การพัฒนาโปรแกรมการให้ข้อมูลผู้สูงอายุก่อนการให้ยาระงับความรู้สึก โดยการใช้สื่อมัลติมีเดียด้วยภาพแอนนิเมชั่นร่วมกับ QR Code เพื่อเพิ่มความรู้ ความพึงพอใจ และลดความวิตกกังวล
คำสำคัญ:
ความรู้, การปฏิบัติตัว, การสอนด้วยสื่อมัลติมีเดียด้วยภาพแอนนิเมชันบทคัดย่อ
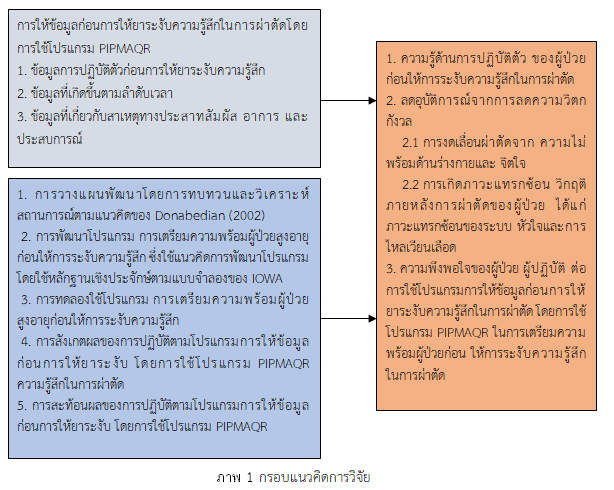
การวิจัยและพัฒนานี้มีวัตถุประสงค์เพื่อเปรียบเทียบความรู้ และความวิตกกังวลของผู้ป่วยที่ได้รับการให้ยาระงับความรู้สึกก่อนและหลังการสอนโดยใช้โปรแกรมการให้ข้อมูลร่วมกับการใช้สื่อมัลติมีเดียด้วยแอนนิเมชันร่วมกับ QR code หรือ Pre-anesthesia information program by using multimedia with animation and QR code (PIPMAQR) กลุ่มตัวอย่างเป็นผู้ป่วยผ่าตัดที่ได้รับการให้ยาระงับความรู้สึกในเวลาราชการ ได้รับการสุ่มโดยคอมพิวเตอร์ตามเกณฑ์ที่กำหนดเพื่อเข้ากลุ่มที่ได้รับโปรแกรมการให้ข้อมูลร่วมกับการใช้สื่อมัลติมีเดียด้วยแอนนิเมชันร่วมกับ QR Code และผู้ป่วยที่ได้รับการพยาบาลตามมาตรฐาน การศึกษาแบ่งเป็น 4 ระยะ คือ 1) วิจัย 2) พัฒนา 3) วิจัย และ 4) ปรับปรุง เครื่องมือที่ใช้วิจัย ได้แก่ แบบสอบถามข้อมูลส่วนบุคคล แบบแผนการเยี่ยมก่อนผ่าตัดโดยการให้ยาระงับความรู้สึกประกอบด้วยโปรแกรม PIPMAQR ตรวจสอบคุณภาพเครื่องมือโดยผู้ทรงคุณวุฒิ 3 ท่าน ได้ค่า CVI เท่ากับ 0.86 แบบวัดความรู้ได้ค่าความเชื่อมั่น เท่ากับ 0.86 และแบบวัดความความวิตกกังวลของผู้ป่วยโดยใช้ Trait Anxiety, A-trait (STAI Form Y-2) ค่าความเชื่อมั่น เท่ากับ 0.81 วิเคราะห์ข้อมูลด้วยสถิติ ร้อยละ ค่าเฉลี่ย ส่วนเบี่ยงเบนมาตรฐาน และ Independent t-test หลังการใช้โปรแกรม PIPMAQR คะแนนเฉลี่ยของความรู้เกี่ยวกับการปฏิบัติตัวก่อนการให้ยาระงับความรู้สึกเพิ่มขึ้นอย่างมีนัยสำคัญทางสถิติที่ (p < 0.001) คะแนนเฉลี่ยของความวิตกกังวลลดลงอย่างมีนัยสำคัญทางสถิติที่ (p < 0.001)
ข้อเสนอแนะ หน่วยงานที่มีผู้ป่วยควรนำโปรแกรม PIPMAQR ไปใช้กับผู้ป่วยเพื่อเพิ่มความรู้ และลดความวิตกกังวล ก่อนการผ่าตัด รวมถึงหน่วยงานอื่นที่มีลักษณะคล้ายกันสามารถนำไปใช้พัฒนาต่อยอดได้ และควรใช้โปรแกรม PIPMAQR โดยผ่านทาง You tube ในการเตรียมผู้ป่วยที่เข้ารับการผ่าตัดโดยผู้ป่วยสามารถเข้าดูเนื้อหาที่ให้ความรู้เกี่ยวกับข้อมูลก่อนการให้ยาระงับความรู้สึกได้ตามความสะดวก และสามารถแชร์ให้ผู้ที่สนใจต่อได้
เอกสารอ้างอิง
Bandura, A. (2002). Social cognitive theory in cultural context. Applied Psychology, 51(2), 269-290.
Chu, C. L., Chiou, H. Y., Chou, W. H., Chang, P. Y., Huang, Y. Y., & Yeh, H. M. (2017). Leading Comorbidity associated with 30-day post-anesthetic mortality in geriatric surgical patients in Taiwan: a retrospective study from the health insurance data. BMC Geriatrics, 17, 1-10.
Donabedian, A. (2002). An introduction to quality assurance in health care. Oxford University Press.
Fowler, A. J., Abbott, T. E. F., Prowle, J., & Pearse, R. M. (2019). Age of patients undergoing surgery. Journal of British Surgery, 106(8), 1012-1018.
González-Arévalo, A., Gómez-Arnau, J. I., delaCruz, F. J., Marzal, J. M., Ramírez, S., Corral, E. M., et al. (2009). Causes for cancellation of elective surgical procedures in a Spanish general hospital. Anaesthesia, 64(5), 487–493.
Gonzalez-Bautista, E., Morsch, P., Mathur, M., Bós, Â. J. G., Hommes, C., & Vega, E. (2021). Assessing health system responsiveness to the needs of older people. Revista Panamericana de Salud Pública, 45.
Hastings, J. T., Bloom, B. S., Madaus, G. F., & Hastings, J. T. (Eds.). (1971). Handbook on formative and summative evaluation of student learning. New York: MacGraw-Hill.
Hawes, R. H., Andrzejowski, J. C., Goodhart, I. M., Berthoud, M. C., & Wiles, M. D. (2016). An evaluation of factors influencing the assessment time in a nurse practitioner‐ led anaesthetic pre‐operative assessment clinic. Anaesthesia, 71(3), 273-279.
Johnson, J. E., & Leventhal, H. (1974). Effects of accurate expectations and behavioral instructions on reactions during a noxious medical examination. Journal of Personality and Social Psychology, 29(5), 710.
Khamwicha, P. (1991). Effects of exposure on anxiety of preoperative patients. Mahidol University. Bangkok. DOI: https://www.doi.nrct.go.th/ListDoi/listDetail?Resolve_
Kumar, R., & Gandhi, R. (2012). Reasons for cancellation of operation on the day of intended surgery in a multidisciplinary 500 bedded hospital. Journal of Anesthesiology, Clinical Pharmacology, 28(1), 66.
Mayer, R. E. (2009). Multimedia learning (2nd ed.). New York: Cambridge University Press.
Partridge, J. S. L., Harari, D., Martin, F. C., & Dhesi, J. K. (2014). The impact of pre‐ operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia, 69, 8-16.
Srijan, J. Kaveevivitchai, C. Neelapaichit, N. & Chantadansawan, T. (2018). Effects of self-efficacy-promoting program with cartoon animation videos on knowledge, anxiety, and perceived self-efficacy in patients undergoing cardiac catheterization. The Journal of Thailand and Midwifery Nursing Council, 33(1), 89-102.
Srisathitnarakoon, B. (2007). The methodology in nursing research. (4th ed.). Bangkok: Faculty of Nursing Chulalongkorn University.
Statistics from Lampang Hospital Statistical Center, 2018. (2018). Statistics of Lampang Hospital. Lampang.
Thorndike, E. L. (1991). The psychology of the school dictionary. International Journal of Lexicography, 4(1), 15-22.
Titler, M. G., Kleiber, C., Steelman, V. J., Rakel, B. A., Budreau, G., Everett, L. Q., et al. (2001). The Iowa model of evidence-based practice to promote quality care. Critical Care Nursing Clinics of North America, 13(4), 497–509.
Tung, A., Dexter, F., Jakubczyk, S., & Glick, D. B. (2010). The limited value of sequencing cases based on their probability of cancellation. Anesthesia & Analgesia, 111(3), 749-756.
Waller, A., Forshaw, K., Carey, M., Robinson, S., Kerridge, R., Proietto, A., et al. (2015). Optimizing patient preparation and surgical experience using e-health technology. JMIR Medical Informatics, 3(3), e29.
Wewer, M. E & Lowe, N. K. (1990). A critical review of visual analogue scales in measurement of clinical phenomena. Nurs Health; 13:227-36.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2023 วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของ วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช และบุคคลากรท่านอื่น ๆ ในวิทยาลัยฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว