Development and Evaluation Clinical Practice Guidelines for Prevention of Delirium Among Critically Ill Patients, Medicine Ward 3, Lampang Hospital
Keywords:
Clinical Practice Guidelines, Prevention ICU Delirium, Critically Ill PatientAbstract
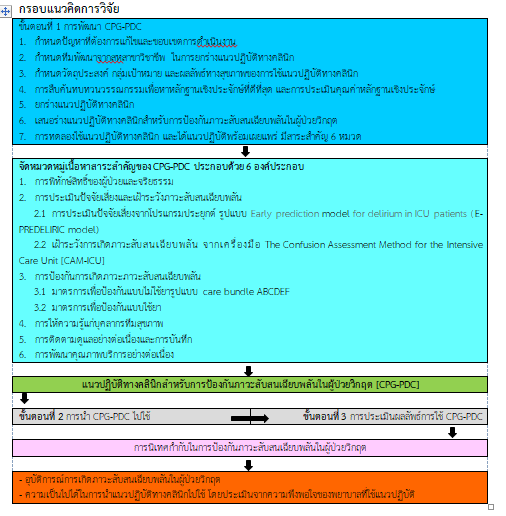
This developmental research aims to develop clinical practice guidelines (CPGs) for prevention delirium in critically ill patients, Lampang Hospital. The study was based on the CPGs implementing framework of the Australian National Health and Medical Research Council (NHMRC, 1999). The sample was selected as the patients who conscious and able to communicate patients, From the Richmond Agitation and Sedation Scale (RASS > -3 score). Subjects included 121 conscious patients, who were confined in Medicine Ward 3 before implementing of CPGs, and 106 subjects who were confined after implementing of CPGs. The instruments used in this study were CPGs for prevention of delirium among critically ill patients and a record form of the incidence of delirium in critically ill patients. Data analyses was done using descriptive statistics, percentage, mean, standard deviation and compare the data before and after using CPGs general data with independent t-test, exact probability test and incidence rate of delirium with multi variable risk difference regression statistics.
The CPGs consisted of six domains 1) patient protection and ethics 2) risk factor and prevention for ICU delirium by the application and The Confusion Assessment Method for the Intensive Care Unit [CAM-ICU] 3) Prevention by using non-pharmacology preventive measures in care bundle ABCDEF 4) Educating health team personnel 5) continuous monitoring and recording and 6) service quality improvement. The finding revealed that the incidence rate of ICU delirium among subjects in the CPGs group was 15 cases 14.2% and the average duration of the incidence (Mean) is 0.9 shift per case while the incidence rate of ICU delirium among subjects in the non-CPGs group was 42 cases only 34.7% and the average duration of the incidence (Mean) is 4.5 shift per case. By the incidence of P-value 0.071, resulting in less than 7-16.2% and the average duration of the incidence (Mean) value P-value < 0.001.
This study confirmed that implementing the CPGs was able to reduce the incidence rate of ICU delirium and the average duration of incidence (Mean). The investigator suggests these CPGs should be incorporated with quality improvement activities among another Ward.
References
Arend, E. & Christensen, M. (2009). Delirium in the intensive care unit: ฟ review. Nursing in Critical Care, 14(3), 145–154.
Bloom, B. S., Madaus, G. F., & Hastings, J. T. (1971). Handbook on formative and summative evaluation of student learning. New York: McGraw-Hill.
Boot, R. (2012). Delirium: a review of the nurse role in the intensive care unit. Intensive & Critical Care Nursing, 28(3), 185–189.
Bourne, R. S. (2008). Delirium and use of sedation agents in intensive care. Nursing in Critical Care, 13(4), 195-202.
Brummel, N. E., & Girard, T. D. (2013). Preventing delirium in the intensive care unit. Critical care Clinics, 29(1), 51-65.
Colombo, R., Corona, A., Praga, F., Minari, C., Giannotti, C., & Castelli, A., et al. (2012). A reorientation strategy for reducing delirium in the critically ill. Results of an interventional study. Minerva Anestesiologica, 78(9), 1026–1033.
Dennis, C. M., Lee, R., Woodard, E. K., Szalaj, J. J., & Walker, C. A. (2010). Benefits of quiet time for neuro-intensive care patients. The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses, 42(4), 217–224.
Desai, S., Chau, T., & George, L. (2013). Intensive care unit delirium. Critical Care Nursing Quarterly, 36(4), 370–389. Doungkaew, N. (2011). Effectiveness of implementing clinical practice guidelines for prevention of unplanned endotracheal extubations in medical intensive care unit, Lampang Hospital. Master of nursing science (Adult nursing) faculty of nursing, Chiang Mai University. (in Thai)
Environmental Protection Agency, Washington DC. (1974). Information on levels of environmental noise requisite to protect public health and welfare with an adequate margin of safety, Retrieved October 30, 2022 from https://www.nonoise.org/library/levels74/levels74.htm.
Fan, Y., Guo, Y., Li, Q., & Zhu, X. (2012). A review: nursing of intensive care unit delirium. The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses, 44(6), 307–316.
Hayhurst, C. J., Pandharipande, P. P., & Hughes, C. G. (2016). Intensive care unit delirium: a review of diagnosis, prevention, and treatment. Anesthesiology, 125(6), 1229–1241. doi: 10.1109/IEEESTD.2007.4299432.
Joanna Briggs Institute. (2013). JBI levels of evidence. Retrieved Jan 1, 2018 from https://jbi.global/sites/default/files/2019-05/JBI-Levels-of evidence_2014_0.pdf
King, J., & Gratrix, A. (2009). Delirium in intensive care. Continuing Education in Anaesthesia, Critical Care & Pain, 9(5), 144–147.
Konkani, A. & Oakley, B. (2012). Noise in hospital intensive care units - a critical review of a critical topic. Journal of Critical Care, 27(5), 522.e1-9.
Laohatanakom, S. (2014). Effectiveness of implementing clinical practice guidelines for prevention of delirium among critically ILL patients, medicial intensive care unit, Lampang hospital. Master of nursing science (Adult nursing) faculty of nursing, Chiang Mai University. (in Thai)
Laohatanakom, S. (2018). Clinical practice guidelines for the prevention of acute confusional states in Sub Intensive Care Unit. Lampang: Department of nursing, Lampang Hospital. (in Thai)
Linkaite, G., Riauka, M., Bunevičiute, I., & Vosylius, S. (2018). Evaluation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for the patients in the care unit. Acta Medica Lituanica, 25, 14-22.
Maldonado, J. R. (2008). Delirium in the acute care setting: Characteristics, diagnosis and treatment. Critical Care Clinics, 24(4), 657–722.
Maria, M. (2012). Delirium: a distressing and disturbing clinical event in a Intensive Care Unit. Health Science Journal, 6(4), 587-597.
Mistraletti, G., Pelosi, P., Mantovani, E. S., Berardino, M., & Gregoretti, C. (2012). Delirium: clinical approach and prevention, best practice & research. Clinical Anaesthesiology, 26(3), 311–326.
National Health and Medical Research Council. (1999). A guideline to the development, implementation and evaluation of clinical practice guideline. Canberra: Commonwealth Australia.
National Health and Medical Research Council. (2000). How to put the evidence into practice: Implementation and dissemination strategies. Canberra: Commonwealth Australia.
Pun, B. T., & Boehm, L. (2011). Delirium in the intensive care unit: Assessment and AACN Advanced Critical Care, 22(3), 225–237. https://doi.org/10.1097/NCI.0b013e318220c173
Rand, D., Lehman, B., & Shteynberg, A. (2007, June). Issues, models and solutions for triac modulated phase dimming of LED lamps. In 2007 IEEE Power Electronics Specialists Conference (pp. 1398-1404). IEEE.
Schiemann, A., Hadzidiakos, D., & Spies, C. (2011). Managing ICU delirium. Current Opinion in Critical Care, 17(2), 131–140.
Statistics of internal medicine wards registration III. (2017). Lampang: internal medicine wards. Lampang Hospital. (in Thai)
Tabet, N., & Howard, R. (2006). Prevention, diagnosis and treatment of delirium: Staff educational approaches. Expert Review of Neurotherapeutics, 6(5), 741–751.
Thongchai, C. (2005). Clinical practice guidelines development. The Thai Journal of Nursing Council, 20(2), 63-76.
Van Rompaey, B., Elseviers, M. M., Schuurmans, M. J., Shortridge-Baggett, L. M., Truijen, S., & Bossaert, L. (2009). Risk factors for delirium in intensive care patients: A prospective cohort study. Critical Care (London, England), 13(3), R77.
Van, R. B., Schuurmans, M. J., Shortridge-Baggett, L. M., Truijen, S., & Bossaert, L. (2008). Risk factors for intensive care delirium: A systematic review. Intensive & Critical Care Nursing, 24(2), 98–107.
Zomorodi, M., Topley, D., & McAnaw, M. (2012). Developing a mobility protocol for early mobilization of patients in a surgical/trauma ICU. Critical Care Research and Practice, 2012, 964547. doi: 10.1155/2012/964547
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Boromarajonani College of Nursing, Nakhon Si Thammarat

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของ วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช และบุคคลากรท่านอื่น ๆ ในวิทยาลัยฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว