แบบแผนความเชื่อด้านสุขภาพที่มีความสัมพันธ์กับพฤติกรรมการดูแลตนเอง เพื่อป้องกันโรคหลอดเลือดสมองของผู้ป่วยที่ไม่สามารถควบคุมความดันโลหิตได้ โรงพยาบาลนภาลัย จังหวัดสมุทรสงคราม
บทคัดย่อ
การวิจัยนี้มีวัตถุประสงค์เพื่อศึกษาแบบแผนความเชื่อด้านสุขภาพที่มีความสัมพันธ์กับพฤติกรรมการดูแลตนเองเพื่อป้องกันโรคหลอดเลือดสมองของผู้ป่วยความดันโลหิตสูงที่ไม่สามารถควบคุมได้ โรงพยาบาลนภาลัย จังหวัดสมุทรสงคราม จำนวน 351 คน เก็บรวบรวมข้อมูลโดยแบบสอบถามที่ผู้วิจัยสร้างขึ้นมีค่า CVI เท่ากับ 0.89 มีค่าความเที่ยงสัมประสิทธิ์แอลฟาของครอนบาค เท่ากับ 0.86 – 0.89 รวบรวมข้อมูลระหว่างเดือนธันวาคม 2564 ถึงกุมภาพันธ์ 2565 วิเคราะห์ข้อมูลโดยใช้สถิติเชิงพรรณนา และสัมประสิทธิ์สหสัมพันธ์โดย Pearson’s product moment correlation coefficient
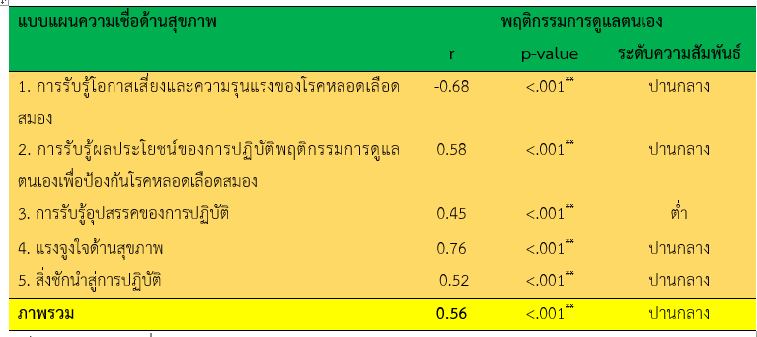
ผลการศึกษา พบว่า พฤติกรรมการดูแลสุขภาพตนเองเพื่อป้องกันโรคหลอดเลือดสมองของผู้ป่วยความดันโลหิตสูงที่ไม่สามารถควบคุมได้ โดยรวมอยู่ในระดับปานกลาง (M= 3.55, S.D.= 0.55) การรับรู้โอกาสเสี่ยงและความรุนแรงของโรคมีความสัมพันธ์ทางลบกับพฤติกรรมการดูแลสุขภาพตนเองเพื่อป้องกันโรคหลอดเลือดสมองของผู้ป่วยความดันโลหิตสูงที่ไม่สามารถควบคุมได้ (r= -0.68, p < 0.01) การรับรู้ถึงผลประโยชน์การป้องกันโรค การรับรู้อุปสรรคการปฏิบัติตน แรงจูงใจด้านสุขภาพ สิ่งชักนำสู่การปฏิบัติ และภาพรวมมีความสัมพันธ์ทางบวกกับพฤติกรรมการดูแลสุขภาพตนเองเพื่อป้องกันโรคหลอดเลือดสมองของผู้ป่วยความดันโลหิตสูงที่ไม่สามารถควบคุมได้ (r= 0.58, 0.45, 0.76, 0.51 และ 0.56, p < 0.01)
ควรมีการจัดกิจกรรมถ่ายทอดประสบการณ์ โปรแกรมปรับเปลี่ยนพฤติกรรมสุขภาพให้กับผู้ป่วยที่ไม่สามารถควบคุมความดันโลหิตได้เพื่อป้องกันโรคหลอดเลือดสมอง โดยเน้นให้เห็นถึงประโยชน์และอุปสรรคในการป้องกันโรคและร่วมกันหาแนวทางการป้องกันโรค
เอกสารอ้างอิง
Adams, A. G., Schweitzer, D., Molenberghs, P., & Henry, J. D. (2019). A meta-analytic review of social cognitive function following stroke. Neuroscience and Biobehavioral Reviews, 102, 400–416. https://doi.org/10.1016/j.neubiorev.2019.03.01.
Banyen, B., Sudta, W. (2020). Perception of stroke in hypertensive patients Makhamlom Sub- District, Suphan Buri Province. Journal of Safety and Health, 13(1), 93-101.
Becker, M. H. (1974). The health belief model and sick role behavior. In M. H. Becker (Ed.), The health belief model, and personal health behavior (pp.82-92). New York: Charles B. Slack.
Benjamin, E. J., Blaha, M. J., Chiuve, S. E., Cushman, M., Das, S. R., & Deo, R., et al. (2017). American heart association statistics committee and stroke statistics subcommittee, heart disease and stroke statistics-2017 update: A report from the american heart association. Circulation, 135(10), e146–e603. https://doi.org/10.1161/CIR.0000000000000485
Boehme, A. K, Esenwa, C, & Elkind, M. S. (2017). Stroke risk factors, genetics, and prevention. Circulation Research, 120(3), 472-495.
Brunner, L. S. (2010). Brunner & Suddarth’s textbook of medical-surgical nursing. (12ed). Vol. 1. 2010: Lippincott Williams & Wilkins.
Cummings, D. M., Letter, A. J., Howard, G., Howard, V. J., Safford, M. M., & Prince, V., et al. (2013). Medication adherence and stroke/TIA risk in treated hypertensives: Results from the regards study. Journal of the American Society of Hypertension, 7(5), 363–369. http://doi.org/10.1016/j.jash.2013.05.002.
Division of Non-Communicable Disease. (2020). Annual report 2020. Nonthaburi: The Office of Disease Prevention and Control. (in Thai)
Duangkaew, T., & Sirasoonthorn, P. (2017). An application of marshall H. Becker’s health belief model [HBM] in the study of hypertension patients in urban communities in Phitsanulok. Naresuan University Journals, 10(3), 101-113. (in Thai)
Feigin, V. L., Lawes, C. M., Bennett, D. A., Barker-Collo, S. L., & Parag, V. (2009). Worldwide stroke incidence and early case fatality reported in 56 population-based studies: A systematic review. The Lancet. Neurology, 8(4), 355–369. https://doi.org/10.1016/S1474-4422(09)70025-0.
Jangwang, S., Pittayapinune, T., & Chutipattana, N. (2017). Factors related to self-care behavior for prevention of diabetes mellitus and hypertension among population groups at risk. The Southern College Network Journal of Nursing and Public Health, 3(1), 110-128. (in Thai).
Krejcie, R. V. & Morgan, D. W. (1970). Determining sample size for research activities. Educational and Psychological Measurement, 30(3), pp. 607-610.
Lahkum, S., & Intaranongpai, S. (2017). Relationship between health belief perception and stroke prevention behavior in high risk patients in Nuea Mueang Sub District, Mueang District, Roiet Province. Journal Of the police Nurse, 9(2), 85-94.
Li, C., Engström, G., Hedblad, B., Berglund, G., & Janzon, L. (2005). Blood pressure control and risk of stroke: A population-based prospective cohort study. Stroke, 36(4), 725–730. https://doi.org/10.1161/01.STR.0000158925.12740.87
Li, J., Yang, S. C., Moullaali, T. J., Chen, R., Woodward, M., & Carcel, C., et al. (2019). Sex differences in blood pressure after stroke: A systematic review and meta-analysis. Journal of hypertension, 37(10), 1991–1999. http://doi.org/10.1097/HJH.0000000000002116.
Loussug W, Lawang W, & Homsin P. (2019). The effects of application of the health belief model with family support program on preventive behaviors against cerebrovascular disease among individual at risk. Journal of Nursing and Education, 12(4), 32-45.
Muanmee, W. (2017). Factor influencing preventive behavior for cerebrovascular disease among hypertensive patients in Bangrakam district, phitsanulok. Master of Nursing Science Thesis (Community Nurse Practitioner), Naresuan university. (in Thai)
Ministry of Public Health, Strategy and Planning Division Office of the Permanent Secretary. (2020). Public health statistics A.D. 2019 [Internet]. 2022 [cited 2020 April 1]. Available from: https://bps.moph.go.th/new_bps/sites/default/files/statistic62.pdf. (in Thai)
Napalai Hospital Center. (2021). A report non-communicable disease from division of non- communicable disease 2019-2020 from Napalai Hospital, Samut Songkhram. (in Thai)
O'Donnell, M. J., Chin, S. L., Rangarajan, S., Xavier, D., Liu, L., & Zhang, H., et al. (2016). Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (Interstroke): A case-control study. Lancet (London, England), 388(10046), 761–775. https://doi.org/10.1016/S0140-6736(16)30506-2.
Owolabi, M. O., & Agunloye, A. M. (2013). Risk factors for stroke among patients with hypertension: A case-control study. Journal of the Neurological Sciences, 325(1-2), 51–56. https://doi.org/10.1016/j.jns.2012.11.016.
Palitnonkert, A., Sriarun, J., Chadlee, N., Jantong, T., Janpurm, A., Chaisunan, C., & Pumpothong, S., et al. (2018). Health belief model related to self-care behavior of patients with hypertension at Bangsamak Sub-District Health Promoting Hospital, Bangpakong District, Chachoengsao Province. Apheit Humanities and Social Sciences Journal, 7(2), 43-52.
Polit, D. F. & Beck, C. T. (2012). Nursing research: Generatingand assessing evidence for nursing practice. (8th ed). New York: J.B. Lippincott.
Ponchaimat, C. & Sangkeang, S. (2020). Factors associated with health care behavior of hypertensive patients in the elderly club in Bang Nok Khwaek Sub-district, Bang Khonthi, Samut Songkhra. Interdisciplinary Management Journal Faculty Of Management Science, Buriram Rajabhat University, 3(1), 65-70.
Purateeranrath, P. & Wongpiriyayothar, A. (2019). The relationships between health beliefs and health behaviors among essential hypertention patients of hypertension clinic, Surin Hospital. Medical Journal of Srisaket Surin Buriram Hospital, 34(2), 257-272.
Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education Quarterly, 15(2), 175-183
Ruangchaithaweesuk, K., Watcharanurak, P. & Klubklay, A. (2021). Factors influencing preventive behavior among stoke-risk patients in Songkhla Province. The Southern College Network Journal of Nursing and Public Health, 4(1), 217-233.
Silberberg, D., Anand, N. P., Michels, K., & Kalaria, R. N. (2019). Brain and other nervous system disorders across the lifespan-global challenges and opportunities. Nature, 527(7578), S151–S154. https://doi.org/10.1038/nature16028.
Singco, T., Changmai, S., & Toskullkao, T. (2020). The effects of promoting perception of health beliefs program on stroke preventive behaviors and perceived benefit of sustained behaviors in elderly at risk. Journal of Charoenkrung Pracharak Hospital, 16(2), 43-60.
Siritawee, C., Iemsadikul, W., & Nuysr, M. (2018). Effects of a health behaviors developing program for hypertension patients at Rattanaburi. Research and Development Health System Journal, 13(2), 307-317.
World Stroke Organization. (2019). Annual reports 2019 [Internet]. 2019 [cited 2022 April 14]. Available from: http://www.world-stroke.org/about-wso/annual-reports. (in Thai)
Yoopan, N., Duangchan, P., & Jampole, P. (2017). Relationships among social support, health beliefs, self-care behaviors and blood pressure of hypertensive. Thai Pharmaceutical and Health Science Journal, 10(1). 75-90.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2022 วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของ วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช และบุคคลากรท่านอื่น ๆ ในวิทยาลัยฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว