10.3892/etm.2018.5937.
Tsuchimoto Y, Yoshida Y, Mine A, Nakamura M, Nishiyama N, Van Meerbeek B, et al. Effect of 4-MET- and 10-MDP-based primers on resin bonding to titanium. Dent Mater J. 2006 Mar;25(1):120–124. doi: 10.4012/dmj.25.120.
Delgado AHS, Owji N, Ashley P, Young AM. Varying 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) level improves polymerisation kinetics and flexural strength in self-adhesive, remineralising composites. Dent Mater. 2021 Sep;37(9):1366–1376. doi: 10.1016/j.dental.2021.06.006.
Ceylan G, Emik S, Yalcinyuva T, Sunbuloğlu E, Bozdag E, Unalan F. The effects of Cross-Linking agents on the mechanical properties of poly (Methyl methacrylate) resin. Polymers (Basel). 2023 May;15(10):2387. doi: 10.3390/polym15102387.
Maletin A, Knežević MJ, Koprivica DĐ, Veljović T, Puškar T, Milekić B, et al. Dental resin-based luting materials—review. Polymers (Basel). 2023 Oct;15(20):4156. doi: 10.3390/polym15204156.
Gheller R, Burey A, Vicentin BLS, Reis PJ, Appoloni CR, Garbelini CCD, et al. Microporosity and polymerization contraction as function of depth in dental resin cements by X‐ray computed microtomography. Microsc Res Tech. 2020 Jun;83(6):658–666. doi: 10.1002/jemt.23456.
Lopes Cde C, Rodrigues RB, Silva AL, Simamoto Júnior PC, Soares CJ, Novais VR. Degree of conversion and mechanical properties of resin cements cured through different All-Ceramic systems. Braz Dent J. 2015 Oct;26(5):484–489. doi: 10.1590/0103-6440201300180.
Jang Y, Ferracane JL, Pfeifer CS, Park JW, Shin Y, Roh BD. Effect of insufficient light exposure on polymerization kinetics of conventional and self-adhesive dual-cure resin cements. Oper Dent. 2017 Jan/Feb;42(1):E1–E9. doi: 10.2341/15-278-L