Swallowing Problems in Children
Main Article Content
Abstract
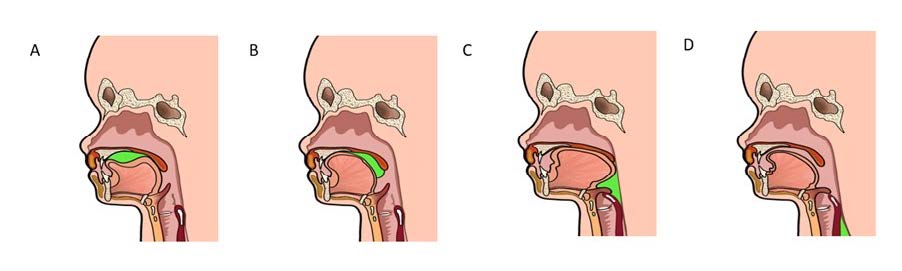
Abnormal swallowing in children is common in pediatric practice, especially in the children with neurological or developmental disorder. The symptoms include frequent choking or coughing during swallowing. In addition, there may be dyspnea caused by airway obstruction, aspiration, and recurrent pneumonia. The healthcare providers who care for children with suspected swallowing problems need to understand the child’s age-related eating development and normal swallowing processes. A thorough history taking, including symptoms, age-appropriate diet, and feeding posture, is essential. A child suspected of having a swallowing problem requires a thorough physical examination, especially the oral cavity, and observing symptoms while eating. Additional investigations such as videofluoroscopic swallowing study (VFSS) or fiberoptic endoscopic evaluation of swallowing (FEES) may be performed where the cause of swallowing problems cannot be determined through history and physical examination. Besides treating the cause of swallowing problems in children, adjusting the texture of diet and eating posture is a necessary additional treatment to reduce complications that may arise if aspiration occurs again.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Gosa MM, Dodrill P, Lefton-Greif MA, Silverman A. A Multidisciplinary Approach to Pediatric Feeding Disorders: Roles of the Speech-Language Pathologist and Behavioral Psychologist. Am J Speech Lang Pathol. 2020;29(2S):956-66.
Arvedson JC, Brodsky L. Pediatric swallowing and feeding: Assessment and management 3rd ed ed: Plural Publishing; 2017.
Garcia JM, Chambers Et, Noll KS. Gravity flow test comparisons for mildly thick consistency. J Texture Stud. 2020;51(2):308-13.
Bhattacharyya N. The prevalence of pediatric voice and swallowing problems in the United States. Laryngoscope. 2015;125(3):746-50.
Arvedson JC. Assessment of pediatric dysphagia and feeding disorders: clinical and instrumental approaches. Dev Disabil Res Rev. 2008;14(2):118-27.
Lefton-Greif MA. Pediatric dysphagia. Phys Med Rehabil Clin N Am. 2008;19(4):837-51, ix.
Benfer KA, Weir KA, Bell KL, Ware RS, Davies PSW, Boyd RN. Oropharyngeal Dysphagia and Cerebral Palsy. Pediatrics. 2017;140(6).
Speyer R, Cordier R, Kim JH, Cocks N, Michou E, Wilkes-Gillan S. Prevalence of drooling, swallowing, and feeding problems in cerebral palsy across the lifespan: a systematic review and meta-analyses. Dev Med Child Neurol. 2019;61(11):1249-58.
Benfer KA, Weir KA, Bell KL, Ware RS, Davies PS, Boyd RN. Oropharyngeal dysphagia in preschool children with cerebral palsy: oral phase impairments. Res Dev Disabil. 2014;35(12):3469-81.
Motion S, Northstone K, Emond A, Team TAS. Persistent early feeding difficulties and subsequent growth and developmental outcomes. Ambul Child Health. 2001;7(3-4):231-7.
Jadcherla S. Dysphagia in the high-risk infant: potential factors and mechanisms. Am J Clin Nutr. 2016;103(2):622S-8S.
Kakodkar K, Schroeder JW, Jr. Pediatric dysphagia. Pediatr Clin North Am. 2013;60(4):969-77.
Durvasula VS, O'Neill AC, Richter GT. Oropharyngeal Dysphagia in children: mechanism, source, and management. Otolaryngol Clin North Am. 2014;47(5):691-720.
Prasse JE, Kikano GE. An overview of pediatric dysphagia. Clin Pediatr (Phila). 2009;48(3):247-51.
Velayutham P, Irace AL, Kawai K, Dodrill P, Perez J, Londahl M, et al. Silent aspiration: Who is at risk? Laryngoscope. 2018;128(8):1952-7.
Jones B. Abnormalities of pharyngeal function. 4th ed ed. Gore RM, Levine MS, editors. Philadelphia: Elsevier Saunders; 2015.
Dodrill P, Gosa MM. Pediatric Dysphagia: Physiology, Assessment, and Management. Ann Nutr Metab. 2015;66 Suppl 5:24-31.
Hiss SG, Postma GN. Fiberoptic endoscopic evaluation of swallowing. Laryngoscope. 2003;113(8):1386-93.
Giraldo-Cadavid LF, Leal-Leano LR, Leon-Basantes GA, Bastidas AR, Garcia R, Ovalle S, et al. Accuracy of endoscopic and videofluoroscopic evaluations of swallowing for oropharyngeal dysphagia. Laryngoscope. 2017;127(9):2002-10.
Cichero JA, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, et al. Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: The IDDSI Framework. Dysphagia. 2017;32(2):293-314.
Wu XS, Miles A, Braakhuis A. The Effectiveness of International Dysphagia Diet Standardization Initiative-Tailored Interventions on Staff Knowledge and Texture-Modified Diet Compliance in Aged Care Facilities: A Pre-Post Study. Curr Dev Nutr. 2022;6(4):nzac032.
Shimizu A, Momosaki R, Kayashita J, Fujishima I. Impact of Multiple Texture-Modified Diets on Oral Intake and Nutritional Status in Older Patients with Pneumonia: A Retrospective Cohort Study. Dysphagia. 2020;35(4):574-82.
Lawlor CM, Choi S. Diagnosis and Management of Pediatric Dysphagia: A Review. JAMA Otolaryngol Head Neck Surg. 2020;146(2):183-91.
Hwang YS, Lin CH, Coster WJ, Bigsby R, Vergara E. Effectiveness of cheek and jaw support to improve feeding performance of preterm infants. Am J Occup Ther. 2010;64(6):886-94.
Larnert G, Ekberg O. Positioning improves the oral and pharyngeal swallowing function in children with cerebral palsy. Acta Paediatr. 1995;84(6):689-92.
Vekerdy Z. Management of seating posture of children with cerebral palsy by using thoracic-lumbar-sacral orthosis with non-rigid SIDO frame. Disabil Rehabil. 2007;29(18):1434-41.
Kerzner B, Milano K, MacLean WC, Jr., Berall G, Stuart S, Chatoor I. A practical approach to classifying and managing feeding difficulties. Pediatrics. 2015;135(2):344-53.