Influence of preparation designs, restorative composite cements, and preheating on cementation force and cement thickness
Main Article Content
Abstract
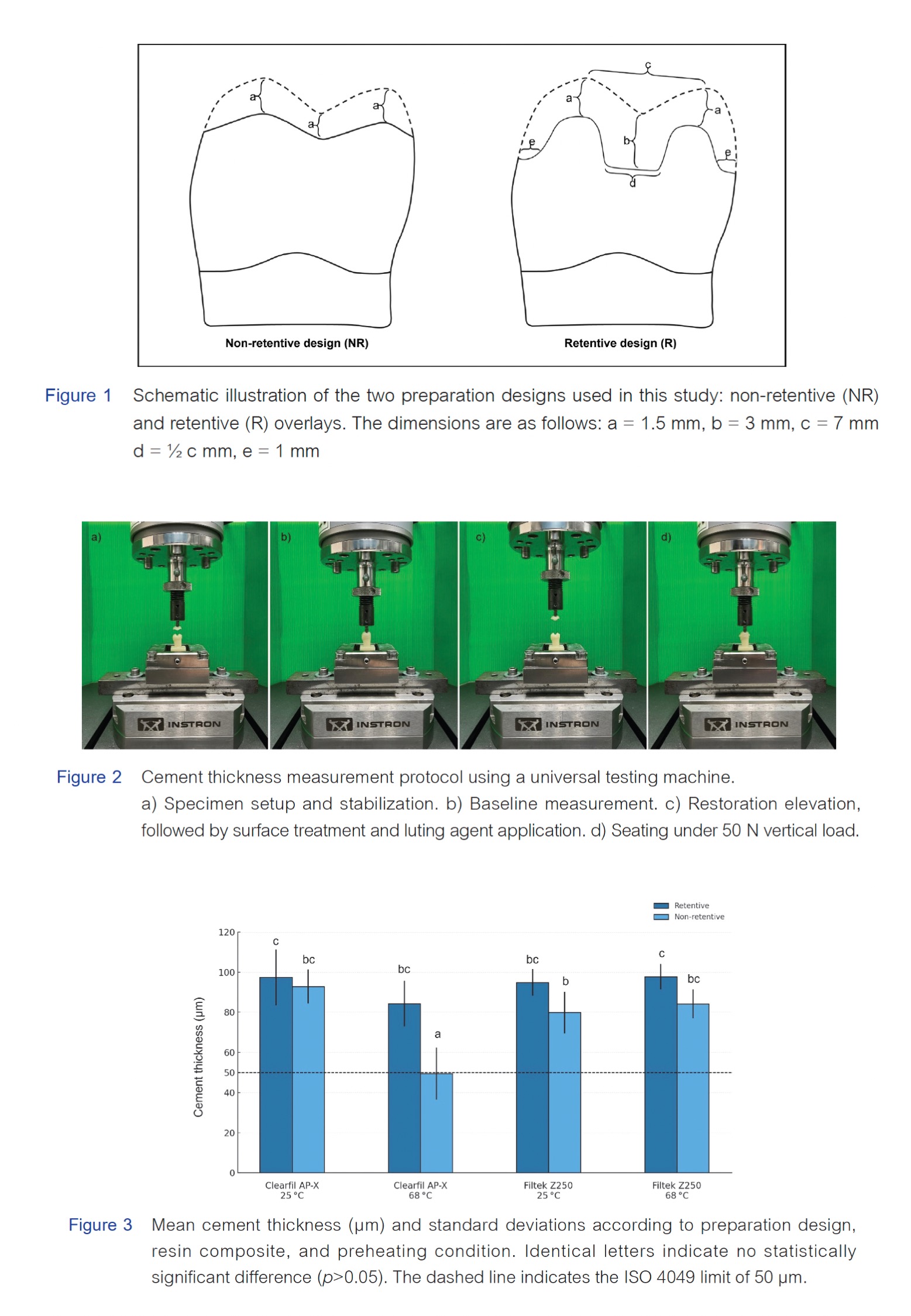
Objectives: To evaluate the effects of two ceramic overlay preparation designs and preheating of two restorative composite resins, Clearfil AP-X and Filtek Z250, on cementation force and cement thickness.
Materials and Methods:A total of 112 mandibular first molar resin dies for ceramic overlays were prepared, using either a retentive MOD design (n = 56) or a non-retentive anatomical design (n = 56). Overlays were milled from IPS e.max CAD. Specimens were divided into two groups (n = 28) for cementation force and cement thickness measurements. Each group was further subdivided by luting material (Clearfil AP-X or Filtek Z250), used at room temperature or after preheating to 68 °C for 5 minutes using a Calset device. Restorations were mounted perpendicular to the load axis on a universal testing machine. For thickness measurement, a constant vertical load of 50 N was applied, and the resulting cement thickness was measured. Cementation force was recorded as the load required to achieve a 50 μm cement thickness. Data were analyzed using three-way ANOVA followed by Tukey HSD test at a 0.05 significance level.
Results: The non-retentive design with preheated Clearfil AP-X demonstrated the lowest cement thickness (49.46 ± 12.92 μm), which was statistically significantly lower than those of the other groups (p<0.05), while other groups showed cement thicknesses ranging from 79 to 97 μm. Cementation forces ranged from 44 N to 74 N. The preheated Clearfil AP-X group, in both retentive (49.73 ± 7.74 N) and non- etentive (44.45 ± 6.92 N) designs, showed significantly lower cementation forces (p<0.05) compared to other groups.
Conclusion: Preparation design, composite type, and preheating significantly influenced cementation. The non-retentive design with preheated Clearfil AP-X showed the lowest cement thickness, approaching the 50 μm ISO threshold, and lower cementation force, highlighting the importance of material and preparation design in achieving thin film thickness and efficient seating for indirect restorations.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Manso AP, Silva NR, Bonfante EA, Pegoraro TA, Dias RA, Carvalho RM. Cements and adhesives for all-ceramic restorations. Dent Clin North Am. 2011 Apr;55(2):311–332, ix. doi:10.1016/j.cden.2011.01.012.
Krämer N, Lohbauer U, Frankenberger R. Adhesive luting of indirect restorations. Am J Dent. 2000 Nov;13(Spec No):60D–76D.
Besek M, Mörmann WH, Persi C, Lutz F. Die aushärtung von komposit unter cerec-inlays [The curing of composites under Cerec inlays]. Schweiz Monatsschr Zahnmed. 1995 Sep;105(9):1123–1128.
Barbon FJ, Isolan CP, Soares LD, Bona AD, de Oliveira da Rosa WL, Boscato N. A systematic review and meta-analysis on using preheated resin composites as luting agents for indirect restorations. Clin Oral Investig. 2022 Apr;26(4):3383–3393. doi:10.1007/s00784-022-04406-z.
Falacho RI, Marques JA, Palma PJ, Roseiro L, Caramelo F, Ramos JC, et al. Luting indirect restorations with resin cements versus composite resins: Effects of preheating and ultrasound energy on film thickness. J Esthet Restor Dent. 2022 Jun;34(4):641–649. doi:10.1111/jerd.12851.
Marcondes RL, Lima VP, Barbon FJ, Isolan CP, Carvalho MA, Salvador MV, et al. Viscosity and thermal kinetics of 10 preheated restorative resin composites and effect of ultrasound energy on film thickness. Dent Mater. 2020 Oct;36(10):1356–1364. doi:10.1016/j.dental.2020.08.004.
Politano G, Van Meerbeek B, Peumans M. Nonretentive bonded ceramic partial crowns: Concept and simplified protocol for long-lasting dental restorations. J Adhes Dent. 2018 Dec;20(6):495–510. doi:10.3290/j.jad.a41630.
Magne P, Razaghy M, Carvalho MA, Soares LM. Luting of inlays, onlays, and overlays with preheated restorative composite resin does not prevent seating accuracy. Int J Esthet Dent. 2018;13(3):318–332.
Peng CC, Chung KH, Ramos V Jr. Assessment of the adaptation of interim crowns using different measurement techniques. J Prosthodont. 2020 Jan;29(1):87–93. doi:10.1111/jopr.13122.
Ramakrishnaiah R, Alkheraif AA, Divakar DD, Matinlinna JP, Vallittu PK. The effect of hydrofluoric acid etching duration on the surface micromorphology, roughness, and wettability of dental ceramics. Int J Mol Sci. 2016 May;17(6):822. doi:10.3390/ijms17060822.
Bajraktarova-Valjakova E, Korunoska-Stevkovska V, Georgieva S, Ivanovski K, Bajraktarova-Misevska C, Mijoska A, et al. Hydrofluoric acid: Burns and systemic toxicity, protective measures, immediate and hospital medical treatment. Open Access Maced J Med Sci. 2018 Nov;6(11):2257–2269. doi:10.3889/oamjms.2018.429.
Lung CY, Matinlinna JP. Aspects of silane coupling agents and surface conditioning in dentistry: an overview. Dent Mater. 2012 May;28(5):467–477. doi:10.1016/j.dental.2012.02.009.
Torres SM, Borges GA, Spohr AM, Cury AA, Yadav S, Platt JA. The effect of surface treatments on the micro-shear bond strength of a resin luting agent and four all-ceramic systems. Oper Dent. 2009 Jul-Aug;34(4):399–407. doi:10.2341/08-87.
Matinlinna JP, Lung CYK, Tsoi JKH. Silane adhesion mechanism in dental applications and surface treatments: A review. Dent Mater. 2018 Jan;34(1):13–28. doi:10.1016/j.dental.2017.09.002.
Souza JCM, Raffaele-Esposito A, Carvalho O, Silva F, Özcan M, Henriques B. Surface modification of zirconia or lithium disilicate-reinforced glass ceramic by laser texturing to increase the adhesion of prosthetic surfaces to resin cements: an integrative review. Clin Oral Investig. 2023 Jul;27(7):3331–3345. doi:10.1007/s00784-023-05016-z.
International Organization for Standardization. Dentistry - Polymer-based restorative materials. ISO 4049:2019. Geneva: ISO; 2019.
Coelho NF, Barbon FJ, Machado RG, Boscato N, Moraes RR. Response of composite resins to preheating and the resulting strengthening of luted feldspar ceramic. Dent Mater. 2019 Oct;35(10):1430–1438. doi:10.1016/j.dental.2019.07.021.
Shobha HK, Sankarapandian M, Kalachandra S, Taylor DF, McGrath JE. Structure property relationship among novel dental composite matrix resins. J Mater Sci Mater Med. 1997 Jun;8(6):385–389. doi:10.1023/a:1018541102275.
Dionysopoulos D, Tolidis K, Gerasimou P, Koliniotou-Koumpia E. Effect of preheating on the film thickness of contemporary composite restorative materials. J Dent Sci. 2014 Dec;9(4):313–319. doi:10.1016/j.jds.2014.03.006.
Magne P, Al-Rafee M, Magne M, Carvalho MA, Milani T. Comparison of film thickness of restorative composites considered for thermo-modified cementation. J Esthet Restor Dent. 2025 Jan;37(1):28-38. doi: 10.1111/jerd.13363.
Blalock JS, Holmes RG, Rueggeberg FA. Effect of temperature on unpolymerized composite resin film thickness. J Prosthet Dent. 2006 Dec;96(6):424–432. doi:10.1016/j.prosdent.2006.09.022.
Elbishari H, Satterthwaite J, Silikas N. Effect of filler size and temperature on packing stress and viscosity of resin-composites. Int J Mol Sci. 2011 Aug;12(8):5330–5338. doi:10.3390/ijms12085330.
Lee JH, Um CM, Lee IB. Rheological properties of resin composites according to variations in monomer and filler composition. Dent Mater. 2006 Jun;22(6):515–526. doi:10.1016/j.dental.2005.05.008.
Sartori N, Peruchi LD, Phark JH, Duarte S Jr. The influence of intrinsic water permeation on different dentin bonded interfaces formation. J Dent. 2016 May;48:46–54. doi:10.1016/j.jdent.2016.03.005.
Teyagirwa PF, Aquin C, Kharouf N, Roman T, Senger B, Reitzer F, et al. Operator versus material influence on film thickness using adhesive resin cement or pre-heated resin composite. J Esthet Restor Dent. 2023 Apr;35(3):517–524. doi:10.1111/jerd.12988.
Almustafa N, Ricketts D, Chadwick G, Sauders W. Force applied by dentists during cementation of all zirconia three unit bridges and its impact on seating. Int J Dent Sci Res. 2020;8(4):112–118. doi:10.12691/ijdsr-8-4-7.
Zortuk M, Bolpaca P, Kilic K, Ozdemir E, Aguloglu S. Effects of finger pressure applied by dentists during cementation of all-ceramic crowns. Eur J Dent. 2010 Oct;4(4):383–388.
Licurci CAA, Lins L, Garbossa M, Canabarro A. A comparative study between replica and cementation techniques in the evaluation of internal and marginal misfits of single crowns. J Prosthet Dent. 2022 Apr;127(4):609–616. doi:10.1016/j.prosdent.2020.11.004.
Pinto C, Silva L, Licurci C, Canabarro A. Effect of clinical and laboratory techniques of cementation on the assessment of marginal and internal fit of prosthetic elements. Braz J Oral Sci. 2024;23:e240950. doi:10.20396/bjos.v23i00.8670950.
Falahchai M, Babaee Hemmati Y, Neshandar Asli H, Neshandar Asli M. Marginal adaptation of zirconia-reinforced lithium silicate overlays with different preparation designs. J Esthet Restor Dent. 2020 Dec;32(8):823–830. doi:10.1111/jerd.12642.
McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971 Aug;131(3):107–111. doi: 10.1038/sj.bdj.4802708.
Komine F, Iwai T, Kobayashi K, Matsumura H. Marginal and internal adaptation of zirconium dioxide ceramic copings and crowns with different finish line designs. Dent Mater J. 2007 Sep;26(5):659–664. doi:10.4012/dmj.26.659.