Alteplase - Induced Orolingual Angioedema: A Case Report
Keywords:
orolingual angioedema, alteplase, acute ischemic stroke, cerebrovascular disorderAbstract
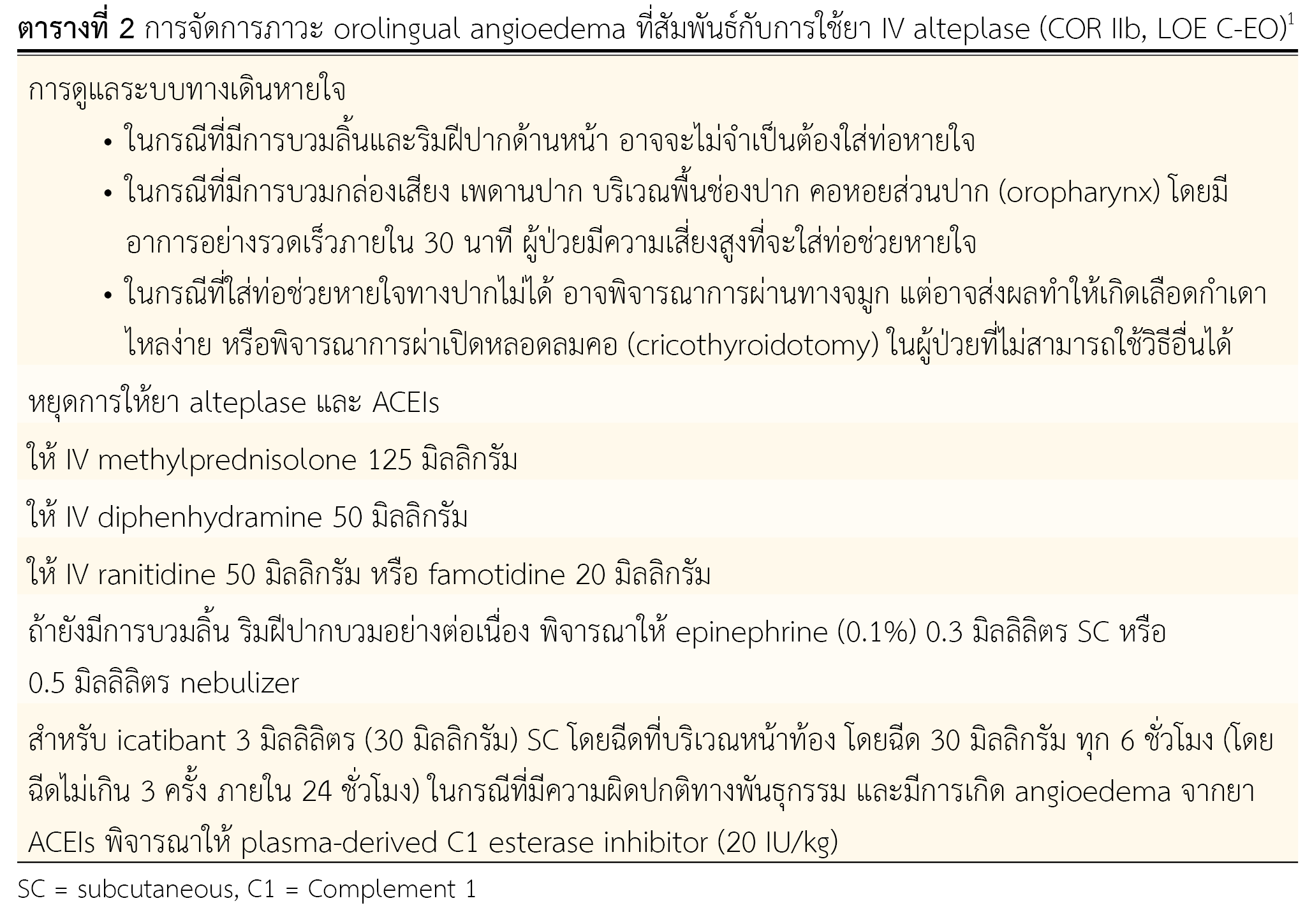
Alteplase is a fibrinolytic drug. It is the primary alternative medicine for treating acute ischemic stroke and effective in reducing disabilities. However, typical adverse effects were found. Intracerebral hemorrhage (6.4%) is mostly found and orolingual angioedema (1.5%) occurs but less frequent. This adverse effect, although low incidence, is essential because it might lead to sudden death.
A 55-year-old male was diagnosed of hypertension last year but had not yet received antihypertensive drugs. Three weeks ago, he had dysphagia and was admitted. At the hospital, he was diagnosed of esophageal cancer. After receiving enalapril, his left limbs were suddenly weak with facial palsy and slurred speech. On physical examination, neurological deficit was found, and on computerized tomography, a hypodensity lesion on the left lentiform nucleus was observed. Physician diagnosed patient as an acute ischemic stroke. Alteplase, an antifibrinoltic drug was given intravenously to patient in the total dose of 48.6 mg (0.9 mg/kg), divided into 4.86 mg in 1 minute and the remaining 43.74 mg intravenously infused 1 hour later. As soon as drug was completely infused, he began to experience stiffness and edema around the lower lip. Alteplase-related orolingual angioedema was suspected.
From this case study, the adverse effect was delayed until 11 hours later. Since every patient must wear a mask to prevent infection from COVID-19, the observation of adverse effect of orolingual angioedema is thus not detected and causes the delay. Fortunately, the patient's symptoms were not severe, and did not cause disability or death. It is therefore recommended to monitor patient who receives alteplase from the beginning and up to 2 hours after drug infusion for adverse effects that may occur and advise patient to self-observe these side effects.
References
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi: 10.1161/STR.0000000000000211.
Neurological Institute of Thailand. Clinical practice guidelines for ischemic stroke. 1st ed. Bangkok: Tanapress Publishers; 2019.
Haire WD. Pharmacology of fibrinolysis. Chest. 1992;101(4 Suppl):91S-7S.
Bivard A, Lin L, Parsonsb MW. Review of stroke thrombolytics. J Stroke. 2013;15(2):90-8.
National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333(24):1581-7.
Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-29.
Correia AS, Matias G, Calado S, Lourenco A, Viana-Baptista M. Orolingual angiodema associated with alteplase treatment of acute stroke: a reappraisal. J Stroke Cerebrovasc Dis. 2015;24(1):31-40.
Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan AM. Anaphylactoid reactions and angioedema during alteplase treatment of acute ischemic stroke. CMAJ. 2000;162(9):1281.
Shirazy M, Chaari A, Hakim K, Bousselmi K, Kauts V. A case of oropharyngeal angioedema following intravenous recombinant tissue plasminogen activator (rt-PA) and mechanical thrombectomy. Drug Saf Case Rep. 2019;6(1):10.
Lang DM, Aberer W, Bernstein JA, Chng HH, Grumach AS, Hide M, et al. International consensus on hereditary and acquired angioedema. Ann Allergy Asthma Immunol. 2012;109(6):395-402.
Wang YX, Li YQ, Chen Y, Zhang CH, Dong Z, Wang Z, et al. Analysis of related factors of orolingual angioedema after rt-PA intravenous thrombolytic therapy. Eur Rev Med Pharmacol Sci. 2018;22(5):1478-84.
Reed BR, Chen AB, Tanswell P, Prince WS, Wert RM, Jr., Glaesle-Schwarz L, et al. Low incidence of antibodies to recombinant human tissue-type plasminogen activator in treated patients. Thromb Haemost. 1990;64(2):276-80.
Tom B, Dendorfer A, de Vries R, Saxena PR, Jan Danser AH. Bradykinin potentiation by ACE inhibitors: a matter of metabolism. Br J Pharmacol. 2002;137(2):276-84.
Hill MD, Lye T, Moss H, Barber PA, Demchuk AM, Newcommon NJ, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60(9):1525-7.
Siragy HM, de Gasparo M, El-Kersh M, Carey RM. Angiotensin-converting enzyme inhibition potentiates angiotensin II type 1 receptor effects on renal bradykinin and cGMP. Hypertension. 2001;38(2):183-6.
Groger M, Lebesgue D, Pruneau D, Relton J, Kim SW, Nussberger J, et al. Release of bradykinin and expression of kinin B2 receptors in the brain: role for cell death and brain edema formation after focal cerebral ischemia in mice. J Cereb Blood Flow Metab. 2005;25(8):978-89.
Myslimi F, Caparros F, Dequatre-Ponchelle N, Moulin S, Gautier S, Girardie P, et al. Orolingual angioedema during or after thrombolysis for cerebral ischemia. Stroke. 2016;47(7):1825-30.
Narjes M, Sana K, Neveen F, Bashir I, Hani K, Hassen M, et al. Bradykinic mediated angioedema related to alteplase successfully treated by frozen fresh plasma (FFP) in Saudi Arabia: a first case report and literature review. J Neurol Neurosci. 2021;12:1-3.
Lewis LM, Graffeo C, Crosley P, Klausner HA, Clark CL, Frank A, et al. Ecallantide for the acute treatment of angiotensin-converting enzyme inhibitor-induced angioedema: a multicenter, randomized, controlled trial. Ann Emerg Med. 2015;65(2):204-13.
Pahs L, Droege C, Kneale H, Pancioli A. A novel approach to the treatment of orolingual angioedema after tissue plasminogen activator administration. Ann Emerg Med. 2016;68(3):345-8.
Cheong E, Dodd L, Smith W, Kleinig T. Icatibant as a potential treatment of life-threatening alteplase-induced angioedema. J Stroke Cerebrovasc Dis. 2018;27(2):e36-7. doi: 10.1016/j.jstrokecerebrovasdis.2017.09.039.
Riha HM, Summers BB, Rivera JV, Van Berkel MA. Novel therapies for angiotensin-converting enzyme inhibitor-induced angioedema: a systematic review of current evidence. J Emerg Med. 2017;53(5):662-79.
De Los Rios La Rosa F, Starosciak AK, Wolf B. Thrombolysis of a stroke patient with history of rtPA-associated angioedema. Neurol Clin Pract. 2017;7(6):541-3.
Sanchez-Borges M, Gonzalez-Aveledo LA. Angiotensin-converting enzyme inhibitors and angioedema. Allergy Asthma Immunol Res. 2010;2(3):195-8.
Brown T, Gonzalez J, Monteleone C. Angiotensin-converting enzyme inhibitor-induced angioedema: a review of the literature. J Clin Hypertens (Greenwich). 2017;19(12):1377-82.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Association of Hospital Pharmacy (Thailand)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมโรงพยาบาลทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของสมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสาร (สมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย)) อย่างเป็นลายลักษณ์อักษร
สมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับสมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) และบุคลากรในสมาคมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ


.png)

