Gender-Affirming Hormone Therapy and Antiretroviral Drugs of Human Immune Deficiency Virus
Main Article Content
Abstract
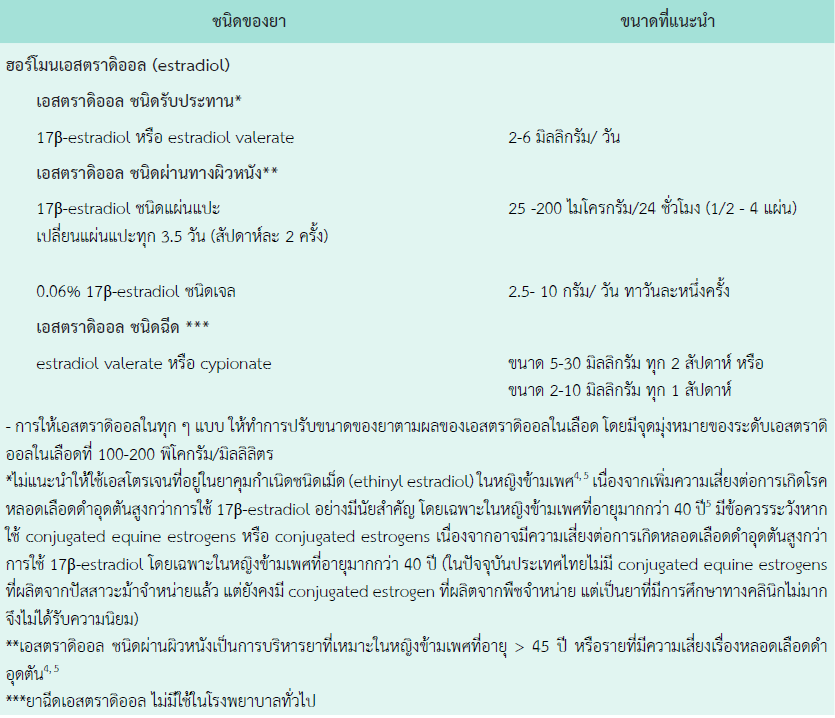
Transgender healthcare consists of three main components, including social transition, gender-affirming hormone treatment, and gender-affirming surgery. Not all transgender individuals need all available treatment options, they have different ways to select the appropriate and suitable therapeutic options. Gender-affirming hormone therapy should be prescribed individually based on benefits versus potential short- and long-term individual risks. There is a major difference in hormone therapy between transgender women and transgender men. In adult transgender women, estrogen and antiandrogen are used to replace female hormone and suppress endogenous male hormone, respectively. On the other hand, estrogen-only therapy should be used in transgender women who had undergone orchiectomy-based gender affirming surgery. In transgender men, testosterone-only therapy can be prescribed for transgender individuals who had or had not undergone gender affirming surgery. Testosterone therapy simultaneously suppresses endogenous female hormone and replaces exogenous male hormone with a single agent. Antiretroviral therapy for Human Immune Deficiency Virus (HIV) prevention, including pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) are very interesting options due to its efficacy. Combinations of transgender hormone therapy and HIV prophylaxis in transgender individuals are common in clinical practice. The drug interaction of the concurrent use of gender-affirming hormone therapy and some antiretroviral drugs for HIV should be taken into account. Some types of antiretroviral drugs affect circulating sex hormone levels. However, some serum antiretroviral drug levels are affected by sex hormone treatment. In clinical practice, the concurrent use of both groups of drugs could be considered. The appropriate strategies are to select the right agents, monitor serum sex hormones, and the appropriate adjustment dose of gender-affirming hormone therapy.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). 5th ed. American Psychiatric Publishing; Arlington: 2013.
World Health Organization. International Statistical Classification of Diseases and related health problems: Alphabetical index. Vol. 3. World Health Organization, 2004.
International Classification of Diseases 11th Revision: World Health Organization. [cited 2023 May 6]; Available from: https://icd.who.int/en
Coleman E, Radix AE, Bouman WP, Brown GR, de Vries ALC, Deutsch MB, et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int J Transgend Health. 2022;23(Suppl 1):S1-S259.
Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102(11):3869-903.
Poteat T, Reisner SL, Radix A. HIV epidemics among transgender women. Curr Opin HIV AIDS. 2014;9(2):168-73.
Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the Prevalence of HIV and Sexual Behaviors Among the US Transgender Population: A Systematic Review and Meta-Analysis, 2006-2017. Am J Public Health. 2019;109(1):e1-e8.
Guadamuz TE, Wimonsate W, Varangrat A, Phanuphak P, Jommaroeng R, McNicholl JM, et al. HIV prevalence, risk behavior, hormone use and surgical history among transgender persons in Thailand. AIDS Behav. 2011;15(3):650-8.
Allan-Blitz LT, Konda KA, Calvo GM, Vargas SK, Leon SR, Segura ER, et al. High incidence of extra-genital gonorrheal and chlamydial infections among high-risk men who have sex with men and transgender women in Peru. Int J STD AIDS. 2018;29(6):568-76.
Hiransuthikul A, Janamnuaysook R, Sungsing T, Jantarapakde J, Trachunthong D, Mills S, et al. High burden of chlamydia and gonorrhoea in pharyngeal, rectal and urethral sites among Thai transgender women: implications for anatomical site selection for the screening of STI. Sex Transm Infect. 2019;95(7):534-9.
UCSF Gender Affirming Health Program, Department of Family and Community Medicine, University of California San Francisco. Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People; 2nd edition. Deutsch MB, ed. June 2016. Available at transcare.ucsf.edu/guidelines.
Dahlhamer JM, Galinsky AM, Joestl SS, Ward BW. Barriers to Health Care Among Adults Identifying as Sexual Minorities: A US National Study. Am J Public Health. 2016;106(6):1116-22.
Thammapiwan P, Suwan A, Panyakhamlerd K, Suwajo P, Phanuphak N, Taechakraichana N. The sexual function among transgender women who have undergone gender-affirming surgery using penile skin inversion vaginoplasty in Thailand. Eur J Plast Surg. 2022;45:101-7.
Elfering L, van der Sluis WB, Mermans JF, Buncamper ME. Herpes neolabialis: herpes simplex virus type 1 infection of the neolabia in a transgender woman. Int J STD AIDS. 2017;28(8):841-3.
Uaamnuichai S, Panyakhamlerd K, Suwan A, Suwajo P, Phanuphak N, Ariyasriwatana C, et al. Neovaginal and anal high-risk human papillomavirus DNA among Thai transgender women in Gender Health Clinics. Sex Transm Dis. 2021;48:547-9.
Bodsworth NJ, Price R, Davies SC. Gonococcal infection of the neovagina in a male-to-female transsexual. Sex Transm Dis. 1994;21(4):211-2.
Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al; iPrEx Study Team. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587-99.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al; Partners PrEP Study Team. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399-410.
Pathela P, Braunstein SL, Blank S, Shepard C, Schillinger JA. The high risk of an HIV diagnosis following a diagnosis of syphilis: a population-level analysis of New York City men. Clin Infect Dis. 2015 ;61(2):281-7.
Ruxrungtham K, Chokephaibulkit K, Chetchotisakd P, Chariyalertsak S, Kiertburanakul S, Putacharoen O, et al. Thailand National Guidelines on HIV/AIDS Treatment and Prevention 2021/2022. Nonthaburi: Division of AIDS and STIs, Department of Disease Control; 2022.
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services [Internet]. [cited 2023 Jan 27]. Available from: https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf
Medical Eligibility Criteria for Contraceptive Use. 5th ed. Geneva: World Health Organization; 2015. PMID: 26447268.
Yager JL, Anderson PL. Pharmacology and drug interactions with HIV PrEP in transgender persons receiving gender affirming hormone therapy. Expert Opin Drug Metab Toxicol. 2020;16(6):463-74.
Grant RM, Pellegrini M, Defechereux PA, Anderson PL, Yu M, Glidden DV, et al. Sex Hormone Therapy and Tenofovir Diphosphate Concentration in Dried Blood Spots: Primary Results of the Interactions Between Antiretrovirals And Transgender Hormones Study. Clin Infect Dis. 2021;73(7):e2117-e2123.
Hiransuthikul A, Janamnuaysook R, Himmad K, Kerr SJ, Thammajaruk N, Pankam T, et al; iFACT Study Team. Drug-drug interactions between feminizing hormone therapy and pre-exposure prophylaxis among transgender women: the iFACT study. J Int AIDS Soc. 2019;22(7):e25338.