Nursing Care for Patients with Symptomatic Severe Aortic Stenosis After Undergoing Transcatheter Aortic Valve Replacement (TAVR)
Main Article Content
Abstract
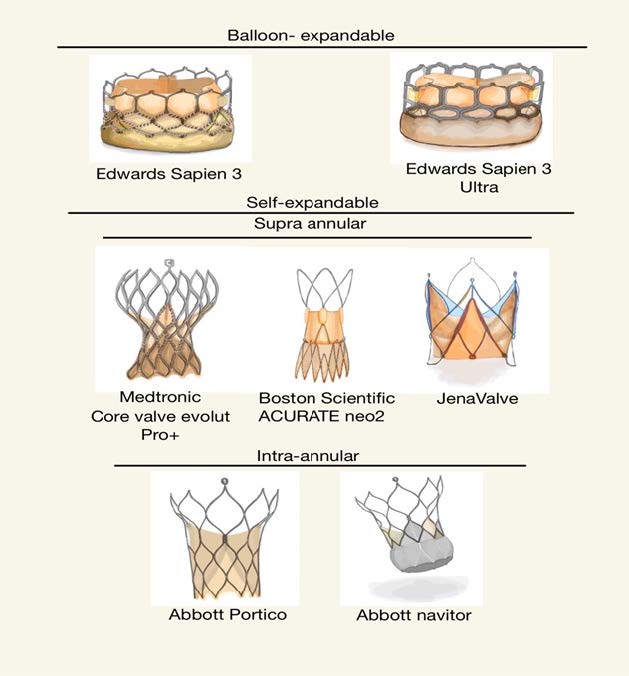
Aortic stenosis (AS) is a common defect of the heart valve, especially among the elderly. If severe AS is left untreated and accompanied by heart failure symptoms, the risk of mortality increases. Early intervention is crucial for improving treatment outcomes and enhancing patients' quality of life. Transcatheter aortic valve replacement (TAVR), a minimally invasive procedure, has advanced significantly over the past decade as a novel technology to treating symptomatic severe aortic stenosis in high-risk elderly patients or those who are not suitable candidates for surgical aortic valve replacement (SAVR). TAVR has gained popularity worldwide, including in Thailand, and has become the primary treatment option replacing the conventional surgical aortic valve replacement. TAVR is considered a minimally invasive alternative with comparable effectiveness and safety to surgical aortic valve replacement. It also reduces the risk of complications associated with surgical aortic valve replacement, allows more rapid patient recovery and reduces the length of hospital stay. However, like any medical procedure, there may be potential complications, such as damage to blood vessels, cerebral artery embolism, acute kidney injury from contrast agents, myocardial ischemia, and cardiac conduction abnormalities. Particularly within the first 24 hours post TAVR procedure, nurses play a crucial role in caring for patients to achieve treatment goals and ensure safety from potential complications. Therefore, nurses must possess knowledge and nursing skills for assessment and close monitoring of changing conditions. They should be able to make timely decisions regarding nursing interventions. Additionally, they should also support patients in their physical recovery as quickly as possible to ensure that patient care meets the highest standards of quality and safety. Understanding TAVR approaches, post-procedural monitoring, and potential complications will enable nurses to provide better care for patients undergoing TAVR and ensure the best possible outcomes.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Aluru JS, Barsouk A, Saginala K, Rawla P, Barsouk A. Valvular Heart Disease Epidemiology. Med Sci 2022;10:32.
Strange G, Stewart S, Celermajer D, Prior D, Scalia GM, Marwick T, et al. Poor Long-Term Survival in Patients With Moderate Aortic Stenosis. J Am Coll Cardiol 2019;74:1851-63.
Karycki MK. Transcatheter aortic valve replacement. Nursing 2019;49:24-31.
Estes BA, Kalra A. Contemporary nursing care in transcatheter aortic valve replacement. J Vasc Nurs 2018;36:186-88.
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease. J Am Coll Cardiol 2021;77:e25-e197.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2022;43:561-632.
Lee CH, Inohara T, Hayashida K, Park D-W. Transcatheter Aortic Valve Replacement in Asia. J Am Coll Cardiol 2021;1:279-93.
Tugaoen Z, Nguyen P, Arora S, Vavalle J. The selection of transcatheter heart valves in transcatheter aortic valve replacement. Trends Cardiovasc Med 2022;32:513-22.
Beurtheret S, Karam N, Resseguier N, Houel R, Modine T, Folliguet T, et al. Femoral Versus Nonfemoral Peripheral Access for Transcatheter Aortic Valve Replacement. J Am Coll Cardiol 2019;74:2728-39.
Paone G, Eng M, Kabbani LS, Borgi J, Peterson E, Novitsky B, et al. Transcatheter Aortic Valve Replacement: Comparing Transfemoral, Transcarotid, and Transcaval Access. Ann Thorac Surg 2018;106:1105-12.
Caring for Patients after Transcatheter Aortic Valve Replacement [Internet]. American Nurses Association 2017 [cited 22 febuary 2023]. Available from: https://www.myamericannurse.com/caring-patients-transcatheter-aortic-valve-replacement/.
Rouleau SG, Brady WJ, Koyfman A, Long B. Transcatheter aortic valve replacement complications: A narrative review for emergency clinicians. Am J Emerg Med 2022;56:77-86.
Bhushan S, Huang X, Li Y, He S, Mao L, Hong W, et al. Paravalvular Leak After Transcatheter Aortic Valve Implantation Its Incidence, Diagnosis, Clinical Implications, Prevention, Management, and Future Perspectives: A Review Article. Curr Probl Cardiol 2022;47:100957.
Rivera FB, Al-Abcha A, Ansay MFM, Magalong JVU, Tang VAS, Ona HM, et al. Transcatheter Aortic Valve Replacement (TAVR)-associated Acute Kidney Injury: An Update. Cardiorenal Med 2023.
Messika-Zeitoun D, Urena M. 16 - Transcatheter Aortic Valve Implantation: Role of Echocardiography in Patient Selection, Procedural Planning and Monitoring, and Evaluation of Outcomes. In: Otto CM, editor. Practice of Clinical Echocardiography (Fifth Edition). Philadelphia: Elsevier; 2017. p. 287-302.
Cantey C. Transcatheter Aortic Valve Replacement: Clinical Update for Nurse Practitioners. J Nurse Pract 2021;17:926-31.
Smolka G, Wojakowski W. Paravalvular leak-important complication after implantation of prosthetic valve. E-journal of Cardiology Practice 2010;9.
ชนนิกานต์ บุญเรือง, ต้นตนัย นำเบญจพล, กานดิษฎ์ ประยงค์รัตน์, หัสยา ประสิทธิ์ดำรง. ภาวะโลหิตจางจากเม็ดเลือดแดงแตกอย่างรุนแรงภายหลังการผ่าตัดเปลี่ยนลิ้นหัวใจเทียมเอออร์ติก. J Hematol Transfus Med 2016;26:43-47.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2021;42:3599-726.
Patel Manesh R, Calhoon John H, Dehmer Gregory J, Grantham James A, Maddox Thomas M, Maron David J, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2016 Appropriate Use Criteria for Coronary Revascularization in Patients With Acute Coronary Syndromes. J Am Coll Cardiol 2017;69:570-91.
Wood David A, Lauck Sandra B, Cairns John A, Humphries Karin H, Cook R, Welsh R, et al. The Vancouver 3M (Multidisciplinary, Multimodality, But Minimalist) Clinical Pathway Facilitates Safe Next-Day Discharge Home at Low-, Medium-, and High-Volume Transfemoral Transcatheter Aortic Valve Replacement Centers. JACC Cardiovasc Interv 2019;12:459-69.
Brouwer J, Nijenhuis VJ, Delewi R, Hermanides RS, Holvoet W, Dubois CLF, et al. Aspirin with or without Clopidogrel after Transcatheter Aortic-Valve Implantation. N Engl J Med 2020;383:1447-57.
Lauck SB, Wood DA, Baumbusch J, Kwon J-Y, Stub D, Achtem L, et al. Vancouver Transcatheter Aortic Valve Replacement Clinical Pathway. Circ Cardiovasc Interv 2016;9:312-21.