The Effects of a Mobile Application–Based Video Education and Monitoring Program on Medication Adherence in Tuberculosis Patient
Keywords:
Educational Program, Medication Monitoring, Mobile Application Video, Medication AdherenceAbstract
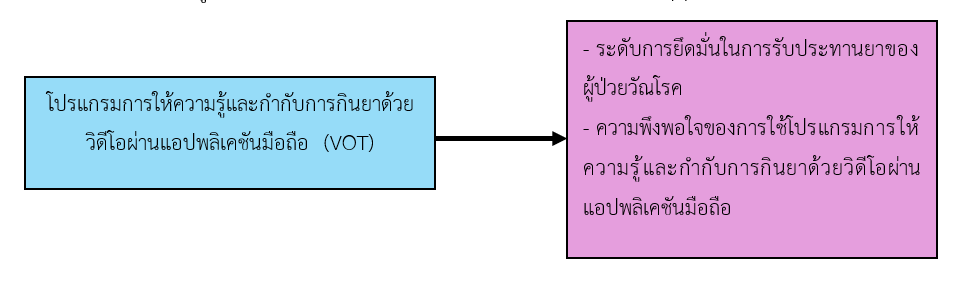
This study aimed to examine the effects of an educational and video-based medication adherence monitoring program delivered via a mobile application on medication adherence among tuberculosis patients, as well as their satisfaction with the program. The sample consisted of 25 newly diagnosed male and female pulmonary tuberculosis patients registered for treatment at the tuberculosis clinic in Trang Province. Participants received the educational program and treatment under directly observed therapy (DOT) using a mobile application, which was adapted from the telehealth principles. The intervention lasted for four weeks. Data were collected using a mobile application–based questionnaire and analyzed with paired t-test statistics.
The findings revealed that tuberculosis patients’ medication adherence scores at Week 4 increased compared to those at Week 1. The mean adherence score in Week 1 was at a moderate level (M= 7.18, SD= 0.60), whereas the mean score in Week 4 reached a high level (M= 8.00, SD= 0.46). The difference between the pre- and post-program mean scores was statistically significant at the 0.05 level. In addition, participants reported a high level of overall satisfaction with the video-based medication adherence monitoring program via mobile application (M= 3.45, SD= 0.52). The highest-rated item was that the program was practical and applicable (M= 3.64, SD= 0.51).
This study demonstrated that a 4-week mobile application–based video education and medication adherence monitoring program improved medication adherence among tuberculosis patients. It is recommended that the program be implemented with feedback mechanisms and two-way communication to further promote continuous medication adherence in tuberculosis patients.
References
Center for Disease Control and Prevention. (2021). Core curriculum on tuberculosis: What the Clinician Should Know. Georgia, USA: CDC.
Chantana, N., Maneesriwongul, W., & Putawatana, P. (2019). Factors related to adherence to multi-drug resistant tuberculosis treatment. Ramathibodi Nursing Journal, 25(3), 298-307. (in Thai)
Choowong, J., Tillgren, P., & Söderbäck, M. (2018). Directly observed therapy providers’ practices when promoting tuberculosis treatment in a local Thai community. Journal of Public Health in Development Countries, 4(1), 458-466.
Cohen, J. (1977). Statistical power analysis for the behavioral sciences (Rev. ed.). Lawrence Erlbaum Associates, Inc.
Division of Tuberculosis. (2021). National tuberculosis control programme guideline, Thailand 2021. Bangkok: Division of Tuberculosis. (in Thai)
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175-191.
Ingkamanee, N., Kusuma Na Ayuthya, S., Puwarawuttipanit, W., & Peerapatdit, T. (2011). Effectiveness of promoting a problem-solving ability program on medication adherence in patients with type 2 diabetic. Journal of Nursing Science, 29(2), 56-64. (in Thai)
Kongkasem, P., Theeranut, A., & Srichan, C. (2020). Effects of innovation “KKU-TB-BOX” on adherence to tuberculosis treatment process. Journal of Nursing Science & Health, 43(2), 1-12. (in Thai)
Kumwichar, P., Chongsuvivatwong, V., & Prappre, T. (2021). Development of a video-observed therapy system to improve monitoring of tuberculosis treatment in Thailand: mixed-methods study. JMIR Formative Research, 5(7), e29463. https://doi.org/10.2196/29463.
Morisky, D. E., Ang, A., Krousel-Wood, M. & Ward, H. (2008) Predictive validity of a medication adherence measure for hypertension control. The Journal of Clinical Hypertension, 10, 348-354. http://dx.doi.org/10.1111/j.1751-7176.2008.07572.x
Naing, L., Winn, T., & Rusli, B. N. (2006). Practical issues in calculating the sample size for prevalence studies. Archives of Orofacial Sciences, 1(1), 9-14.
Pathaweesrisutha, P. (2021). Effects of education and treatment using directly observed treatment (DOT) program through line application on anti-tuberculosis medication adherence in patients with pulmonary tuberculosis. Research and Development Health System Journal, 14(2), 301-309. (in Thai)
Rattanasuwan, P. (2018). TB treatment: DOT vs. VOT. Journal of Bamrasnaradura Infectious Diseases Institute, 12(1), 43-47. (in Thai)
Thammakumpee, G. (2019). Pulmonary tuberculosis in the 21th century. (1st ed.). Bangkok: Sahamit Pattana Printing (1992) Company Limited. (in Thai)
Togun, T., Kampmann, B., Stoker, N.G., Lipman, M. (2020). Anticipating the impact of the COVID-19 pandemic on TB patients and TB control programmes. Annals of Clinical Microbiology and Antimicrobials, 19, 21. https://doi.org/10.1186/s12941-020-00363-1
Trang Provincial Public Health Office. (2021). Annual report 2020. Trang: Trang provincial public health office. (in Thai) Wongprakornkul, S. (2020). New era of healthcare through business ecosystem and telehealth. Mahidol R2R e-Journal, 7(2), 1-15.
World Health Organization. (2017). Handbook for the use of digital technologies to support tuberculosis medication adherence. Geneva, Switzerland.
World Health Organization. (2021). Review on palliative care with focus on 18 high tuberculosis priority countries, 2020. Copenhagen: WHO Regional Office for Europe; 2021. Geneva, Switzerland.
World Health Organization. (2021). WHO global lists of high burden countries for tuberculosis (TB), TB/HIV and multidrug/rifampicin-resistant TB (MDR/RR-TB), 2021 - 2025. Geneva, Switzerland.
Zimmer, A. J., Heitkamp, P., Malar, J., Dantas, C., O'Brien, K., Pandita, A., et al. (2021). Facility- based directly observed therapy (DOT) for tuberculosis during COVID-19: A community perspective. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 24, 100248. https://doi.org/10.1016/j.jctube.2021.100248.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Boromarajonani College of Nursing, Nakhon Si Thammarat

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของ วิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับวิทยาลัยพยาบาลบรมราชชนนี นครศรีธรรมราช และบุคคลากรท่านอื่น ๆ ในวิทยาลัยฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว