An overview of sleep bruxism and management, a review
Main Article Content
Abstract
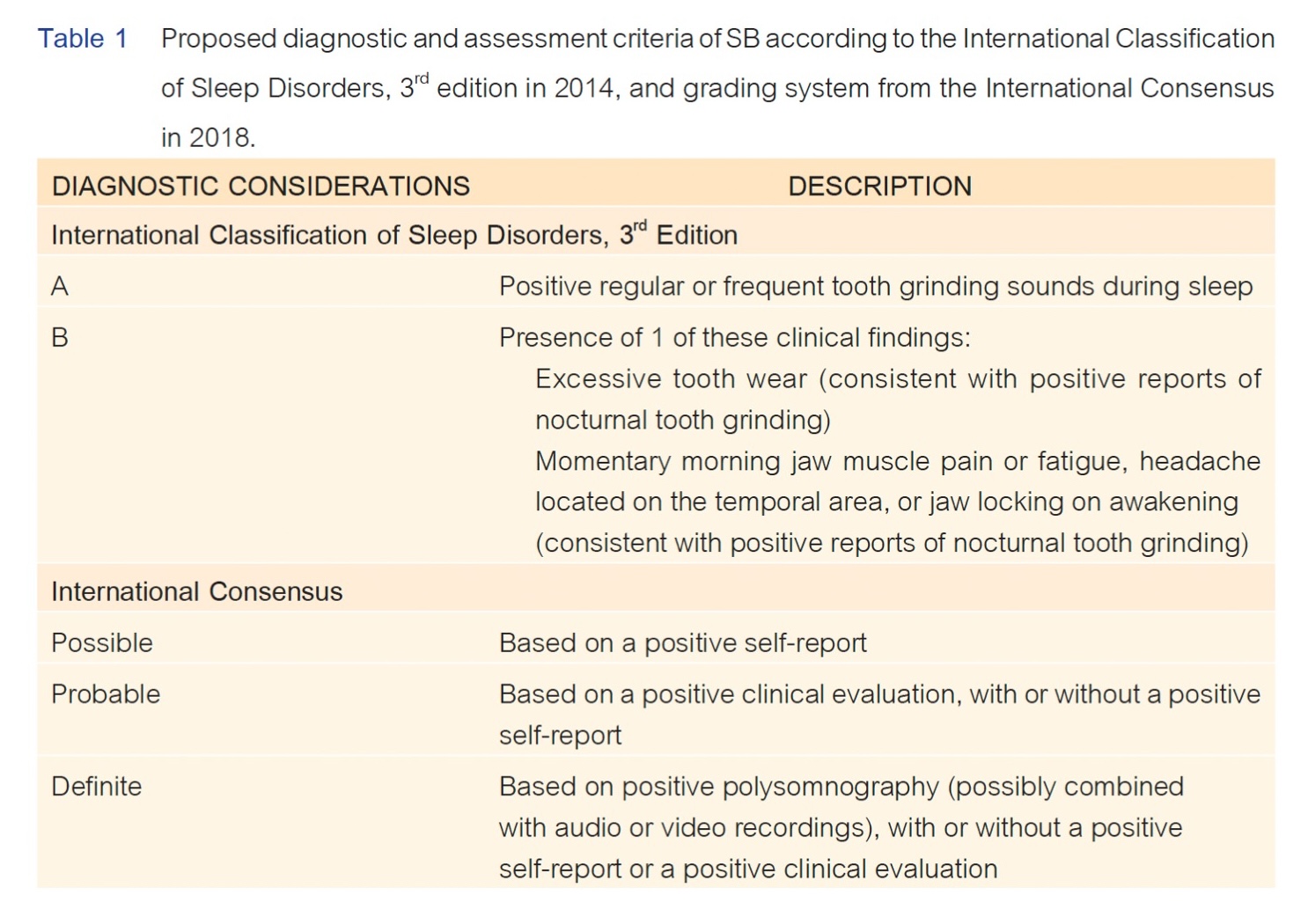
The concept of sleep bruxism (SB) has evolved over the past several decades. Many theories and hypotheses have been proposed as to the definition, pathophysiology, and management of SB. An international consensus was attained on the definition of SB as masticatory muscle activities that occur during sleep (characterized as rhythmic or non-rhythmic). The etiology of bruxism is not well known, but it is believed to be multifactorial. Assessment tools of bruxism may be made by patient report, clinical interview, clinical examination, and instrumental assessment, leading to diagnostic criteria that challenge to provision of scientifically proven information regarding SB management. Several investigations have been carried out to confirm the safety and efficacy of various kinds of treatment aimed at solving bruxism. In addition, the methodological quality, the different criteria of SB diagnosis, and the lack of homogeneity in terms of study design can result in poor meta-analysis data, mislead readers, and induce malpractice. These issues are also discussed.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, et al. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013 Jan;40(1):2-4. doi: 10.1111/joor.12011.
Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T, et al. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. 2018 Nov;45(11):837-844. doi: 10.1111/joor.12663.
Verhoeff MC, Lobbezoo F, Ahlberg J, Bender S, Bracci A, Colonna A, et al. Updating the bruxism definitions: report of an international consensus meeting. J Oral Rehabil. 2025 Sep;52(9):1335-1342. doi: 10.1111/joor.13985.
Thomas DC, Manfredini D, Patel J, George A, Chanamolu B, Pitchumani PK, et al. Sleep bruxism: The past, the present, and the future-evolution of a concept. J Am Dent Assoc. 2024 Apr;155(4):329-343. doi: 10.1016/j.adaj.2023.12.004.
Ustrell-Barral M, Zamora-Olave C, Khoury-Ribas L, Rovira-Lastra B, Martinez-Gomis J. Relationship between sleep bruxism and masticatory performance in healthy adults: A cross-sectional study. J Prosthet Dent. 2025 Sep;134(3):712-722. doi: 10.1016/j.prosdent.2025.03.029.
Manfredini D, Ahlberg J, Aarab G, Bracci A, Durham J, Emodi-Perlman A, et al. The development of the standardised tool for the assessment of bruxism (STAB): An international road map. J Oral Rehabil. 2024 Jan;51(1):15-28. doi:10.1111/joor.13380.
Johansson A, Omar R, Carlsson GE. Bruxism and prosthetic treatment: a critical review. J Prosthodont Res. 2011 Jul;55(3):127-136. doi: 10.1016/j.jpor.2011.02.004.
RAMFJORD SP. Bruxism, a clinical and electromyographic study. J Am Dent Assoc. 1961 Jan;62:21-44. doi: 10.14219/jada.archive.1961.0002.
Rugh JD, Barghi N, Drago CJ. Experimental occlusal discrepancies and nocturnal bruxism. J Prosthet Dent. 1984 Apr;51(4):548-553. doi: 10.1016/0022-3913(84)90312-3.
Ommerborn MA, Giraki M, Schneider C, Fuck LM, Handschel J, Franz M, et al. Effects of sleep bruxism on functional and occlusal parameters: a prospective controlled investigation. Int J Oral Sci. 2012 Sep;4(3):141-145. doi: 10.1038/ijos.2012.48.
Clark GT, Tsukiyama Y, Baba K, Watanabe T. Sixty-eight years of experimental occlusal interference studies: what have we learned? J Prosthet Dent. 1999 Dec;82(6):704-713. doi: 10.1016/s0022-3913(99)70012-0.
Fluerașu MI, Bocsan IC, Buduru S, Pop RM, Vesa SC, Zaharia A, et al. The correlation between sleep bruxism, salivary cortisol, and psychological status in young, caucasian healthy adults. Cranio. 2021 May;39(3):218-224. doi: 10.1080/08869634.2019.1619250.
Osses-Anguita ÁE, Sánchez-Sánchez T, Soto-Goñi XA, García-González M, Alén Fariñas F, Cid-Verdejo R, et al. Awake and sleep bruxism prevalence and their associated psychological factors in first-year university students: a pre-mid-post COVID-19 pandemic comparison. Int J Environ Res Public Health. 2023 Jan 30;20(3):2452. doi: 10.3390/ijerph20032452.
van Selms M, Kroon J, Tuomilehto H, Peltomaa M, Savolainen A, Manfredini D, et al. Self-reported sleep bruxism among Finnish symphony orchestra musicians: associations with perceived sleep-related problems and psychological stress. Cranio. 2023 Jul;41(4):323-330. doi: 10.1080/08869634.2020.1853310.
Smardz J, Martynowicz H, Wojakowska A, Michalek-Zrabkowska M, Mazur G, Wieckiewicz M. Correlation between sleep bruxism, stress, and depression—a polysomnographic study. J Clin Med. 2019 Aug;8(9):1344. doi: 10.3390/jcm8091344.
Walentek NP, Schäfer R, Bergmann N, Franken M, Ommerborn MA. Association between psychological distress and possible, probable, and definite sleep bruxism-a comparison of approved diagnostic procedures. J Clin Med. 2024 Jan;13(2):638. doi: 10.3390/jcm13020638.
Chemelo VDS, Né YGS, Frazão DR, de Souza-Rodrigues RD, Fagundes NCF, Magno MB, et al. Is there association between stress and bruxism? a systematic review and meta-analysis. Front Neurol. 2020 Dec;11:590779. doi: 10.3389/fneur.2020.590779.
Polmann H, Réus JC, Massignan C, Serra-Negra JM, Dick BD, Flores-Mir C, et al. Association between sleep bruxism and stress symptoms in adults: a systematic review and meta-analysis. J Oral Rehabil. 2021 May;48(5):621-631. doi: 10.1111/joor.13142.
Belenda González I, Montero J, Gómez Polo C, Pardal Peláez B. Evaluation of the relationship between bruxism and/or temporomandibular disorders and stress, anxiety, depression in adults: a systematic review and qualitative analysis. J Dent. 2025 May;156:105707. doi: 10.1016/j.jdent.2025.105707.
Polmann H, Domingos FL, Melo G, Stuginski-Barbosa J, Guerra ENDS, Porporatti AL, et al. Association between sleep bruxism and anxiety symptoms in adults: a systematic review. J Oral Rehabil. 2019 May;46(5):482-491. doi: 10.1111/joor.12785.
Kuang B, Li D, Lobbezoo F, de Vries R, Hilgevoord A, de Vries N, et al. Associations between sleep bruxism and other sleep-related disorders in adults: a systematic review. Sleep Med. 2022 Jan;89:31-47. doi: 10.1016/j.sleep.2021.11.008.
Doblado NG, Barrera Mora JM, Dorado FP, Fernández JCR, Ordeix GB, Escalona EE. Relationship between bruxism and obstructive sleep apnea: a systematic review of the literature. J Clin Med. 2025 Jul;14(14):5013. doi: 10.3390/jcm14145013.
Li D, Kuang B, Lobbezoo F, de Vries N, Hilgevoord A, Aarab G. Sleep bruxism is highly prevalent in adults with obstructive sleep apnea: a large-scale polysomnographic study. J Clin Sleep Med. 2023 Mar;19(3):443–451. doi: 10.5664/jcsm.10348.
Dadphan N, Chalidapongse P, Muntham D, Chirakalwasan N. Prevalence and predictors of sleep bruxism in patients with obstructive sleep apnea and the effect of positive airway pressure treatment. Sleep Breath. 2024 Jun;28(3):1119-1125. doi: 10.1007/s11325-023-02985-z.
Martynowicz H, Gac P, Brzecka A, Poreba R, Wojakowska A, Mazur G, et al. The relationship between sleep bruxism and obstructive sleep apnea based on polysomnographic findings. J Clin Med. 2019 Oct ;8(10):1653. doi: 10.3390/jcm8101653
Rintakoski K, Hublin C, Lobbezoo F, Rose RJ, Kaprio J. Genetic factors account for half of the phenotypic variance in liability to sleep-related bruxism in young adults: a nationwide finnish twin cohort study. Twin Res Hum Genet. 2012 Dec;15(6):714-719. doi: 10.1017/thg.2012.54.
Oporto GH 5th, Bornhardt T, Iturriaga V, Salazar LA. Single nucleotide polymorphisms in genes of dopaminergic pathways are associated with bruxism. Clin Oral Investig. 2018 Jan;22(1):331-337. doi: 10.1007/s00784-017-2117-z.
Strausz T, Strausz S, FinnGen, Palotie T, Ahlberg J, Ollila HM. Genetic analysis of probable sleep bruxism and its associations with clinical and behavioral traits. Sleep. 2023 Oct ;46(10):zsad107. doi: 10.1093/sleep/zsad107
Pecori A, Luppieri V, Santin A, Spedicati B, Zampieri S, Cadenaro M, et al. Clenching the strings of bruxism etiopathogenesis: association analyses on genetics and environmental risk factors in a deeply characterized italian cohort. Biomedicines. 2024 Jan;12(2):304. doi: 10.3390/biomedicines12020304
Melo G, Dutra KL, Rodrigues Filho R, Ortega AOL, Porporatti AL, Dick B, et al. Association between psychotropic medications and presence of sleep bruxism: a systematic review. J Oral Rehabil. 2018 Jul;45(7):545-554. doi: 10.1111/joor.12633.
de Baat C, Verhoeff MC, Ahlberg J, Manfredini D, Winocur E, Zweers P, et al. Medications and addictive substances potentially inducing or attenuating sleep bruxism and/or awake bruxism. J Oral Rehabil. 2021 Mar;48(3):343-354. doi: 10.1111/joor.13061.
Bertazzo-Silveira E, Kruger CM, Porto De Toledo I, Porporatti AL, Dick B, Flores-Mir C, et al. Association between sleep bruxism and alcohol, caffeine, tobacco, and drug abuse: a systematic review. J Am Dent Assoc. 2016 Nov;147(11):859-866.e4. doi: 10.1016/j.adaj.2016.06.014.
Beddis H, Pemberton M, Davies S. Sleep bruxism: an overview for clinicians. Br Dent J. 2018 Sep;225(6):497-501. doi: 10.1038/sj.bdj.2018.757.
Yachida W, Arima T, Castrillon EE, Baad-Hansen L, Ohata N, Svensson P. Diagnostic validity of self-reported measures of sleep bruxism using an ambulatory single-channel EMG device. J Prosthodont Res. 2016 Oct;60(4):250-257. doi: 10.1016/j.jpor.2016.01.001.
Ohlmann B, Rathmann F, Bömicke W, Behnisch R, Rammelsberg P, Schmitter M. Validity of patient self-reports and clinical signs in the assessment of sleep bruxism based on home-recorded electromyographic/electrocardiographic data. J Oral Rehabil. 2022 Jul;49(7):720-728. doi: 10.1111/joor.13327.
Raja HZ, Saleem MN, Mumtaz M, Tahir F, Iqbal MU, Naeem A. Diagnosis of bruxism in adults: a systematic review. J Coll Physicians Surg Pak. 2024 Oct;34(10):1221-1228. doi: 10.29271/jcpsp.2024.10.1221.
Beddis HP, Davies SJ. Relationships between tooth wear, bruxism and temporomandibular disorders. Br Dent J. 2023 Mar;234(6):422-426. doi: 10.1038/s41415-023-5584-4.
Wetselaar P, Lobbezoo F. The tooth wear evaluation system: a modular clinical guideline for the diagnosis and management planning of worn dentitions. J Oral Rehabil. 2016 Jan;43(1):69-80. doi: 10.1111/joor.12340.
Kapagiannidou D, Koutris M, Wetselaar P, Visscher CM, van der Zaag J, Lobbezoo F. Association between polysomnographic parameters of sleep bruxism and attrition-type tooth wear. J Oral Rehabil. 2021 Jun;48(6):687-691. doi: 10.1111/joor.13149.
Castroflorio T, Bargellini A, Rossini G, Cugliari G, Deregibus A, Manfredini D. Agreement between clinical and portable EMG/ECG diagnosis of sleep bruxism. J Oral Rehabil. 2015 Oct;42(10):759-764. doi: 10.1111/joor.12320.
Jonsgar C, Hordvik PA, Berge ME, Johansson AK, Svensson P, Johansson A. Sleep bruxism in individuals with and without attrition-type tooth wear: An exploratory matched case-control electromyographic study. J Dent. 2015 Dec;43(12):1504-1510. doi: 10.1016/j.jdent.2015.10.002.
Manfredini D, Ahlberg J, Aarab G, Bender S, Bracci A, Cistulli PA, et al. Standardised tool for the assessment of bruxism. J Oral Rehabil. 2024 Jan;51(1):29-58. doi: 10.1111/joor.13411.
Koyano K, Tsukiyama Y, Ichiki R, Kuwata T. Assessment of bruxism in the clinic. J Oral Rehabil. 2008 Jul;35(7):495-508. doi: 10.1111/j.1365-2842.2008.01880.x.
Holmgren K, Sheikholeslam A, Riise C. Effect of a full-arch maxillary occlusal splint on parafunctional activity during sleep in patients with nocturnal bruxism and signs and symptoms of craniomandibular disorders. J Prosthet Dent. 1993 Mar;69(3):293-297. doi: 10.1016/0022-3913(93)90109-2.
Korioth TW, Bohlig KG, Anderson GC. Digital assessment of occlusal wear patterns on occlusal stabilization splints: a pilot study. J Prosthet Dent. 1998 Aug;80(2):209-213. doi: 10.1016/s0022-3913(98)70112-x.
Onodera K, Kawagoe T, Sasaguri K, Protacio-Quismundo C, Sato S. The use of a bruxchecker in the evaluation of different grinding patterns during sleep bruxism. Cranio. 2006 Oct;24(4):292-299. doi: 10.1179/crn.2006.045.
Ustrell-Barral M, Zamora-Olave C, Khoury-Ribas L, Rovira-Lastra B, Martinez-Gomis J. The BruxChecker system for quantitatively assessing sleep bruxism at the dental level: reliability, reference values and methodological considerations. J Oral Rehabil. 2025 Jul;52(7):979–990. doi: 10.1111/joor.13959.
Lavigne G, Kato T, Herrero Babiloni A, Huynh N, Dal Fabbro C, Svensson P, et al. Research routes on improved sleep bruxism metrics: toward a standardised approach. J Sleep Res. 2021 Oct;30(5):e13320. doi: 10.1111/jsr.13320.
Manfredini D, Ahlberg J, Wetselaar P, Svensson P, Lobbezoo F. The bruxism construct: from cut-off points to a continuum spectrum. J Oral Rehabil. 2019 Nov;46(11):991-997. doi: 10.1111/joor.12833.
Jessica Vensel Rundo, Ralph Downey III. Polysomnography; In: Kerry H. Levin, Patrick Chauvel, editors. Handbook of Clinical Neurology. Volume 160. Elsevier, 2019; p.381-392.
F. Lobbezoo, G. Aarab, K. Koyano, and D. Manfredini. Assessment of sleep bruxism; In: M. Kryger, T. Roth, C. A. Goldstein, and W. C. Dement, editors. Principles and practice of sleep medicine, 7th ed. Elsevier, 2022; p.1636–1644.
Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014 Nov;146(5):1387-1394. doi: 10.1378/chest.14-0970.
Palinkas M, De Luca Canto G, Rodrigues LA, Bataglion C, Siéssere S, Semprini M, et al. Comparative capabilities of clinical assessment, diagnostic criteria, and polysomnography in detecting sleep bruxism. J Clin Sleep Med. 2015 Nov;11(11):1319-1325. doi: 10.5664/jcsm.5196.
Popescu AM, Ionescu M, Vlăduțu DE, Popescu SM, Marinescu IR, Scrieciu M, et al. Non-instrumental and instrumental tools validity in bruxism diagnostics. Diagnostics (Basel). 2025 Jan;15(2):200. doi: 10.3390/diagnostics15020200.
Soares-Silva L, de Amorim CS, Magno MB, Tavares-Silva C, Maia LC. Effects of different interventions on bruxism: an overview of systematic reviews. Sleep Breath. 2024 Jun;28(3):1465-1476. doi: 10.1007/s11325-023-02961-7.
Macedo CR, Silva AB, Machado MA, Saconato H, Prado GF. Occlusal splints for treating sleep bruxism (tooth grinding). Cochrane Database Syst Rev. 2007 Oct ;2007(4):CD005514. doi: 10.1002/14651858.CD005514.pub2
Minakuchi H, Fujisawa M, Abe Y, Iida T, Oki K, Okura K, et al. Managements of sleep bruxism in adult: a systematic review. Jpn Dent Sci Rev. 2022 Nov:58:124-136. doi: 10.1016/j.jdsr.2022.02.004.
Riley P, Glenny AM, Worthington HV, Jacobsen E, Robertson C, Durham J, et al. Oral splints for temporomandibular disorder or bruxism: a systematic review. Br Dent J. 2020 Feb;228(3):191-197. doi: 10.1038/s41415-020-1250-2.
Hardy RS, Bonsor SJ. The efficacy of occlusal splints in the treatment of bruxism: a systematic review. J Dent. 2021 May;108:103621. doi: 10.1016/j.jdent.2021.103621.
Mungia R, Lobbezoo F, Funkhouser E, Glaros A, Manfredini D, Ahlberg J, et al. Dental practitioner approaches to bruxism: preliminary findings from the national dental practice-based research network. Cranio. 2025 May;43(3):480-488. doi: 10.1080/08869634.2023.2192173.
Solanki N, Singh BP, Chand P, Siddharth R, Arya D, Kumar L, et al. Effect of mandibular advancement device on sleep bruxism score and sleep quality. J Prosthet Dent. 2017 Jan;117(1):67-72. doi: 10.1016/j.prosdent.2016.04.009.
Singh PK, Alvi HA, Singh BP, Singh RD, Kant S, Jurel S, et al. Evaluation of various treatment modalities in sleep bruxism. J Prosthet Dent. 2015 Sep;114(3):426-431. doi: 10.1016/j.prosdent.2015.02.025.
Abe S, Huynh NT, Romprß PH, de Grandmont P, Landry-Schönbeck A, Landry ML, et al. Sleep quality and comfort reported by sleep bruxism individuals wearing the occlusal splint and mandibular advancement Splint: Revisiting Two Crossover Studies. Int J Prosthodont. 2023 May;36(2):138-147. doi: 10.11607/ijp.7525.
Dal Fabbro C, Bornhardt-Suazo T, Landry Schönbeck A, de Meyer M, Lavigne GJ. Understanding the clinical management of co-occurring sleep-related bruxism and obstructive sleep apnea in adults: a narrative and critical review. J Prosthodont. 2025 Apr;34(S1):46-61. doi: 10.1111/jopr.13966.
Florjanski W, Malysa A, Orzeszek S, Smardz J, Olchowy A, Paradowska-Stolarz A, et al. Evaluation of biofeedback usefulness in masticatory muscle activity management—a systematic review. J Clin Med. 2019 May;8(6):766. doi: 10.3390/jcm8060766.
Criado L, de La Fuente A, Heredia M, Montero J, Albaladejo A, Criado JM. Electromyographic biofeedback training for reducing muscle pain and tension on masseter and temporal muscles: a pilot study. J Clin Exp Dent. 2016 Dec;8(5):e571–e576. doi: 10.4317/jced.52867.
Raphael KG, Janal MN, Sirois DA, Svensson P. Effect of contingent electrical stimulation on masticatory muscle activity and pain in patients with a myofascial temporomandibular disorder and sleep bruxism. J Orofac Pain. 2013 Winter;27(1):21-31. doi: 10.11607/jop.1029.
Conti PC, Stuginski-Barbosa J, Bonjardim LR, Soares S, Svensson P. Contingent electrical stimulation inhibits jaw muscle activity during sleep but not pain intensity or masticatory muscle pressure pain threshold in self-reported bruxers: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014 Jan;117(1):45-52. doi: 10.1016/j.oooo.2013.08.015.
Jadidi F, Castrillon E, Svensson P. Effect of conditioning electrical stimuli on temporalis electromyographic activity during sleep. J Oral Rehabil. 2008 Mar;35(3):171-183. doi: 10.1111/j.1365-2842.2007.01781.x.
Amorim CSM, Espirito Santo AS, Sommer M, Marques AP. Effect of physical therapy in bruxism treatment: a systematic review. J Manipulative Physiol Ther. 2018 Jun;41(5):389-404. doi: 10.1016/j.jmpt.2017.10.014.
Valiente López M, van Selms MK, van der Zaag J, Hamburger HL, Lobbezoo F. Do sleep hygiene measures and progressive muscle relaxation influence sleep bruxism? report of a randomised controlled trial. J Oral Rehabil. 2015 Apr;42(4):259-265. doi: 10.1111/joor.12252.
Blitzer A, Sulica L. Botulinum toxin: basic science and clinical uses in otolaryngology. Laryngoscope. 2001 Feb;111(2):218-226. doi: 10.1097/00005537-200102000-00006.
Fernández-Núñez T, Amghar-Maach S, Gay-Escoda C. Efficacy of botulinum toxin in the treatment of bruxism: systematic review. Med Oral Patol Oral Cir Bucal. 2019 Jun;24(4):e416–e424. doi: 10.4317/medoral.22923.
Malcangi G, Patano A, Pezzolla C, Riccaldo L, Mancini A, Di Pede C, et al. Bruxism and botulinum injection: challenges and insights. J Clin Med. 2023 Jul;12(14):4586. doi: 10.3390/jcm12144586.
Ågren M, Sahin C, Pettersson M. The effect of botulinum toxin injections on bruxism: a systematic review. J Oral Rehabil. 2020 Mar;47(3):395-402. doi: 10.1111/joor.12914.
Yacoub S, Ons G, Khemiss M. Efficacy of botulinum toxin type A in bruxism management: a systematic review. Dent Med Probl. 2025 Jan-Feb;62(1):145-160. doi: 10.17219/dmp/186553.
Rafferty KL, Liu ZJ, Ye W, Navarrete AL, Nguyen TT, Salamati A, et al. Botulinum toxin in masticatory muscles: short- and long-term effects on muscle, bone, and craniofacial function in adult rabbits. Bone. 2012 Mar;50(3):651-662. doi: 10.1016/j.bone.2011.11.015.
Raphael KG, Janal MN, Tadinada A, Santiago V, Sirois DA, Lurie AG. Effect of multiple injections of botulinum toxin into painful masticatory muscles on bone density in the temporomandibular complex. J Oral Rehabil. 2020 Nov;47(11):1319-1329. doi: 10.1111/joor.13087.
Wojtovicz EL, Alvarez OM, Lopez-Davis A, Armijo-Olivo S. Botulinum toxin type a injection into the masticatory muscles and its effects on mandibular bone resorption and density. a systematic review. Clin Oral Investig. 2024 Aug;28(9):477. doi: 10.1007/s00784-024-05838-5.
Cerón L, Pacheco M, Delgado Gaete A, Bravo Torres W, Astudillo Rubio D. Therapies for sleep bruxism in dentistry: a critical evaluation of systematic reviews. Dent Med Probl. 2023 Apr-Jun;60(2):335-344. doi: 10.17219/dmp/156400.