Care Service for Patients with Herpes Genitalis at Siriraj Hospital
Main Article Content
Abstract
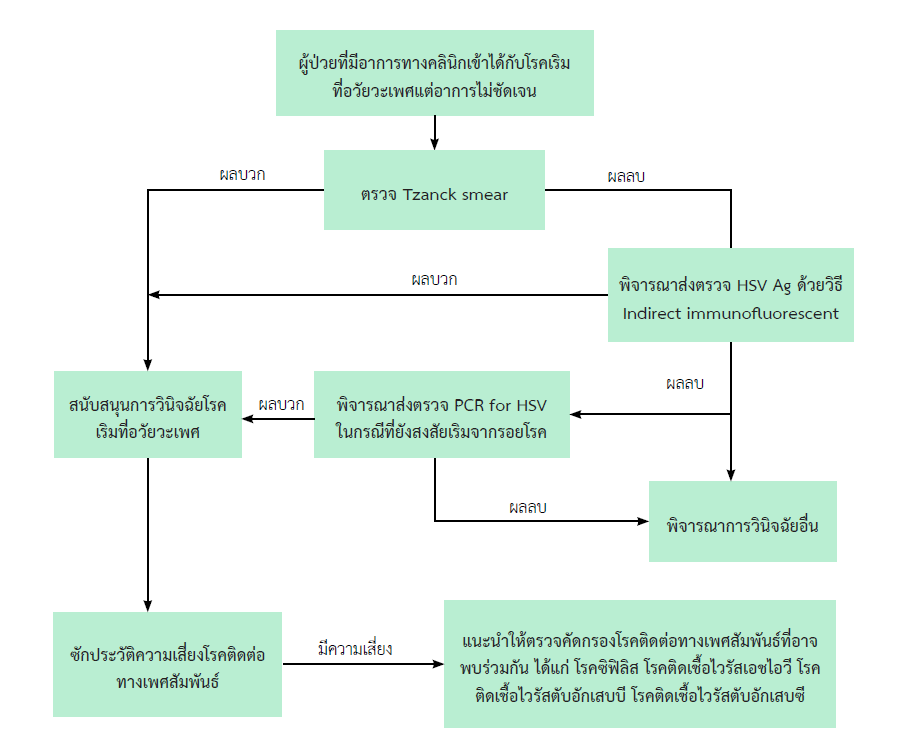
Genital herpes is a sexually transmitted infection (STI) caused by two types of Herpes simplex virus (HSV); HSV-1 and HSV-2. HSV-2 causes higher disease severity and more frequent recurrence. It typically presents as a group of vesicles in which transmission occurs. The vesicles then rupture and transform into ulcers with concomitant secondary bacterial infections. As asymptomatic shedding is very common, its prevalence and the probability of horizontal transmission are high. Differential diagnoses include syphilis, chancroid, or other non-STI genital ulcers. Patients presenting with pathognomonic lesions can be clinically diagnosed and can be confirmed using Tzanck smear, the most commonly used bedside diagnostic tool. Serologic tests, like HSV immunoglobulin G and immunoglobulin M, may be used to guide to the tailor-made management. Patients presenting with atypical lesions can be tested using HSV antigen and nucleic acid amplification tests (NAAT). Patients are prescribed with either oral acyclovir, valacyclovir, or famciclovir, which are considered the mainstay treatment. Patients with primary infection and recurrent episodes require different treatment regimens. In pregnant patients and patients with immunocompromised conditions, adjusted doses are given based on specific guidelines. Furthermore, the consideration in treating pregnant women with genital herpes should be based on the stage of disease and the gestational age at acquiring HSV. Vertical transmission can occur during pregnancy, mainly during the intrapartum period. The primary infection with HSV in the third trimester is the most critical period. All patients should also be evaluated for other STIs, such as human immunodeficiency virus infection, syphilis, hepatitis B infection, and hepatitis C infection.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187.
Leeyaphan C, Surawan TM, Chirachanakul P, Prasertworonun N, Punyaratabandhu P, Omcharoen V, et al. Clinical characteristics of hypertrophic herpes simplex genitalis and treatment outcomes of imiquimod: a retrospective observational study. International Journal of Infectious Diseases. 2015;33:165-70.
Chaiyabutr C JN, Apinuntham C, Leeyaphan C, Jiamton S. . Comparison of the Sensitivity and Specificity of Tzanck Smear and Immunofluorescence Assay for the Diagnosis of Cutaneous Herpes Simplex Virus and Varicella Zoster Virus Infections in a Real-life Clinical Setting Siriraj Med J. 2021;73(5):305-11.
Singh A, Preiksaitis J, Ferenczy A, Romanowski B. The laboratory diagnosis of herpes simplex virus infections. Can J Infect Dis Med Microbiol. 2005;16(2):92-8.
LeGoff J, Péré H, Bélec L. Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virol J. 2014;11:83-.
Glass N, Nelson HD, Huffman LH, editors. Screening for Genital Herpes Simplex : Brief Update for the U . S . Preventive Services Task Force2005.
M Hansgeorg, K Heinz. Neoplasias and Hyperplasia of Muscular and Neural Origin. Fitzpatrick’s Dermatology 9th ed. New York: McGraw-Hill Education.2019.
Chaweekulrat P, Leeyaphan C. Hypertrophic Herpes Simplex Infections: successful adjuvant treatment with topical imiquimod. Thai J Dermatol 2020;36(1):1-6.
Leeyaphan C, Nanchaipruek Y, Phinyo P. Therapeutic outcomes and prognostic factors in patients with hypertrophic herpes simplex infection treated with imiquimod: A systematic review and meta-analysis of individual patient data from case reports and case series. J Dermatol. 2022;49(9):879-86.
Samies N, James SH. Prevention and treatment of neonatal Herpes simplex virus. Antiviral Res.2020;176:104721
Amecian College of Obstetricians and Gynecologists. ACOG Practice Bulletin No.220: Management of genital herpes in pregnancy. Obstetrics&Gynecology. 2020;135:e193-e202
Foley E, Clarke E, Beckett VA, Harrison S, Pillai A, FitzGerald M, Owen P, Low-Beer N, Patel R. Green-top guideline No. 30: Management of genital herpes in pregnancy. https://www.rcog.org.uk/guidance/browse-all-guidance/other-guidelines-and-reports/management-of-genital-herpes-in-pregnancy/ (Accessed 6 September 2022)