Effectiveness of the Nutritional Support Program on Malnutrition Level and Performance Status among Peritoneal Dialysis Patients with Malnutrition in a Dialysis Clinic, Maesot Hospital, Tak Province
Keywords:
Nutritional Support Program, Malnutrition, Performance Status, Peritoneal Dialysis Patients, Dialysis ClinicAbstract
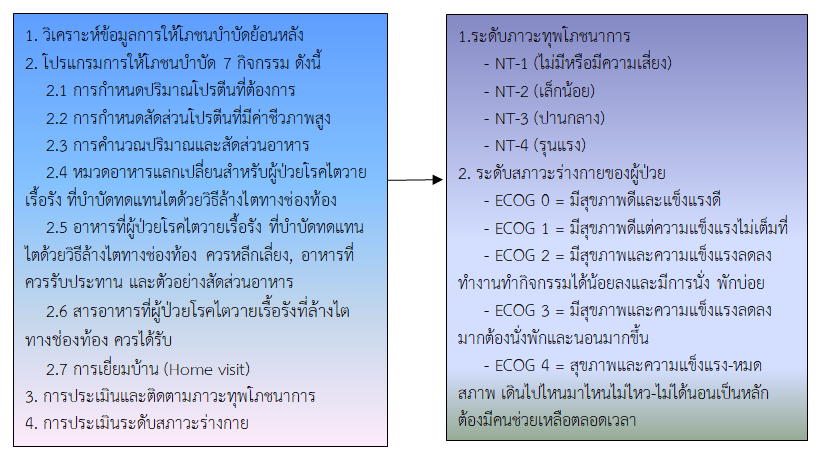
This one-group pretest-posttest quasi-experimental research aimed to examine the effectiveness of the nutritional support program on the level of malnutrition and performance status among peritoneal dialysis patients with malnutrition in a dialysis clinic, Maesot Hospital, Tak Province, from May to September 2020. 45 participants were selected by the purposive sampling technique. The instrument used in the experiment was a nutritional therapy program with seven activities. The collection data tools were the nutritional status screening form, the malnutrition assessment form, and the physical condition assessment form. The data were analyzed by descriptive statistics and a Wilcoxon signed rank test.
The results showed that 57.8% of the participants were female, with an average age of 54 years. After receiving the nutritional therapy program, peritoneal dialysis patients with malnutrition had statistically significant decreased levels of malnutrition and had a better level of physical condition than before receiving the nutrition therapy program (p-value< 0.001).
Therefore, medical professionals, multidisciplinary teams, dietitians, and nutritionists should implement this nutrition therapy program in community hospitals and sub-district health promotion hospitals, as well as promote self-care abilities in caregivers and health volunteers, to reduce the referral rate of peritoneal dialysis patients with severe malnutrition to network hospitals.
References
Brown, R. O. & Compher, C. (2010). A.S.P.E.N. Clinical guidelines: nutrition support in adult acute and chronic renal failure. Journal of Parenteral Enteral Nutrition, 34(4), 366-377. https://www.doi.org/10.1177/0148607110374577.
Bulun, A. & Suwalee L., (2022). Food consumption behavior and factors affecting food consumption Behavior of chronic kidney disease patients at chronic disease clinic, Chiang Yuen hospital, Mahasarakham province. KKU Journal for Public Health Research, 15(2), 28-38.
Cano, N., Fiaccadori, E., Tesinsky, P., Toigo, G., Druml, W., Kuhlmann, M., et al. (2006). ESPEN guidelines on enteral nutrition: adult renal failure. Clinical Nutrition, 25(2), 295-310. https://www.doi:10.1016/j.clnu.2006.01.023.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. (2nd). New jersey: Lawrence Erlbaum Associates, Publishers.
Department of Nutritional. (2019). Evaluation of malnutrition in chronic renal failure patients. Faculty of Public Health: Nakhon Pathom. (in Thai)
Gemma, S. C., Lluis, S. M., & Lourdes, R., (2005). What and how much do we eat? 24-hour dietary recall method. Nutricion Hospitalaria, 31(Supl.3), 46-48. https://www.doi:10.3305/nh.2015.31.sup3.8750.
Health Technology and Policy Assessment Program. (2017). Revised nutritional screening and evaluation tool, easy to use, does not increase workload [online]. [cited 2020 April 10]; Available from https://www.hitap.net/168140
Intha, S., Tangkawanich, T., & Yokubol, D., (2013). Effects of supportive and educative nursing program on self care. Quality of life and target clinical indicators for progression of severity of chronic kidney disease patients in a community. Journal of Nursing Science Chulalongkorn University, 25(2), 95-107.
Jivakanon, S. & Kittisakulnam, P. (2013). Malnutrition in peritoneal dialysis patients: principles and evaluation. In the patronage of patronage, Textbook of guidelines for peritoneal dialysis, textbook practical peritoneal dialysis. Faculty of Medicine. Bangkok: Chulalongkorn University, (in Thai)
Jiwakanon, S., Warodomwichit, D., Supasyndh, O., Chattranukulchai, P., Pisprasert, V., Nongnuch, A., et al. (2018). Clinical practice recommendation for nutritional management in adult kidney patients 2018. Thai JPEN, 28(2), 18-67.
Kaematorn, K., Panpae, K., (2019) Factors influencing quality of life in pre-dialysis chronic kidney disease patients In CKD clinic Damnoensaduak hospital. Hua Hin Sook Jai Klai Kangwon Journal, 3(2), 28-37.
Kalsamrit, K. (2017). Nutrition for the chronic kidney disease. In Pachotakarn, K., Techangam, S. Editor, nutrition for people with kidney disease Chronic. Bangkok: Wakkawittaya. Department of Internal Medicine Faculty of Medicine Siriraj Hospital, Mahidol University and Rajavithi Hospital, Department of Medical Services. (in Thai)
Klabcharoen, S. (2002). The relationship between attitude towards food practice family support withDietary behaviors of chronic renal failure patients receiving Hemodialysis treatment with hemodialysis. Thesis master’s degree nutrition sciences, faculty of science. Bangkok: Mahidol University.
Lacey, K., & Pritchett, E. (2003). Nutrition care process and model: ADA adopts road map to quality care and outcomes management. Journal of the Academy of Nutrition and Dietetics, 103(8), 1061-1072.
Medical Informatics Division (2020). From the statistical data, the top 5 diseases in Thai patients who died Mae Sot Hospital, Tak Province, the past 5 years 2015 - 2019. Tak: Mae Sot Hospital. (in Thai)
Nanna, P. (2011). Effects of a supportive-educative nursing program on knowledge, self-care agency in patients with chronic kidney disease treated with hemodialysis. Journal of faculty of nursing Burapha University, 19(3), 10-22.
Oken, M., Creech, R., Tormey, D., Horton, J., Davis, T. E., McFadden, E. T., et al. (1982). Toxicity and response criteria of the Eastern Cooperative Oncology Group. American Journal Clinical Oncology, 5(6), 649-655.
Pairojkittrakul, S., Harnirattisai, T., & Thitiarchakul, S. (2014). The effect of a shared care-promoting program on shared care, nutritional status and, exit site infection among continuous ambulatory peritoneal dialysis patients. Ramathibodi Nursing Journal, 20(3), 325-340.
Rebollo, P., Alvarez-Ude, F., Valdés, C., & Estébanez, C. (2004). Different evaluations of the health related quality of life in dialysis patients. Journal of Nephrology, 17(6), 833-840.
Rongmuang, D., & Sukrungreung, I. (2021). Nursing care to promote health and quality of life among the elderly undergoing continuous ambulatory peritoneal dialysis. Journal of health science research, 15(2),162-172.
Salamon, K. M., & Lambert, K. (2018). Oral nutritional supplementation in patients undergoing peritoneal dialysis: a randomised, crossover pilot study. Journal of Renal Care, 44(2), 73–81. https://www.doi.org/10.1111/jorc.12224
Suwanphet, N. (2010). Stress health conditions Outstanding with high-level library. Thesis Master of Nursing Yod, Faculty of Nursing, Khon Kaen University. (in Thai)
Taweebut, P., Kerdmongko, P., & Amnatsatsue, K. (2017). The effect of a supportive - educative nursing program for chronic disease patients with early stage kidney disease. Journal of Public Health Nursing, 31(1), 129-145.
The Nephrology Society of Thailand. (2015). Recommendations for the prior care of patients with chronic kidney disease Kidney Replacement Therapy 2015. Bangkok. (in Thai)
The Nephrology Society of Thailand. (2018). Clinical Practice Recommendation for Nutritional Management in Adult Kidney Patients 2018 [online]. [cited 2021 April 10]; Available from: https://www.nephrothai.org/wp-content/uploads/2021/10/ Guidelines for nutrition therapy for adults with nephrotic syndrome-2018.pdf. (in Thai)
The Nephrology Society of Thailand. (2021). Thailand renal replacement therapy year 2016-2019 [online]. [cited 2021 April 10]; Available from https://www.nephrothai.org/wp-content/uploads/2021/01/1.TRT-Annual-report-2016-2019.pdf. (in Thai)
Trakulhoon, V., & Prammanasudh, B. (2020). From BNT 2000 to NT 2013 the malnutrition dentification in Adult Patients” Royal Thai Air Force Medical Gazette, 66(2), 14-32.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Boromarajonani College of Nursing, Nakhon Si Thammarat

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของ วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช และบุคคลากรท่านอื่น ๆ ในวิทยาลัยฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว