Efficacy and Safety of New Direct Oral Anticoagulants for The Treatment of Venous Thromboembolism
Keywords:
direct oral anticoagulants, deep vein thrombosis, pulmonary embolism, venous thromboembolismAbstract
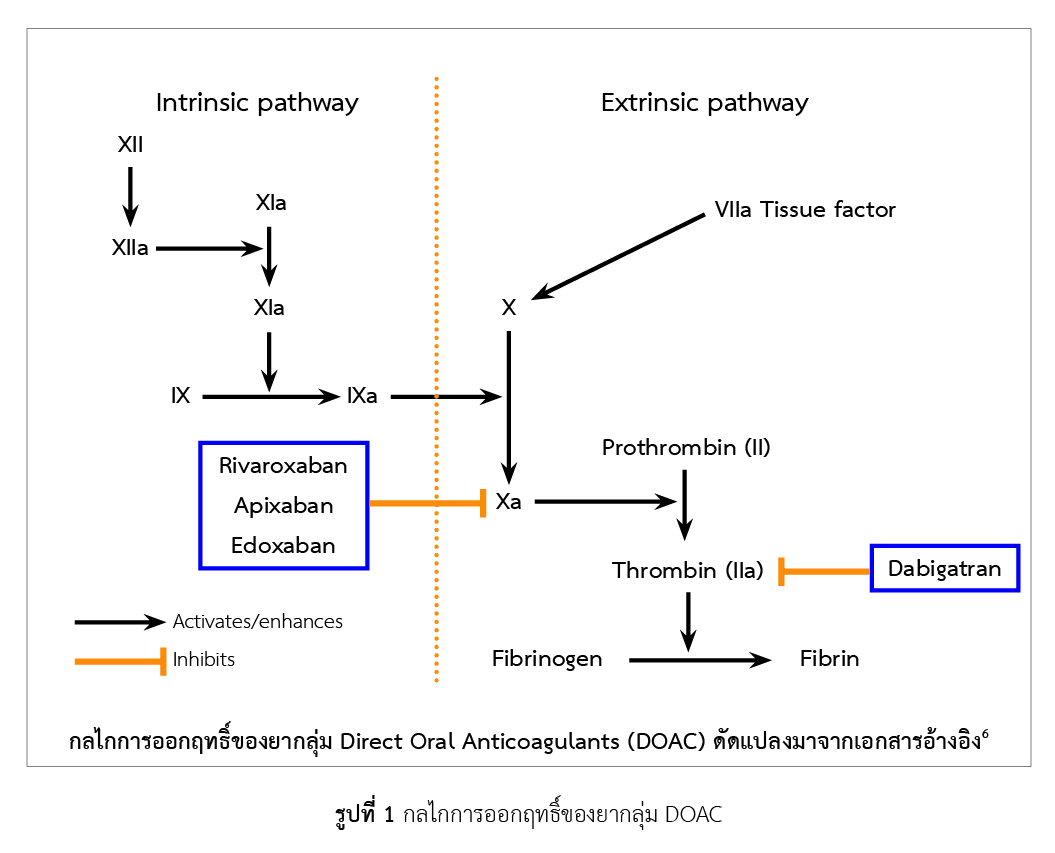
Direct oral anticoagulants (DOAC) are oral anticoagulants that act by directly inhibiting specific coagulation factors. This drug class was developed to overcome the limitation of warfarin that requires routine monitoring of international normalized ratio. One of the main indications of DOAC is for the treatment of venous thromboembolism (VTE) caused by abnormalities of blood coagulation, declined blood flow, or damaged blood vessel epithelial cells, and VTE can be divided into two types: deep vein thrombosis, and pulmonary embolism (PE). Time to maximum concentration of DOAC in blood ranges from 1 to 6 hours. The drug is metabolized in liver, and excreted in urine and feces. Adverse effects of DOAC such as major bleeding must be closely monitored. Renal function should also be evaluated as doses of DOAC must be adjusted in renal failure. Comparison of efficacy and safety of DOAC in the treatment of VTE suggested that DOAC can reduce VTE recurrence, major bleeding, and clinically relevant non-major bleeding, although these effects were not different from warfarin. On considering the effect of specific DOAC, it was found that apixaban and rivaroxaban can reduce the risk of major bleeding. DOAC that have been approved to be used in Thailand are apixaban, dabigatran, edoxaban, and rivaroxaban, which are all categorized as non-essential drugs in the national drugs lists. Thai practice guideline for VTE has recommended heparin and warfarin as the first line treatment, without inclusion of other DOAC.
References
Daniel MW, Nathan PC, Sara RV. Venous thromboembolism. In: Joseph TD, Robert LT, Gary CY, Gary RM, Barbara GW, Michael PL (eds). Pharmacotherapy: a pathophysiological approach. 10th ed. New York: McGraw-Hill Education, 2017. p. 231-60.
ยิ่งยง ชินธรรมมิตร์. การหาสาเหตุของภาวะลิ่มเลือดอุดตันหลอดเลือดในผู้ใหญ่. วารสารโลหิตวิทยาและเวชศาสตร์บริการโลหิต. 2560;27(4):433-7.
Wendelboe AM, Raskob GE. Global burden of thrombosis. Circ Res. 2016;118(9):1340-7.
Yeh CH, Hogg K, Weitz JI. Overview of the new oral anticoagulants: opportunities and challenges. Arterioscler Thromb Vasc Biol. 2015;35(5):1056-65.
Garmo C, Bajwa T, Burns B. Physiology, clotting mechanism. 2020. [cited 2020 July 11]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507795/.
Ann KW, Edith AN. Thrombosis. In: Koda-Kimble MA, Alldredge BK, editors. Applied therapeutics: the clinical use of drugs. 10th ed. Philadelphia: Lippincott Williams & Wilkins, 2013. p. 345-76.
Micromedex® (electronic version). Truven Health Analytics, Inc. Greenwood Village, Colorado, USA. [cited 2020 July 9]. Available from: https://www.micromedexsolutions.com.
Diane MFS, Jonathan MZ. Apixaban: Drug information. [cited 2020 June 30]. Available from: https://www.uptodate.com/contents/apixaban-drug-information?search=Apixaban&source=panel_search_result&selectedTitle=1~149&usage_type=panel&kp_tab=drug_general&display_rank=1.
Diane MFS, Jonathan MZ. Edoxaban: Drug information. [cited 2020 June 30]. Available from: https://www.uptodate.com/contents/edoxaban-drug-information?search=edoxaban%20drug%20information&source=panel_search_result&selectedTitle=1~102&usage_type=panel&kp_tab=drug_general&display_rank=1.
Diane MFS, Jonathan MZ. Rivaroxaban: Drug information. [cited 2020 June 30]. Available from: https://www.uptodate.com/contents/rivaroxaban-drug-information?search=rivaroxaban%20drug%20information&source=panel_search_result&selectedTitle=1~148&usage_type=panel&kp_tab=drug_general&display_rank=1.
Diane MFS, Jonathan MZ. Dabigatran: Drug information.[cited 2020 June 30]. Available from: https://www.uptodate.com/contents/dabigatran-drug-information?search=dabigatran%20drug%20information&source=panel_search_result&selectedTitle=1~143&usage_type=panel&kp_tab=drug_general&display_rank=1.
Di Minno A, Frigerio B, Spadarella G, Ravani A, Sansaro D, Amato M, et al. Old and new oral anticoagulants: food, herbal medicines and drug interactions. Blood Rev. 2017;31(4):193-203.
Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, et al. The 2018 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39:1330-93.
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-52.
Mazzolai L, Aboyans V, Ageno W, Agnelli G, Alatri A, Bauersachs R, et al. Diagnosis and management of acute deep vein thrombosis: a joint consensus document from the European Society of Cardiology working groups of aorta and peripheral vascular diseases and pulmonary circulation and right ventricular function. Eur Heart J. 2017;39(47):4208-18.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): the task force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Heart J. 2019;41(4):543-603.
Elsebaie MAT, van Es N, Langston A, Büller HR, Gaddh M. Direct oral anticoagulants in patients with venous thromboembolism and thrombophilia: a systematic review and meta-analysis. J Thromb Haemost. 2019;17(4):645-56.
Elshafei MN, Mohamed MFH, El-Bardissy A, Ahmed MB, Abdallah I, Elewa H, et al. Comparative effectiveness and safety of direct oral anticoagulants compared to warfarin in morbidly obese patients with acute venous thromboembolism: systematic review and a meta-analysis. J Thromb Thrombolysis. 2021;51(2):388-96.
Sterne JA, Bodalia PN, Bryden PA, Davies PA, López-López JA, Okoli GN, et al. Oral anticoagulants for primary prevention, treatment and secondary prevention of venous thromboembolic disease, and for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis and cost-effectiveness analysis. Health Technol Assess. 2017;21(9):1-386.
สำนักคณะกรรมการอาหารและยา. ตรวจสอบการอนุญาต. [สืบค้นเมื่อ 20 กรกฎาคม 2563]. สืบค้นจาก: http://porta.fda.moph.go.th/FDA_SEARCH_ALL/MAIN/SEARCH_CENTER_MAIN.aspx.
คณะกรรมการพัฒนาระบบยาแห่งชาติ. ประกาศคณะกรรม–การพัฒนาระบบยาแห่งชาติ เรื่อง บัญชียาหลักแห่งชาติ พ.ศ. ๒๕๖๒. [สืบค้นเมื่อ 11 กรกฎาคม 2563]. สืบค้นจาก: http://dmsic.moph.go.th/index/dataservice/97/0.
Downloads
Published
How to Cite
Issue
Section
License
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมโรงพยาบาลทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของสมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสาร (สมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย)) อย่างเป็นลายลักษณ์อักษร
สมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับสมาคมเภสัชกรรมโรงพยาบาล (ประเทศไทย) และบุคลากรในสมาคมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ


.png)

