Comparing maxillary surgical accuracy in mandible-first and maxilla-first sequencing for bimaxillary orthognathic surgery: a retrospective study in facial asymmetry patients
Main Article Content
Abstract
Objective: This study aimed to compare the surgical accuracy of the maxilla between the maxilla- and mandible-first sequence bimaxillary orthognathic surgery for facial asymmetry patients
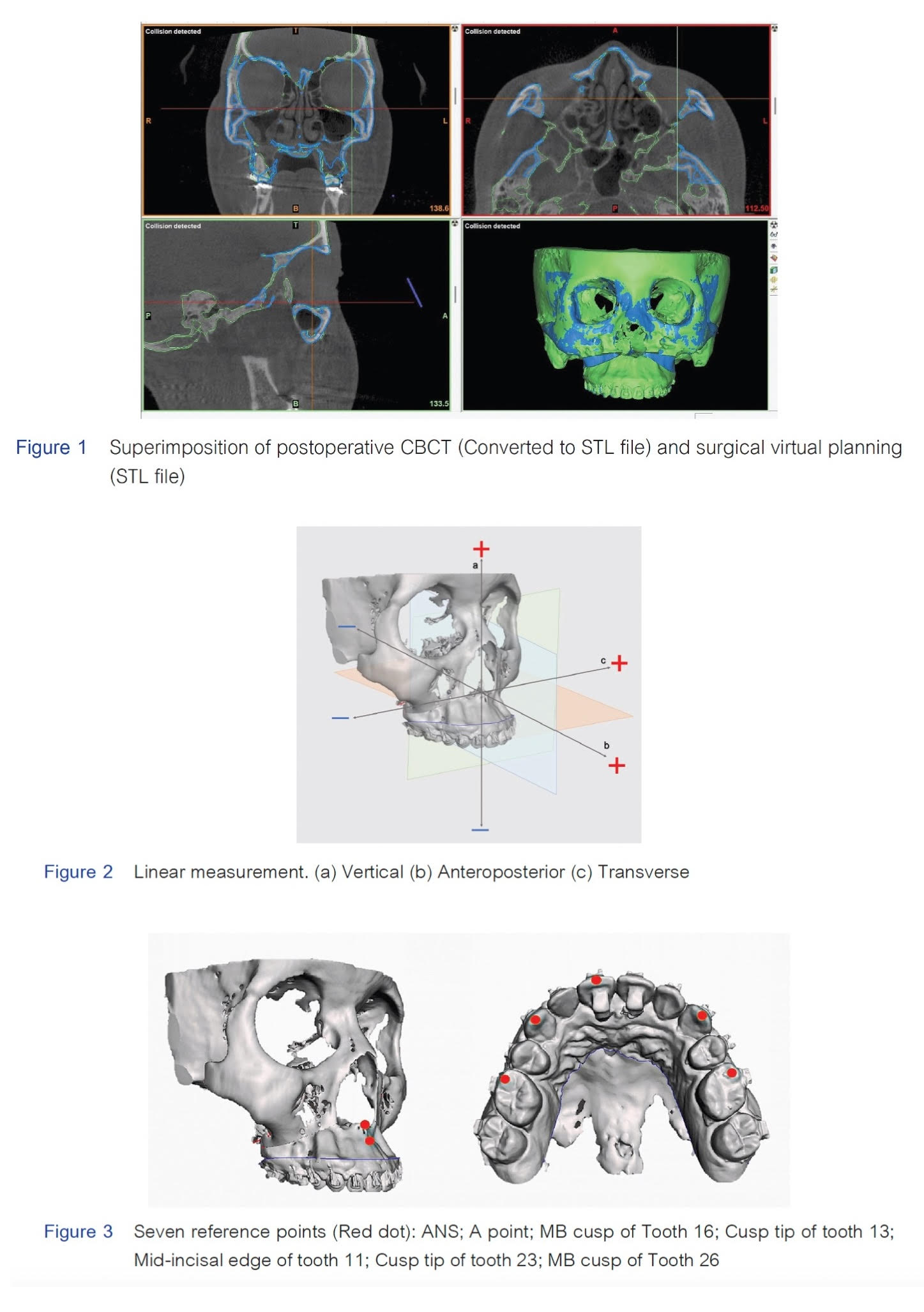
Materials and Methods: A retrospective cohort study was conducted on forty patients with skeletal asymmetry of the jaw(s) who underwent bimaxillary orthognathic surgery. The patients were evenly divided into the maxilla-first and mandible-first sequence groups. Surgical accuracy of the maxilla was determined by comparing the maxillary position in immediate postoperative cone beam computed tomography images to the simulated surgical plans. Three linear measurements using seven reference points and three angular measurements (roll, pitch, and yaw) were performed. Statistical analysis, including the independent samples t-test and the Mann-Whitney U test, was used to compare the means and medians between the two groups. The level of significance was set at p < 0.05.
Results: The accuracy of the maxilla, as measured by linear measurements, showed no significant differences between the two groups (p = 0.05–0.92). On the other hand, significant differences were observed in the roll and yaw rotations, with p-values of 0.03 and 0.04, respectively. In the anteroposterior direction, the greatest inaccuracy was found at the MB cusp of tooth 26 in the maxilla-first group (mean deviation 1.42 ± 0.86 mm) and at the MB cusp of tooth 16 in the mandible-first group (mean deviation 1.47 ± 0.79 mm).
Conclusions: The accuracy of the maxilla after bimaxillary orthognathic surgery in patients with skeletal asymmetry was comparable between the maxilla-first and mandible-first sequencing techniques. The statistically significant differences found in the roll and yaw axes were not clinically relevant. Similar postoperative accuracy and intraoperative benefits suggest that the mandible-first sequence may be the preferred technique in patients with skeletal asymmetry.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Chia MS, Naini FB, Gill DS. The aetiology, diagnosis and management of mandibular asymmetry. Ortho Update. 2008 May; 1:44-52. doi: 10.12968/ortu.2008.1.2.44.
Borikanphanitphaisan T, Ko EW. Accuracy of different sequencing in bimaxillary orthognathic surgery: A systematic review and meta-analysis. Taiwanese J Orthod. 2019 Jan; 31(1):article 2. doi: 10.30036/TJO.201903_31(1).002.
Borikanphanitphaisan T, Lin CH, Chen YA, Ko EW. Accuracy of mandible-first versus maxilla-first approach and of thick versus thin splints for skeletal position after two-jaw orthognathic surgery. Plast Reconstr Surg. 2021 Feb; 147(2):421-431. doi: 10.1097/prs.0000000000007536.
Cottrell DA, Wolford LM. Altered orthognathic surgical sequencing and a modified approach to model surgery. J Oral Maxillofac Surg. 1994 Oct; 52(10):1010-1020; discussion 1020-1021. doi: 10.1016/0278-2391(94)90164-3.
Iwai T, Omura S, Honda K, Yamashita Y, Shibutani N, Fujita K, et al. An accurate bimaxillary repositioning technique using straight locking miniplates for the mandible-first approach in bimaxillary orthognathic surgery. Odontology. 2017 Jan; 105(1):122-126. doi: 10.1007/s10266-016-0236-7
Liebregts J, Baan F, de Koning M, Ongkosuwito E, Bergé S, Maal T, et al. Achievability of 3D planned bimaxillary osteotomies: maxilla-first versus mandible-first surgery. Sci Rep. 2017 Aug; 7(1):9314. doi: 10.1038/s41598-017-09488-4
Lindorf HH, Steinhäuser EW. Correction of jaw deformities involving simultaneous osteotomy of the mandible and maxilla. J Maxillofac Surg. 1978 Nov; 6(4):239-244. doi: 10.1016/s0301-0503(78)80099-x.
Perez D, Ellis E 3rd. Sequencing bimaxillary surgery: mandible first. J Oral Maxillofac Surg. 2011 Aug; 69(8):2217-2224. doi: 10.1016/j.joms.2010.10.053
Ritto FG, Ritto TG, Ribeiro DP, Medeiros PJ, de Moraes M. Accuracy of maxillary positioning after standard and inverted orthognathic sequencing. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014 May; 117(5):567-574. doi: 10.1016/j.oooo.2014.01.016.
Salmen FS, de Oliveira TFM, Gabrielli MAC, Pereira Filho VA, Real Gabrielli MF. Sequencing of bimaxillary surgery in the correction of vertical maxillary excess: retrospective study. Int J Oral Maxillofac Surg. 2018 Jun; 47(6):708-14. doi: 10.1016/j.ijom.2017.11.007.
Stokbro K, Liebregts J, Baan F, Bell RB, Maal T, Thygesen T, et al. Does mandible-first sequencing increase maxillary surgical accuracy in bimaxillary procedures? J Oral Maxillofac Surg. 2019 Sep; 77(9):1882-1893. doi: 10.1016/j.joms.2019.03.023.
Borba AM, Borges AH, Cé PS, Venturi BA, Naclério-Homem MG, Miloro M. Mandible-first sequence in bimaxillary orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg. 2016 Apr; 45(4):472-475. doi: 10.1016/j.ijom.2015.10.008.
Perez D, Ellis E, 3rd. Implications of sequencing in simultaneous maxillary and mandibular orthognathic surgery. Atlas Oral Maxillofac Surg Clin North Am. 2016 Mar; 24(1):45-53. doi: 10.1016/j.cxom.2015.10.004
Varol C, Fındık Y, Baykul DDT, Koçer G, Şentürk MF, Yazıcı T, et al. Mandible-first sequence approach in bimaxillary orthognathic surgery using 3D printed surgical templates for facial asymmetry. Eurasia J Oral Maxillofac Surg. 2023 May; 2(2):40-1. doi:
Trevisiol L, Bersani M, Lobbia G, Scirpo R, D'Agostino A. Sequencing in orthognathic bimaxillary surgery: which jaw should be operated First? A coping review. J Clin Med. 2023 Oct; 12(21). doi: 10.3390/jcm12216826
Bozok E, Ozel A, Akkoyun EF, Dolanmaz E. Mandible-first and maxilla-first sequencing in virtual surgical planning for orthognathic surgery: comparison of planned and actual outcomes. Ear Nose Throat J. 2024 Nov; 103(3_suppl):106s-118s. doi: 10.1177/01455613241280003
Ruckman P 3rd, Schlieve T, Borba AM, Miloro M. External reference nasal pin for orthognathic maxillary positioning: What Is the proper method of placement? J Oral Maxillofac Surg. 2016 Feb; 74(2):399.e1-.e9. doi: 10.1016/j.joms.2015.10.004.
Van Sickels JE, Larsen AJ, Triplett RG. Predictability of maxillary surgery: a comparison of internal and external reference marks. Oral Surg Oral Med Oral Pathol. 1986 Jun; 61(6):542-545. doi: 10.1016/0030-4220(86)90089-7.
Stefanova N, Stella JP. The predictability of inferior medial canthus as a stable external vertical reference point in maxillary repositioning surgery. Int J Adult Orthodon Orthognath Surg. 2000 Winter; 15(4):305-308.
Bouchard C, Landry PÉ. Precision of maxillary repositioning during orthognathic surgery: a prospective study. Int J Oral Maxillofac Surg. 2013 May; 42(5):592-596. doi: 10.1016/j.ijom.2012.10.034.
Ferguson JW, Luyk NH. Control of vertical dimension during maxillary orthognathic surgery: A clinical trial comparing internal and external fixed reference points. J Craniomaxillofac Surg. 1992 Dec; 20(8):333-336. doi: 10.1016/S1010-5182(05)80360-9.
Sousa CS, Turrini RNT. Complications in orthognathic surgery: a comprehensive review. J Oral Maxillofac Surg Med Pathol. 2012 May; 24(2):67-74. doi: 10.1016/j.ajoms.2012.01.014.
Kriwalsky MS, Maurer P, Veras RB, Eckert AW, Schubert J. Risk factors for a bad split during sagittal split osteotomy. Br J Oral Maxillofac Surg. 2008 Apr; 46(3):177-179. doi: 10.1016/j.bjoms.2007.09.011.
Yamashita Y, Nakamura Y, Shimada T, Nomura Y, Hirashita A. Asymmetry of the lips of orthognathic surgery patients. Am J Orthod Dentofacial Orthop. 2009 Oct; 136(4):559-563. doi: 10.1016/j.ajodo.2007.10.057.
Zawiślak E, Przywitowski S, Olejnik A, Gerber H, Golusiński P, Nowak R. Current trends in orthognathic surgery in Poland—a retrospective analysis of 124 cases. Appl Sci. 2021 Jul; 11(14):6439. doi: 10.3390/app11146439.