แนวทางการจัดการตนเองของผู้ที่เสี่ยงต่อการเป็นโรคเบาหวานตำบลบ้านลำนาว จังหวัดนครศรีธรรมราช
คำสำคัญ:
แนวทางการจัดการตนเอง, ปัจจัยเสี่ยง, ผู้ที่เสี่ยงต่อการเป็นโรคเบาหวานบทคัดย่อ
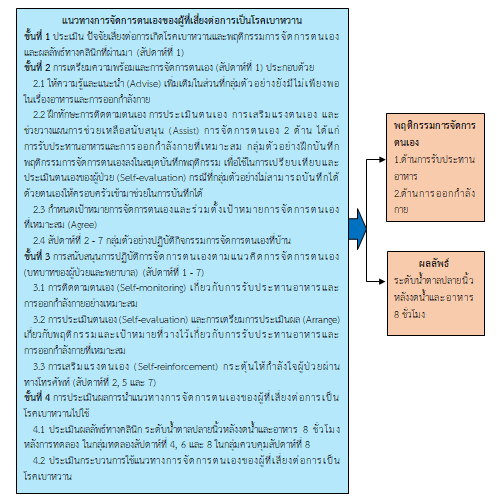
การวิจัยกึ่งทดลองนี้มีวัตถุประสงค์เพื่อศึกษาผลของการใช้แนวทางการจัดการตนเองในการลดปัจจัยเสี่ยงต่อการเป็นโรคเบาหวาน ประชากรที่ใช้ในการศึกษา คือ ผู้ที่เสี่ยงต่อการเป็นโรคเบาหวาน คำนวณขนาดกลุ่มตัวอย่าง โดยโปรแกรม Power analysis จำนวน 60 คน สุ่มกลุ่มตัวอย่างอย่างง่าย สุ่มเลือกตัวอย่างเข้าเป็นกลุ่มทดลองและกลุ่มควบคุมโดยวิธีจับฉลาก กลุ่มละ 30 คน เก็บข้อมูลระหว่างเดือนมีนาคม – พฤษภาคม พ.ศ. 2566 กลุ่มทดลองได้รับแนวทางการจัดการตนเองของผู้ที่เสี่ยงต่อการเป็นโรคเบาหวาน ประกอบด้วย 4 ขั้นตอน ได้แก่ 1) การประเมินปัจจัยเสี่ยงต่อการเกิดโรคเบาหวานและความรู้การรับประทานอาหารและ
การออกกำลังกาย 2) การให้ความรู้เกี่ยวกับโรคเบาหวาน การจัดการตนเองเพื่อลดปัจจัยสี่ยงต่อการเป็นโรคเบาหวาน และการฝึกทักษะการจัดการตนเองเพื่อลดปัจจัยสี่ยงต่อการเป็นโรคเบาหวาน 3) การสนับสนุนการจัดการตนเอง และ 4) การประเมินผลการปรับเปลี่ยนพฤติกรรม กลุ่มควบคุมได้รับบริการสุขภาพตามระบบเดิม กลุ่มทดลองได้รับการประเมินระดับน้ำตาลปลายนิ้วหลังงดน้ำและอาหาร 8 ชั่วโมง ในระยะก่อนทดลองและหลังทดลองสัปดาห์ที่ 4, 6 และ 8 วิเคราะห์ข้อมูลโดยแจกแจงความถี่ ร้อยละ ค่าเฉลี่ย ส่วนเบี่ยงเบนมาตรฐาน ทดสอบความแตกต่างของระดับน้ำตาลในเลือดระหว่างกลุ่มทดลองและกลุ่มควบคุมด้วยสถิติ independent t-test และทดสอบความแตกต่างของระดับน้ำตาลในเลือดในระยะก่อนทดลองและหลังทดลองสัปดาห์ที่ 4, 6 และ 8 โดยใช้ Repeated Measure ANOVA
ผลการวิจัย พบว่า หลังการทดลองสัปดาห์ที่ 8 กลุ่มทดลองมีค่าเฉลี่ยระดับน้ำตาลปลายนิ้วหลังงดน้ำและอาหาร 8 ชั่วโมง ต่ำกว่ากลุ่มควบคุมอย่างมีนัยสำคัญทางสถิติ (p < 0.01) และค่าเฉลี่ยระดับน้ำตาลในเลือดของกลุ่มทดลองในสัปดาห์ที่ 8 ต่ำกว่าสัปดาห์ที่ 6 สัปดาห์ที่ 4 และก่อนทดลองอย่างมีนัยสำคัญทางสถิติ (p < 0.01)
จากงานวิจัย แสดงให้เห็นถึงประสิทธิผลของแนวทางการจัดการตนเองของผู้ที่เสี่ยงต่อการเป็นโรคเบาหวานพยาบาลระดับปฐมภูมิสามารถนำไปใช้เป็นแนวทางปฏิบัติสำหรับผู้ที่เสี่ยงต่อการเป็นโรคเบาหวาน
เอกสารอ้างอิง
Aekplakorn, W., Bunnag, P., Woodward, M., Sritara, P., Cheepudomwit, S., Yamwong, S., et al. (2006). A risk score for predicting incident diabetes in the Thai population. Diabetes Care, 29, 1872-1877.
Akeplakorn, W., Puckcharern, H., & Satheannoppakao, W. (2021). Diabetes. In Akeplakorn, W. (Editor), The 6th Survey of Thai Public Health by Physical Examination, 2019-2020. Bangkok: Aksorn Grphic and Design Publishing Limited Partnership. (in Thai)
American Diabetes Association. (2017). Classification and diagnosis of diabetes. Diabetes Care, 40(1), S11-24.
American Diabetes Association. (2018). Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care. 41(1), S13-S27.
Balk, E. M., Earley, A., Raman, G., Avendano, E. A., Pittas, A. G., & Remington, P. L. (2015). Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force. Annals of Internal Medicine, 163(6), 437-451.
Bloom, B. S. (1971). Handbook on formative and summative evaluation of student learning. New York : McGraw-Hill.
Boontein, P., Poungkaew, A., Praphasil, O., & Kuakool, P. (2021). Factors predicting self- management behavior in patients with type II diabetes. Nursing Science Thailand, 39(1), 13-23.
Chulaporn, S. & Sattanako, C. (2017). Effects of self management program on glycemic control in patients with type 2 diabetes. Journal of Nursing and Education, 10(4), 32-46.
Cohen, J. (1998). Statistical power analysis for the behavioral sciences (2nd ed). New Jersey: Lawrence Erlbaum Associates, Incorporated.
Glasgow, R. E., Emont, S., & Miller, D. C. (2006). Assessing delivery of five ‘As’ for patient- centered counseling. Health Promotion International, 21(3), 245-255.
Grady, P. A. & Gough, L. L. (2014). Self-management: a comprehensive approach to management of chronic conditions. American Journal of Public Health, 104(1), 25-31.
Jangwang, S., Pittayapinune, T., & Chutipattana, N. (2016). Factors related to self-care behavior for prevention of diabetes mellitus and hypertension among population groups at risk. The Southern College Network Journal of Nursing and Public Health, 3(1), 110-128.
Kanfer, F. H. & Gaelick-Bays, L. (1991). Self management medthod. In Kanfer, F. H., Goldsteinn, A. (Eds.), Helping people change: a text book at medthods. (305-360). New York: Pergamon press.
Milenkovi, T., Gavrilovic, S., Percan, V., & Petrovski, G. (2004). Influence of diabetic education on patient well-being and metabolic control. Diabetologia Croatica, 33(3), 91-96.
Ministry of Public Health. (2017). eHealth strategy, Ministry of Public Health (2017 – 2026). Retrieved May 24, 2023 from https://www.ict.moph.go.th/upload_file/files/eHealth_Strategy_ENG_141117.pdf.
Moucheraud, C., Lenz, C., Latkovic, M., & Wirtz, V. J. (2019). The costs of diabetes treatment in low-and middle-income countries: a systematic review. The British Medical Journal Global Health, 4(1), 1-12.
Munsrakeat, K., Rawiworrakul, T., & Lagampan, S. (2019). Effects of self-management program for glycemic control among insulin depen-dent type 2 diabetes patients. The Journal of Baromarajonani College of Nusing, Nakhonratchasima, 25(2), 87-103.
Nakhon Si Thammarat Provincial Health Office. (2022). The report system sends 43 files (HDC). Retrieved December 15, 2022 from https://nrt.hdc.moph.go.th/hdc/main/index_pk.php. (in Thai)
Polit, D. F. & Hungler, B. P. (1995). Nursing research: principles and medthods (5th ed.). New York: Lippincott company.
Saeedi, P., Petersohn, I., Salpea, P., Malanda, B., Karuranga, S., Unwin, N., et al. (2019). Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Research and Clinical Practice, 157, 107843. Retrieved December 15, 2022 from https://www.doi.org/10.1016/j.diabres.2019.107843
Sanee, A. (2014). Self-management program in chronic diseases. Journal of The Royal Thai Army Nurses, 15(2), 129-134.
Senaphan, S. & Sitthiban, S. (2018). Self-management guideline for reduction of diabetes risk factors in Ban Pakthon community, Chawang district, Nakhon Si Thammarat province. Region 11 Medical Journal, 32(1), 805-812.
Sontimuang, W. (2022). Factors related to self-care behavior of diabetic patients among the Urak Lawois, Koh Lanta district Krabi province. Maharaj Nakhon Si Thammarat Medical Journal, 5(2), 68-78.
Terathongkum, S., Kraithaworn, P., Poolsukkho, P., & Poolsawat, S. (2018). Effects of health behavior change program with arm swing exercise on body mass index and capillary blood sugar in pre-diabetes group. Thai Journal of Nursing and Midwifery Practice, 5(1), 19-31.
Wandao, Y., Chinnawong, T., Chalothorn, U., & Tipwong, A. (2018). The experience of self- management in patients with uncontrolled type 2 diabetes, Sadao hospital, Sadao, Songkhla. Songklanagarind Journal of Nursing, 38(3), 54-64.
WatcharapornNatkamyoung. (2023). The effects of developing a self-Management model in patients with uncontrolled type 2 diabetes, Banthi hospital, Lamphun province. Journal of Nursing and Public Health Research, 3(2), 78-95.
Wongpanarak, N. (2014). The therapeutic relationship: application in nursing process. Journal of The Royal Thai Army Nurses, 15(2), 84-91.
Wongsin, U. & Wannasri, A. (2018). Unit cost of diabetes care: a case study of a general hospital in Thailand. Journal of the Department of Medical Services, 43(6), 45-49.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2023 วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของ วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช และบุคคลากรท่านอื่น ๆ ในวิทยาลัยฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว