Development of a Patient Empowerment Program to Promote Effective Breathing Capacity in Gynecological Patients at Risk of Ineffective Breathing after Abdominal Surgery
Main Article Content
Abstract
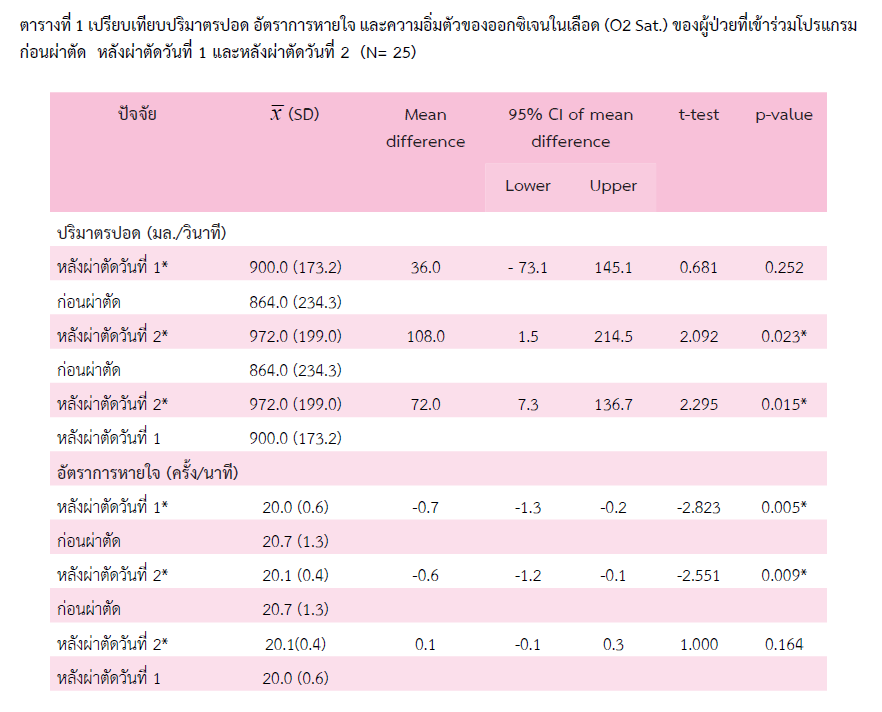
Effective breathing reduces the problems during the recovery process for patients after surgery. This study shows that a patient empowerment program to promote effective breathing capacity in gynecological patients at risk of ineffective breathing after abdominal surgery could reduce the risk of respiratory complications and promote better recovery. The patient empowerment program includes a variety of actions and engagement, from assessing the patient's risk of ineffective breathing and encouraging positive interactions between nurses and patients while teaching patients how to practice effective breathing techniques to the effects of abdominal surgery on effective breathing. Teach patients proper breathing techniques and how to measure lung capacity with lung exercise equipment such as an incentive spirometer (Triflo). Encourage patients to practice continuous, effective breathing without stimulation. Identify and resolve the problems that prevent patients from using lung exercise equipment. The nurse uses a participatory and active teaching method to train the patients on the breathing exercise until they can do it flawlessly on their own. Keep a record of the patient's spirometry test, as it is an indicator of the patient's ability to breathe effectively. This study showed that the patients in the empowerment program could breathe effectively on day 1 and day 2 after surgery, with a mean lung volume of 900.0±173.2 ml/s and 972.0±199.0, respectively. This patient empowerment program demonstrates that encouraging postoperative patients to breathe more effectively is one of the methods for reducing the risk of respiratory complications and promoting better recovery among gynecological patients after surgery.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Statistic Report 2018: Siriraj Hospital [Statistical Report]: Division of Medical Record, Siriraj Hospital. Faculty of Medicine Siriraj Hospital, Mahidol University; 2019. Available from: https://www.si.mahidol.ac.th/office_h/medrecord/stunit/PDF/Statistical%20report%202018.pdf.
Meleis AI, Sawyer LM, Im EO, Hilfinger Messias DK, Schumacher K. Experiencing transitions: an emerging middle-range theory. ANS Adv Nurs Sci. 2000 Sep;23(1):12-28.
Westerdahl E. Optimal technique for deep breathing exercises after cardiac surgery. Minerva Anestesiol. 2015 Jun;81(6):678-83.
Suaroo P. Risk factors in prolonged use of mechanical ventilators in postoperative abdominal surgery patients. JTMNC. 2015;30:107-20.
Rattanakanlaya K. Coaching on breathing exercise by applying incentive spirometer in postoperative patients. JRTAN. 2018;19:1-8.
Ngamprasert M, Utriyaprasit K, Sindhu S, Ratinthorn A, Viwatwongkasem C. The relationship among a palliative care service, patient’s factors, and quality of life of post treatment cervical cancer patients: a causal model approach. Siriraj Med J. 2019;71(4):268-77.
Opaspasu A, Trisarawat P, Kongamnoiysak U, Buranapuntalug S. The immediate effects of costal breathing exercise with sustained maximal inspiration technique and flow incentive spirometer on chest expansion in sedentary young adults. TMJ. 2016;16(2):220-9.
Ubolsakka-Jones C PhD PT, Tasangkar W Msc PT, Jones DAP. Comparison of breathing patterns, pressure, volume, and flow characteristics of three breathing techniques to encourage lung inflation in healthy older people. Physiotherapy theory and practice. 2019 Dec;35(12):1283-91.
Mayr U, Karsten E, Lahmer T, Rasch S, Thies P, Henschel B, et al. Impact of large volume paracentesis on respiratory parameters including transpulmonary pressure and on transpulmonary thermodilution derived hemodynamics: A prospective study. PLoS One. 2018;13(3):e0193654. PubMed PMID: 29538440.
Chokmoh K, Saensom D. Incidence and factors predicting respiratory complications after 48 hours of general anesthesia. Nurs Sci J Thai. 2022;40(4):17-3211.
วรรณพร ทองประมูล. การศึกษาปัจจัยที่มีความสัมพันธ์กับการเกิดภาวะความอิ่มตัวของออกซิเจนต่ำในผู้ป่วยที่ได้รับยาระงับความรู้สึกเพื่อการผ่าตัดใน ห้องพักฟื้น โรงพยาบาลนครนายก. NJPH. 2016;25(3):120-31
Moustafa AAM, Abdelazim IA. Impact of obesity on recovery and pulmonary functions of obese women undergoing major abdominal gynecological surgeries. J Clin Monit Comput. 2016;30(3):333-9.
Hunsicker O, Fotopoulou C, Pietzner K, Koch M, Krannich A, Sehouli J, et al. Hemodynamic consequences of malignant ascites in epithelial ovarian cancer surgery : a prospective substudy of a randomized controlled trial. Medicine (Baltimore). 2015;94(49):e2108-e.
Matos CMP, Moraes KS, França DC, Tomich GM, Farah MW, Dias RC, et al. Changes in breathing pattern and thoracoabdominal motion after bariatric surgery : a longitudinal study. Respiratory physiology & neurobiology. 2012;181(2):143-7.
Rattanakanlaya K. Coaching on breathing exercise by applying Incentive spirometer in postoperative patients. JRTAN. 2018;19.
Shuleeporn V, Punyanuch C. Information needs and received in preoperative patients for gynecologic surgery. JFONUBUU. 2017;25(4):51-9.
Duranti R, Laffi G, Misuri G, Riccardi D, Gorini M, Foschi M, et al. Respiratory mechanics in patients with tense cirrhotic ascites. Eur Respir J. 1997 Jul;10(7):1622-30.