The Effects of Developing an Inpatient Medication Reconciliation System at Waeng Hospital
Keywords:
Medication Reconcilation, Medication DiscrepanciseAbstract
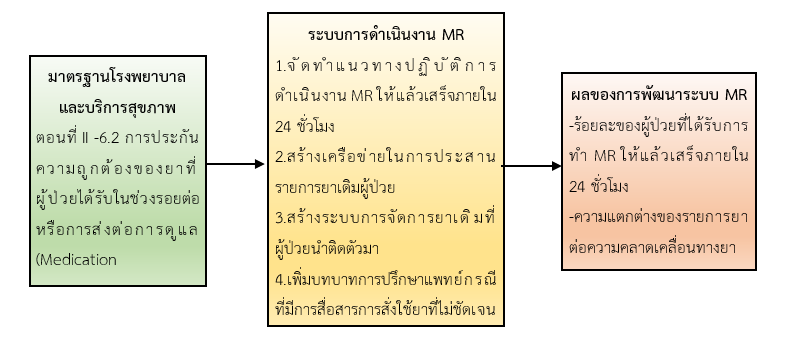
This research and development study aimed to examine the effects of developing an inpatient medication reconciliation (MR) system at Waeng Hospital. The research was conducted in three phases: Phase 1 studied the current situation and identified problems in the existing MR process; Phase 2 involved developing the inpatient MR system; and Phase 3 evaluated the effectiveness of the developed system. The sample consisted of all inpatients with chronic medication use admitted to Waeng Hospital. The research instruments included the medication reconciliation record form, doctor order sheets, and the HosXp program, with a content validity index of 1.00. Data were analyzed using frequency, percentage, and pre–post comparison with the Chi-square test.
The study found that the system ensured completion of the medication reconciliation (MR) process within 24 hours. Prior to the system development, 66.90% of inpatients had the MR process completed within 24 hours, whereas after the development, this increased to 99.66%. Following the system development, it became possible to analyze differences in medication lists related to medication errors for all patients. The findings revealed that 71.37% of the discrepancies were due to unintentional physician errors, which were classified as medication errors. In terms of severity, the errors were categorized at Level B, as the MR process guaranteed completion within 24 hours, thereby preventing the errors from reaching the patients. Before the system development, such analysis could not be performed.
The findings demonstrate that the medication reconciliation process can enhance medication safety when it is carried out comprehensively and within the specified timeframe. The process helps reduce the severity of adverse drug events, thereby improving patient safety in medication use.
References
Chiewchantanakit, D., Anupong, M., Pituchaturont, N., Dilokthornsakul, P.Dhippayom, T. (2020). The effectiveness of medication reconciliation to prevent medication errors: a systematic review and meta-analysis. ResSoc Admin Pharm, 16, 886-94.
Department of Disease Control. (2023). Annual report 2023, Division of Non-Communicable Diseases. Retrieved May 26, 2025 from https://www.ddc.moph.go.th/uploads/files/4155620240314033823.pdf. (in Thai)
ISMP Canada. Medication Reconciliation (MedRec). (2011). Institutes for safe medication practices 2011. Retrieved May 26, 2025 from https://www.ismp-canada.org/.
Jitanapakarn, P., Khunawaradisai, N., & Supapaan, T. (2023). Outcomes of medication reconciliation at patient ward in a community hospital in the Northeast. Thai Journal of Pharmacy Practice, 15(4), 1003-1014.
Joint Commission on Accreditation of Healthcare Organization. (2006). Sentinel event alert: using medication reconciliation to prevent errors. Retrieved May 26, 2025, from https://www.jointcommission.org//media/deprecatedunorganizedF.
Leeprapaiwong, R., Chantong, S., Wannarit, K., & Chitchaisong, S. (2017). Medication reconciliation in outpatients at the psychiatric clinic, Faculty of Medicine Siriraj Hospital. Siriraj Medical Bulletin, 7(2), 53–63. (in Thai)
Ministry of Public Health. (2022). Drug safety standards assessment program in hospitals and public health offices. Retrieved May 26, 2025. from https://dmsic.moph.go.th/editors/userfiles/files/hospital.pdf. (in Thai)
National Coordinating Council for Medication Error Report and Prevention (NCCMERP). (2008). What is amedication error?. Retrieved January 25, 2025. from https://nccmerp.org/about-medication-errors.
Ningsanon, T. (2008). Medication reconciliation. In Ningsanon, T., Montakantikul, P., & Chulavatnatol,S. Medication Reconciliation (pp.2–26). Prachachon. (in Thai)
Pattanakriangkrai, P., Thungwilai, W., & Pamonsinlapatham, P. (2022). Outcomes of the improvements of medication reconciliation process by multidisciplinary health team: case study at internal medicine ward 1, Sawanpracharak hospital, Nakhon Sawan province. Thai Journal of Pharmacy Practice, 14(4), 887-990. (in Thai)
Piriyachananusorn, N., Chalortham, N., & Kitikannakorn, N. (2023). Improvement and evaluation of medication reconciliation at orthopedic wards in a Regional hospital. Thai Journal of Pharmacy Practice, 15(3), 750-765. (in Thai)
Prince of Songkla University, (2020). Guideline for the Prevention and Management of Medication Errors, Announcement of the Faculty of Medicine. Retrieved January 25, 2025. from: https://medinfo.psu.ac.th/nurse/drug_paper/drug_12.pdf. (in Thai)
Puntakul, K., Topark-Ngarm, A. (2012). Medication reconciliation at Nakhon Ratchasima Rajanagarindra Psychiatric Hospital. Isan Journal of Pharmaceutical Sciences, 8(2), 28-38.
Ratanadetsakul, C. h. , Ratanadetsakul, P. (2018). Medication reconciliation through the 3P concept (Purpose-Process-Performance). Center for countinuing pharmacy education. Retrieved May 26, 2025. from https://ccpe.pharmacycouncil.org/index.php?option=article_detail &subpage=article_detail&id=469. (in Thai)
Saepang, K. (2010). Medication reconciliation and hospital standards and healthcare services. Thai Bulletin of Pharmaceutical Sciences, 5(1), 99–110. (in Thai)
Tewthanom, K., Tananonniwas, S. (2009). Medication error and prevention quide for patient’s safety. Veridian E-Jouenal, Silpakorn University, 2(1), 1-23. (in Thai)
The Healthcare Accreditation Institute (Public Organization). (2022). “Medication use practice.” In Hospital and Healthcare Standards. (pp.120-128), (5th ed.). Nonthaburi. (in Thai)
Thompson, C. A. (2005). JCAHO views medication reconciliation as adverse-event prevention. Am J Health Syst Pharm, 62(15), :1528-1532.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Boromarajonani College of Nursing, Nakhon Si Thammarat

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของ วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช และบุคคลากรท่านอื่น ๆ ในวิทยาลัยฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว