Clinical Characteristics and Survival of Pemphigoid and Pemphigus Patients in a Thai Population
DOI:
https://doi.org/10.33192/smj.v76i1.248614Keywords:
Autoimmune bullous disease, pemphigoid, pemphigus, survival rate, prognostic factorAbstract
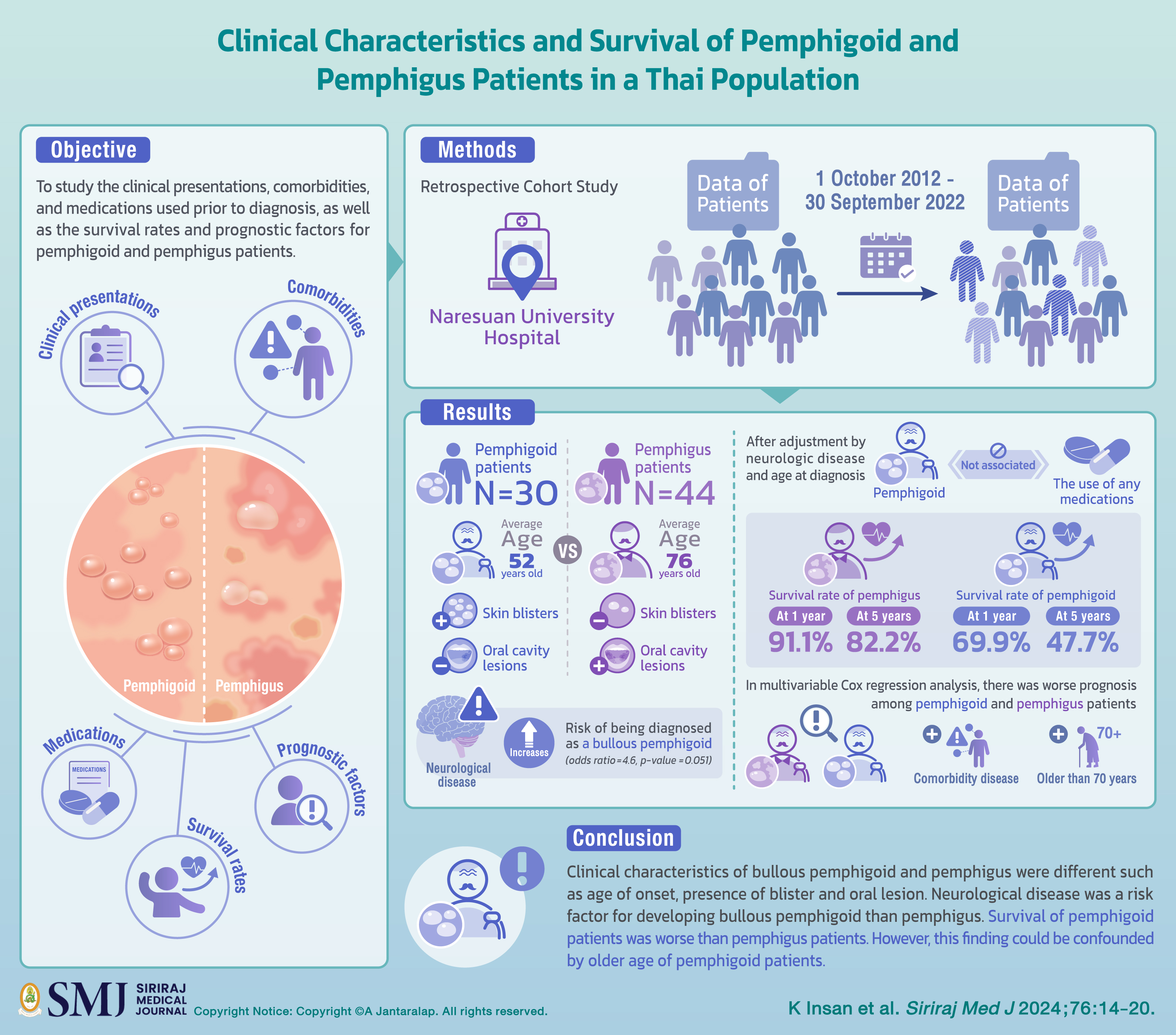
Objective: Pemphigoid and pemphigus are skin diseases with high morbidity and mortality. The research aims to study the clinical presentations, comorbidities, and medications used prior to diagnosis, as well as the survival rates and prognostic factors for pemphigoid and pemphigus patients.
Materials and Methods: The cohort study was conducted on retrospective data of patients who were treated at Naresuan University Hospital between 1 October 2012 and 30 September 2022.
Results: There were 30 pemphigoid patients and 44 pemphigus patients. Pemphigoid patients were on average older than pemphigus patients (76 years vs 52 years), have more skin blisters, and less oral cavity lesions. Neurological disease increases risk of being diagnosed as a bullous pemphigoid (odds ratio=4.6, p-value =0.051). After adjustment by neurologic disease and age at diagnosis, pemphigoid was not significantly associated with the use of any medications. The survival rate of pemphigus was 91.1% at 1 year and 82.2% at 5 years, while the survival rate of pemphigoid was 69.9% at 1 year, and 47.7% at 5 years. In multivariable Cox regression analysis, there was worse prognosis among pemphigoid and pemphigus patients that have comorbidity disease (adjusted HR= 3.13, p-value=0.057) and were older than 70 years (adj HR= 6.93, p-value=0.015).
Conclusion: Clinical characteristics of bullous pemphigoid and pemphigus were different such as age of onset, presence of blister and oral lesion. Neurological disease was a risk factor for developing bullous pemphigoid than pemphigus. Survival of pemphigoid patients was worse than pemphigus patients. However, this finding could be confounded by older age of pemphigoid patients.
References
Chaiyamahapurk S, Warnnissorn P. Prevalence and Pattern of Diseases of The Skin and Subcutaneous Tissue in A Primary Care Area in Thailand. Siriraj Med J [Internet]. 2021 Jun. 1 [cited 2023 Dec. 10];73(6):357-62.
Moro F, Fania L, Sinagra JLM, Salemme A, Di Zenzo G. Bullous Pemphigoid: Trigger and Predisposing Factors. Biomolecules. 2020;10(10):1432.
Borradori L, Van Beek N, Feliciani C, Tedbirt B, Antiga E, Bergman R, et al. Updated S2 K guidelines for the management of bullous pemphigoid initiated by the European Academy of Dermatology and Venereology (EADV). J Eur Acad Dermatol Venereol. 2022;36(10):1689-704.
Heng LC, Phoon YW, Pang SM, Lee HY. Pemphigoid and pemphigus: Comparative analysis of clinical epidemiology, course and outcome in an Asian Academic Medical Centre. Australas J Dermatol. 2021;62(2):e288-90.
Kridin K, Shihade W, Bergman R. Mortality in Patients with Bullous Pemphigoid: A Retrospective Cohort Study, Systematic Review and Meta-analysis. Acta Derm Venereol. 2019;99(1):72-7.
Kulthanan K, Chularojanamontri L, Tuchinda P, Sirikudta W, Pinkaew S. Prevalence and clinical features of Thai patients with bullous pemphigoid. Asian Pac J Allergy Immunol. 2011;29(1):66-72.
Bastuji-Garin S, Joly P, Lemordant P, Sparsa A, Bedane C, Delaporte E, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131(3):637-43.
Langan SM, Groves RW, West J. The relationship between neurological disease and bullous pemphigoid: a population-based case-control study. J Invest Dermatol. 2011;131(3):631-6.
Lai YC, Yew YW, Lambert WC. Bullous pemphigoid and its association with neurological diseases: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2016;30(12):2007-15.
Ujiie H. What’s new in the pathogeneses and triggering factors of bullous pemphigoid. J Dermatol. 2023;50(2):140-9.
Liu SD, Chen WT, Chi CC. Association Between Medication Use and Bullous Pemphigoid: A Systematic Review and Meta-analysis. JAMA Dermatol. 2020;156(8):891-900.
Ghaedi F, Etesami I, Aryanian Z, Kalantari Y, Goodarzi A, Teymourpour A, et al. Drug-induced pemphigus: A systematic review of 170 patients. Int Immunopharmacol. 2021;92:107299.
Palleria C, Bennardo L, Dastoli S, Iannone LF, Silvestri M, Manti A, et al. Angiotensin-converting-enzyme inhibitors and angiotensin II receptor blockers induced pemphigus: A case series and literature review. Dermatol Ther. 2019;32(1):e12748.
Joly P, Horvath B, Patsatsi Α, Uzun S, Bech R, Beissert S, et al. Updated S2K guidelines on the management of pemphigus vulgaris and foliaceus initiated by the european academy of dermatology and venereology (EADV). J Eur Acad Dermatol Venereol. 2020;34(9):1900-13.
Cortés B, Khelifa E, Clivaz L, Cazzaniga S, Saurat JH, Naldi L, et al. Mortality rate in bullous pemphigoid: a retrospective monocentric cohort study. Dermatology. 2012;225(4):320-5.
Amonchaisakda N, Aiempanakit K. Clinical characteristics, mortality, and prognostic factors for bullous pemphigoid in a Thai population. Medicine (Baltimore). 2020;99(43):e22850.
Titou H, Hjira N. Mortality and prognostic factors of Bullous Pemphigoid in a Moroccan population. Australas J Dermatol. 2022;63(3):328-34.
Jelti L, Cordel N, Gillibert A, Lacour JP, Uthurriague C, Doutre MS, et al. Incidence and Mortality of Pemphigus in France. J Invest Dermatol. 2019;139(2):469-73.
Joly P, Benichou J, Lok C, Hellot MF, Saiag P, Tancrede-Bohin E, et al. Prediction of survival for patients with bullous pemphigoid: a prospective study. Arch Dermatol. 2005;141(6):691-8.
Singh S, Kirtschig G, Anchan VN, Chi CC, Taghipour K, Boyle RJ, et al. Interventions for bullous pemphigoid. Cochrane Database Syst Rev. 2023;8(8):CD002292.
Oren-Shabtai M, Mimouni D, Nosrati A, Atzmony L, Kaplan B, Barzilai A, et al. Biological treatment for bullous pemphigoid. Front Immunol. 2023;14:1157250.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














