Antimicrobial Resistance Patterns Amid Community-Acquired Uropathogens in Outpatient Settings of a Tertiary Care Hospital in Thailand
DOI:
https://doi.org/10.33192/Smj.2021.65Keywords:
Community, urinary tract infection, antibiotic resistanceAbstract
Objective: To document the distribution of antimicrobial resistance patterns of community-acquired uropathogens.
Materials and Methods: Outpatient microbiology data of urine culture results in Songklanagarind Hospital between January to December 2019 were reviewed.
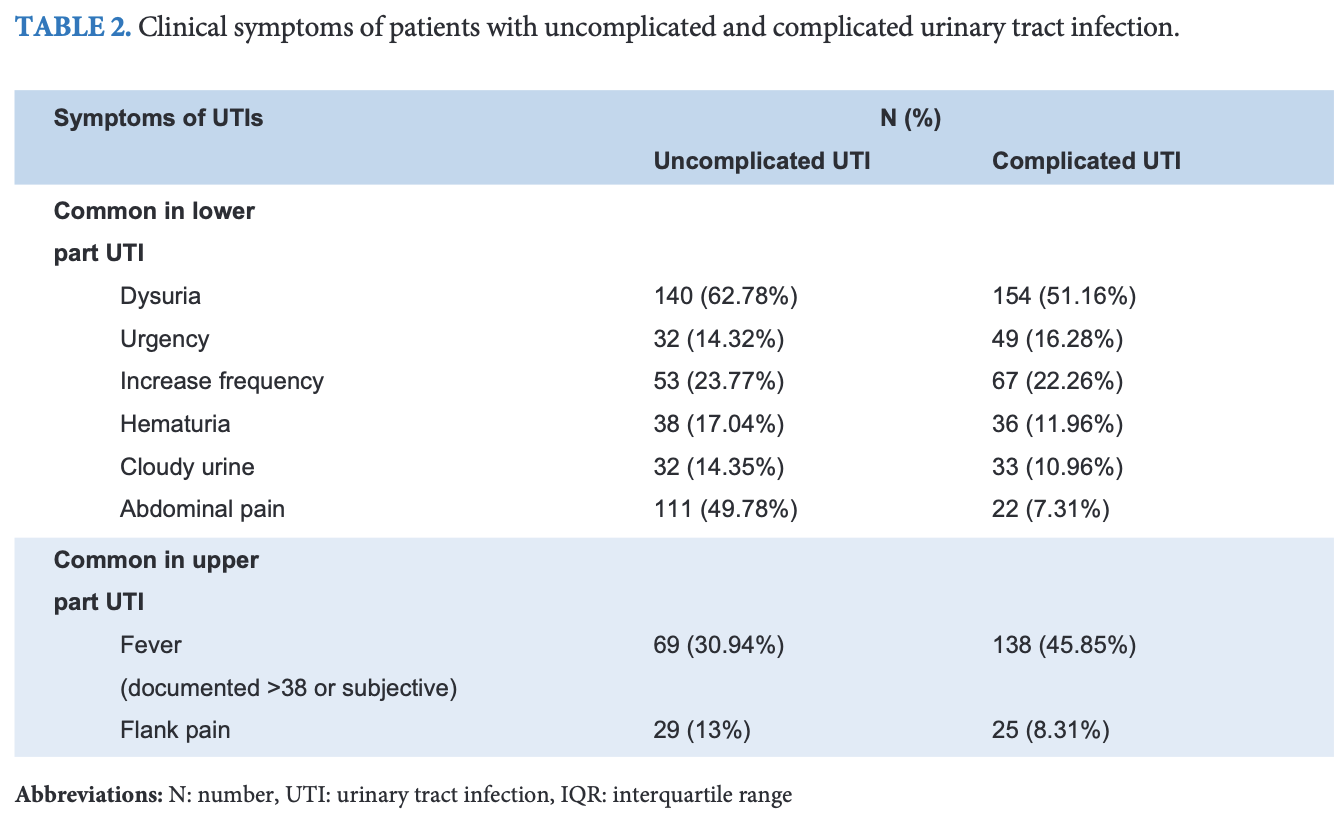
Results: This study included 649 episodes of positive urine cultures in 598 patients, in which 80.7% were symptomatic cases. The elderly (median 63 ± IQR 26 years) showed high prevalence of urinary tract infections in this study, for which nearly 80% of all samples were female. The three most common uropathogens identified were: Escherichia coli (E. coli) (69.6%), Klebsiella pneumoniae (9.5%) and Staphylococcus saprophyticus (4.9%). E. coli were highly resistant to ciprofloxacin (49.0 %), cotrimoxazole (41.2%) and ceftriaxone (20.6%), but had a low level of resistance to fosfomycin (0%), and amikacin (0.4%).
Conclusion: The antimicrobial resistance pattern of E. coli was high for commonly antimicrobial agents used in outpatients; especially quinolone, cotrimoxazole and cephalosporin. However, due to low resistance levels, fosfomycin and amikacin could be considered as effective treatment options for community acquired UTIs in our study.
References
2. Ong DSY, Kuyvenhoven MM, van Dijk L, Verheij TJM. Antibiotics for respiratory, ear and urinary tract disorders and consistency among GPs. J Antimicrob Chemother 2008; 62(3): 587-92.
3. Bonine NG, Berger A, Altincatal A, Wang R, Bhagnani T, Gillard P, et al. Impact of Delayed Appropriate Antibiotic Therapy on Patient Outcomes by Antibiotic Resistance Status From Serious Gram-negative Bacterial Infections. Am J Med Sci 2019; 357(2): 103-10.
4. Sangsuwan T, Jamulitrat S. Antimicrobial resistance among urinary tract infection pathogens in the Outpatient Department of Songklanagarind Hospital in the year 2008 [Dissertation]. Songkhla: Prince of Songkla University; 2010.
5. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 2002; 137(10): 791-7.
6. Bonkat, G, Pickard, R, Bartoletti, R. EAU guidelines on urogenital infections. Leiden,
The Netherlands: European Association of Urology,2018. [cited 2020 Feb 7]. Available
from: http://uroweb.org/guideline/urological-infections/
7. Ghafourian S, Sadeghifard N, Soheili S, Sekawi Z. Extended Spectrum Beta-lactamases: Definition, Classification and Epidemiology. Curr Issues Mol Biol. 2015;17:11-21.
8. CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 29th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2019.
9. Ho HJ, Tan MX, Chen MI, Tan TY, Koo SH, Koong AYL, et al. Interaction between Antibiotic Resistance, Resistance Genes, and Treatment Response for Urinary Tract Infections in Primary Care. J Clin Microbiol [Internet]. 2019 [cited 2020 Feb 7];57(9). Available from: https://jcm.asm.org/content/57/9/e00143-19
10. Dash M, Padhi S, Mohanty I, Panda P, Parida B. Antimicrobial resistance in pathogens causing urinary tract infections in a rural community of Odisha, India. J Family Community Med 2013; 20(1): 20-6.
11. Rafalskiy V, Pushkar D, Yakovlev S, Epstein O, Putilovskiy M, Tarasov S, et al. Distribution and antibiotic resistance profile of key Gram-negative bacteria that cause community-onset urinary tract infections in the Russian Federation: RESOURCE multicentre surveillance 2017 study. J Glob Antimicrob Resist 2020; 21: 188-94.
12. Lob SH, Nicolle LE, Hoban DJ, Kazmierczak KM, Badal RE, Sahm DF. Susceptibility patterns and ESBL rates of Escherichia coli from urinary tract infections in Canada and the United States, SMART 2010–2014. Diagn Microbiol Infect Dis 2016;0 85(4): 459-65.
13. Kim YJ, Lee J-M, Cho J, Lee J. Change in the Annual Antibiotic Susceptibility of Escherichia coli in Community-Onset Urinary Tract Infection between 2008 and 2017 in a Tertiary Care Hospital in Korea. J Korean Med Sci [Internet] 2019 [cited 2021 Jan 23];34(34). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6717241/
14. Wong CKM, Kung K, Au-Doung PLW, Ip M, Lee N, Fung A, et al. Antibiotic resistance rates and physician antibiotic prescription patterns of uncomplicated urinary tract infections in southern Chinese primary care. PLoS ONE 2017; 12(5): e0177266.
15. Arslan H, Azap O, Ergonul O, Ergin F, Aydın K, Bakır M, et al. Risk factors for ciprofloxacin resistance among Escherichia coli strains isolated from community-acquired urinary tract infections in Turkey. J Antimicrob Chemother 2005 ; 56: 914–8.
16. Klingeberg A, Noll I, Willrich N, Feig M, Emrich D, Zill E, et al. Antibiotic-Resistant E. coli in Uncomplicated Community-Acquired Urinary Tract Infection. Dtsch Arztebl Int 2018; 115: 494-500.
17. NARST: National Antimicrobial Resistance Surveillance Center, THAILAND [Internet]. [cited 2021 Feb 2]. Available from:http://narst.dmsc.moph.go.th/news001.html
18. Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011; 52(5): e103-20.
19. Craig WA. Optimizing aminoglycoside use. Crit Care Clin 2011; 27: 107-21.
20. Sung YC, Su MC, Sun HP, Dong GL, Jung HC, Jin HY. Amiin therapy for urinary tract infections caused by extended-spectrum β-lactamase-producing Escherichia coli. Korean J Intern Med 2016; 31: 156-61.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














