ผู้ป่วยโรคโควิด-19 เกิดภาวะเลือดออกใต้ผิวหนังขนาดใหญ่หลังได้รับยากลุ่มเฮพารินที่มีน้ำหนักโมเลกุลต่ำ
คำสำคัญ:
โควิด-19, อีน็อคซาพาริน, เฮพาริน, ยากลุ่มเฮพารินที่มีน้ำหนักโมเลกุลต่ำบทคัดย่อ
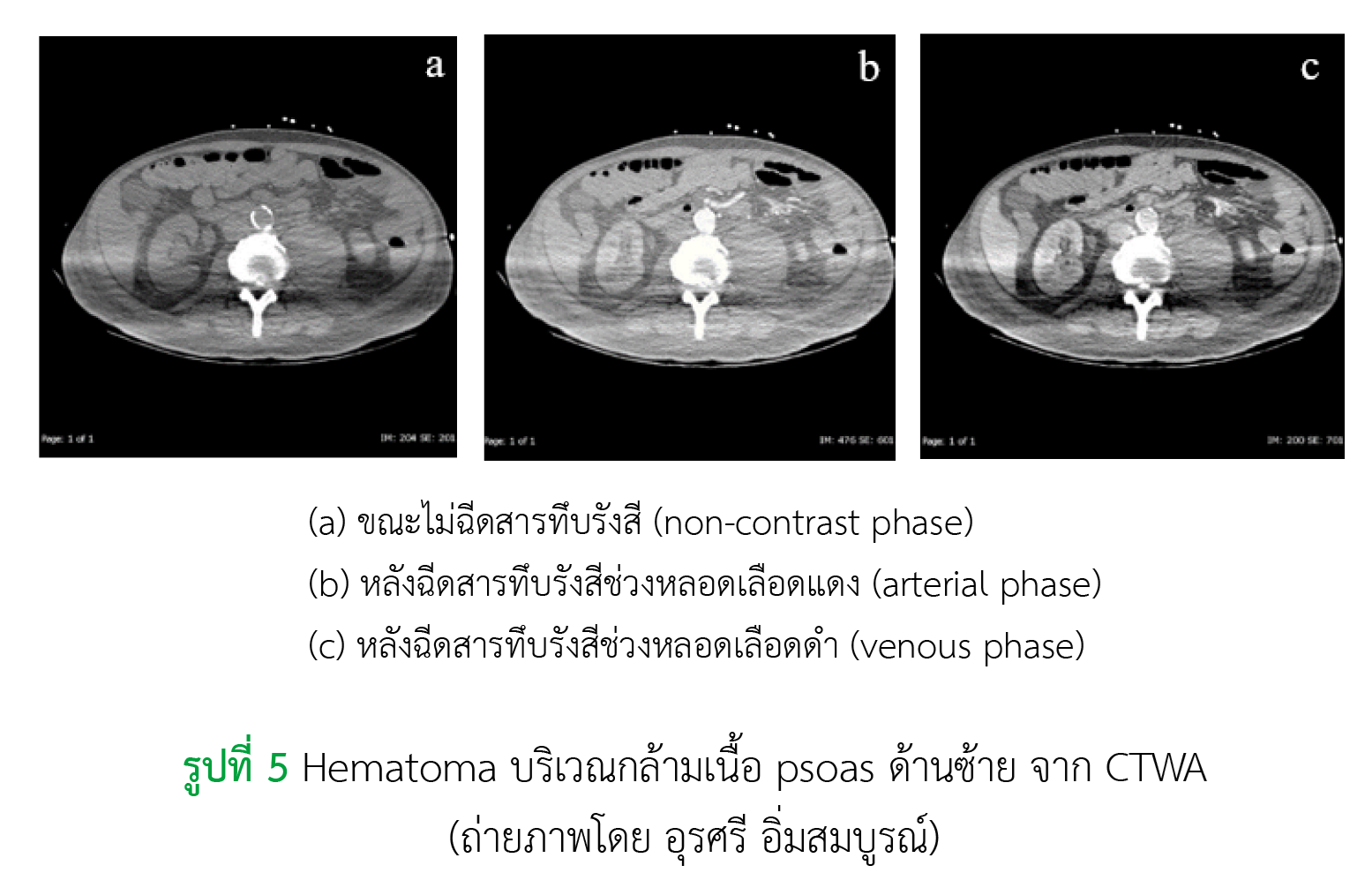
ภาวะลิ่มเลือดอุดหลอดเลือดดำและโรคลิ่มเลือดอุดกั้นในปอด เป็นภาวะที่พบบ่อยในผู้ป่วยที่มีการติดเชื้อ ไวรัสโคโรนา 2019 หรือโควิด-19 เนื่องจากผู้ป่วยกลุ่มนี้มักมีภาวะการแข็งตัวของเลือดที่ผิดปกติ แนวทางการรักษาจึงแนะนำการให้ยาต้านการแข็งตัวของเลือดเพื่อป้องกันและรักษาภาวะลิ่มเลือดอุดตัน โดยมักใช้ยาต้านการแข็งตัวของเลือดชนิดฉีดเข้าใต้ชั้นผิวหนังที่สามารถออกฤทธิ์ได้อย่างรวดเร็ว จากกรณีผู้ป่วย 2 รายที่ได้รับยาเฮพารินชนิดที่มีน้ำหนักโมเลกุลต่ำ คือ อีน็อคซาพาริน ในขนาดยา 40 มิลลิกรัม วันละ 1 ครั้ง ซึ่งเป็นขนาดยาเพื่อป้องกันการเกิดลิ่มเลือดอุดตัน เกิดภาวะเลือดออกบริเวณที่ฉีดและกล้ามเนื้อ psoas ซึ่งอยู่ใกล้เคียงบริเวณที่ฉีด โดยความเสี่ยงที่ทำให้ผู้ป่วยเกิดภาวะเลือดออกคือการได้รับยาในขนาดสูงและเทคนิคการฉีดที่ไม่เหมาะสม ทั้งนี้การป้องกันและลดความเสี่ยงในการเกิดภาวะเลือดออกสามารถทำได้โดยการปรับขนาดยาตามค่าการทำงานของไต และติดตามค่า anti-Xa หลังจากการได้รับยาครั้งที่ 3 ในผู้ป่วยที่ได้รับยาวันละ 1 ครั้ง หรือหลังจากการได้รับยาครั้งที่ 3 หรือ 4 ในผู้ป่วยที่ได้รับยาวันละ 2 ครั้ง รวมถึงการฉีดยาด้วยเทคนิคที่ถูกต้อง คือ การฉีดยานานอย่างน้อย 30 วินาทีจนยาหมดหลอดยาโดยดึงผิวหนังตลอดเวลาขณะเดินยาและทิ้งเข็มค้างไว้ประมาณ 10 วินาที จะสามารถลดความเสี่ยงในการเกิดภาวะเลือดออกในผู้ป่วยได้
เอกสารอ้างอิง
Sharma S, Mishra A, Ashraf Z. COVID-19 induced coagulopathy (CIC): thrombotic manifestations of viral infection. TH Open. 2022;6(1):e70-9. doi: 10.1055/s-0042-1744185.
Nopp S, Moik F, Jilma B, Pabinger I, Ay C. Risk of venous thromboembolism in patients with COVID-19: a systematic review and meta-analysis. Res Pract Thromb Haemost. 2020;4(7):1178–91. doi: 10.1002/rth2.12439.
Geerts WH. Prevention of venous thromboembolism in high-risk patients. Hematology Am Soc Hematol Educ Program. 2006;2006(1):462–6. doi: 10.1182/asheducation-2006.1.462.
Sakr Y, Giovini M, Leone M, Pizzilli G, Kortgen A, Bauer M, et al. Pulmonary embolism in patients with coronavirus disease-2019 (COVID-19) pneumonia: a narrative review. Ann Intensive Care. 2020;10:124. doi: 10.1186/s13613-020-00741-0.
Cuker A, Tseng EK, Nieuwlaat R, Angchaisuksiri P, Blair C, Dane K, et al. American society of hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19. Blood Adv. 2021;5(3):872–88. doi: 10.1182/bloodadvances.2020003763.
Ohn MH, Ng JR, Ohn KM, Luen NP. Double-edged sword effect of anticoagulant in COVID-19 infection. BMJ Case Rep. 2021;14(3):e241955. doi: 10.1136/bcr-2021-241955.
Musoke N, Lo KB, Albano J, Peterson E, Bhargav R, Gul F, et al. Anticoagulation and bleeding risk in patients with COVID-19. Thromb Res. 2020;196:227–30. doi: 10.1016/j.thromres.2020.08.035.
Cosmi B, Giannella M, Fornaro G, Cristini F, Patacca A, Castagna A, et al. Intermediate dose enoxaparin in hospitalized patients with moderate-severe COVID-19: a pilot phase II single-arm study, INHIXACOVID19. BMC Infect Dis. 2023;23(1):718. doi: 10.1186/s12879-023-08297-7.
Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825-30. doi: 10.7326/0003-4819-158-11-201306040-00007.
Sikes L, Charles K, Antigua A, Patel R, Imboywa S, Cherian P. Anti-factor Xa level monitoring for enoxaparin prophylaxis and treatment in high-risk patient groups. HCA Healthc J Med [Internet]. 2023;4(2):105-9. doi: 10.36518/2689-0216.1464.
Zufferey PJ, Dupont A, Lanoiselée J, Bauters A, Poissy J, Goutay J, et al. Pharmacokinetics of enoxaparin in COVID-19 critically ill patients. Thromb Res. 2021;205:120–7. doi: 10.1016/j.thromres.2021.07.010.
Spyropoulos AC, Goldin M, Giannis D, Diab W, Wang J, Khanijo S, et al. Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with COVID-19: the HEP-COVID randomized clinical trial. JAMA Intern Med. 2021;181(12):1612-20. doi: 10.1001/jamainternmed.2021.6203.
Montalescot G, Collet JP, Tanguy ML, Ankri A, Payot L, Dumaine R, et al. Anti-Xa activity relates to survival and efficacy in unselected acute coronary syndrome patients treated with enoxaparin. Circulation. 2004;110(4):392–8. doi: 10.1161/01.CIR.0000136830.65073.C7.
Stutsrim AE, Eady JM, Collum M, Rebo GJ, Rebo KA, Miller PR, et al. Weight-based enoxaparin achieves adequate anti-Xa levels more often in trauma patients: a prospective study. Am Surg. 2021;87(1):77–82. doi: 10.1177/0003134820949519.
COVID-19 Treatment Guidelines Panel. Antithrombotic therapy in patients with COVID-19. In: Coronavirus disease 2019 (COVID-19) treatment guidelines [Internet]. Bethesda, Maryland: National Institutes of Health. 2023 [cited 2023 Nov 25]. Available from: https://www.covid19treatmentguidelines.nih.gov/therapies/antithrombotic-therapy/
คณะแพทยศาสตร์โรงพยาบาลรามาธิบดี ศูนย์บริการพยาธิวิทยา. คู่มือการใช้บริการทางพยาธิวิทยา ฉบับ 2563-2565 [อินเทอร์เน็ต]. กรุงเทพมหานคร: ศูนย์บริการข้อมูลโรงพยาบาลรามาธิบดี คณะแพทยศาสตร์โรงพยาบาลรามาธิบดี มหาวิทยาลัยมหิดล. 2565 [สืบค้นเมื่อ 5 ม.ค. 2566]. สืบค้นจาก: https://www.ramapatholab.com/homepage/labtest/70
คณะแพทยศาสตร์ศิริราชพยาบาล ภาควิชาพยาธิวิทยาคลินิก. คู่มือการส่งตรวจทางห้องปฏิบัติการ ภาควิชาพยาธิวิทยาคลินิก: Anti-Xa assay [อินเทอร์เน็ต]. กรุงเทพมหานคร: คณะแพทยศาสตร์ศิริราชพยาบาล มหาวิทยาลัยมหิดล. 2565 [สืบค้นเมื่อ 5 ม.ค. 2566]. สืบค้นจาก: https://www.si.mahidol.ac.th/th/manual/Project/pdf/anti-xa.pdf
Thomas O, Lybeck E, Strandberg K, Tynngård N, Schött U. Monitoring low molecular weight heparins at therapeutic levels: dose-responses of, and correlations and differences between aPTT, anti-factor Xa and thrombin generation assays. PLoS One. 2015;10(1):e0116835. doi: 10.1371/journal.pone.0116835.
Schmid P, Fischer AG, Wuillemin WA. Low-molecular-weight heparin in patients with renal insufficiency. Swiss Med Wkly. 2009;139(31–32):438–52. doi: 10.4414/smw.2009.11284.
สุพัตรา อุปนิสากร, จารุวรรณ บุญรัตน์. การฉีดยากลุ่มเฮพารินที่มีน้ำหนักโมเลกุลต่ำเข้าชั้นใต้ผิวหนัง : ประสบการณ์ทางการพยาบาล. วารสารมหาวิทยาลัยนราธิวาสราชนครินทร์ [อินเทอร์เน็ต]. 2556 [สืบค้นเมื่อ 25 พ.ย. 2566];5(3):142-50. สืบค้นจาก: https://li01.tci-thaijo.org/index.php/pnujr/article/view/53780
ณยฎา ธนกิจธรรมกุล. การพยาบาลเพื่อลดการเกิดรอยช้ำในผู้ป่วยที่ได้รับยาอีนอกซาพารินโซเดียม. วารสารสมาคมพยาบาลแห่งประเทศไทยฯ สาขาภาคเหนือ [อินเทอร์เน็ต]. 2564 [สืบค้นเมื่อ 25 พ.ย. 2566];27(1):38-49. สืบค้นจาก: https://he01.tci-thaijo.org/index.php/jnorthnurse/article/view/247399
Jueakaew S, Piancharoensin R, Pinkesorn N, Thippayarom S, Sermsathanasawadi N. Novel subcutaneous low-molecular-weight heparin injection technique to reduce post-injection bruising. Phlebology. 2019;34(6):399–405. doi: 10.1177/0268355518813512.
Chung KT. Intra-abdominal hematoma following enoxaparin injection. Clin Med Insights Case Rep. 2016;9:35–8. doi: 10.4137/CCRep.S17881.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2023 สมาคมเภสัชกรรมโรงพยาบาล(ประเทศไทย)

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมโรงพยาบาลทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของสมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสาร (สมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย)) อย่างเป็นลายลักษณ์อักษร
สมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับสมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) และบุคลากรในสมาคมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ


.png)

