Randomized Controlled Trial Evaluating the Efficacy and Cost Effectiveness of a Ready-to-Use Applicator Containing Iodine Povacrylex and Isopropyl Alcohol Compared with Conventional Skin Scrubbing and Painting in Patients Undergoing Colorectal Surgery
DOI:
https://doi.org/10.33192/Smj.2021.74Keywords:
Surgical site infection, Skin preparation, Colorectal surgery, A ready-to-use applicator containing iodine povacrylex and isopropyl alcohol (IPIA)Abstract
Objective: The aim of this study was to evaluate the efficacy and cost-effectiveness of a ready-to-use applicator containing iodine povacrylex and isopropyl alcohol (IPIA) for the prevention of surgical site infection (SSI) following intra-abdominal surgery.
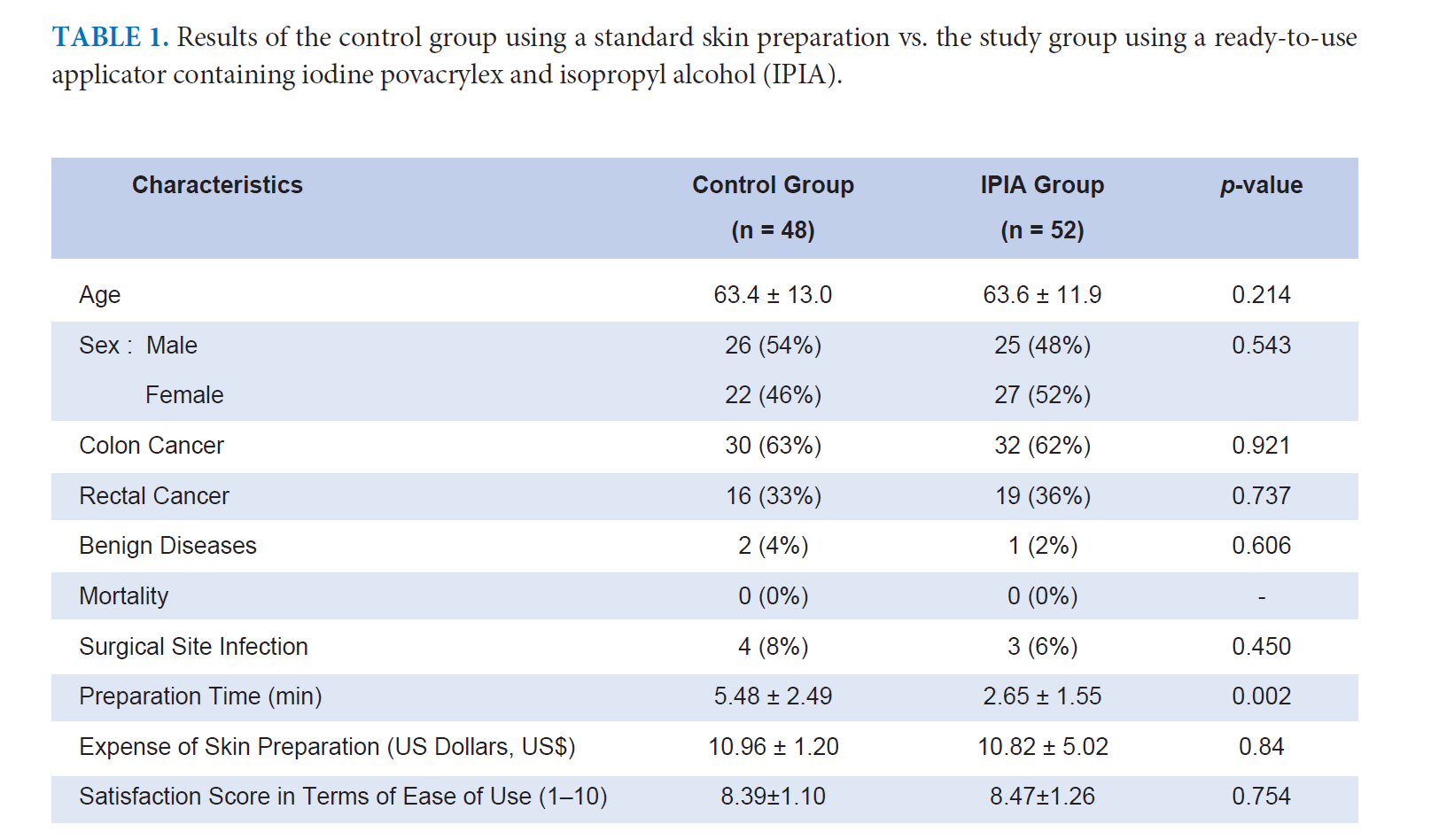
Materials and Methods: The IPIA was randomly used in patients who underwent colorectal surgical procedures. The control group for comparison was a group of patients who underwent colorectal surgical procedures using conventional skin scrubbing and painting with antiseptic solutions without IPIA. In total, 100 patients were included in the study, randomized into 2 groups: one was applied IPIA and another group a conventional skin preparation. The outcome measurements included ease-of-use as assessed by a questionnaire, preparation time comparison, estimated skin preparation expense, adverse reactions, and rate of SSI. All the patients were visited daily up to 7 days postoperation or until discharge, and then 14 and 30 days postoperatively for monitoring the occurrence of SSI.
Results: Of the 100 patients undergoing elective intra-abdominal surgery enrolled in the study, 51 were males and 49 females, with the mean age of 63.5 ± 11.3 years. The majority of the patients had undergone colorectal cancer colectomies or rectal resections. There was no mortality. Seven patients (7%) had postoperative SSI (4 patients in the control group and 3 patients in the IPIA group, 4% vs. 3%, p = 0.45). The bacterial cultures revealed Gram negative-bacilli in all of the patients with SSI. The preparation time for the skin preparation was 5.48 ± 2.49 min in the control group and 2.65 ± 1.55 min in the IPIA group (p = 0.002), without statistical significance of expenses.
Conclusion: IPIA was demonstrated to be as safe and effective as conventional antiseptic solutions as a skin preparation to prevent SSI following colorectal surgery. With good ease of use, IPIA proved more convenient than a scrubbing preparation as well as offered better cost effectiveness by significantly reducing the time and cost of the skin preparation.
References
Auerbach AD. Prevention of surgical site infections. In: Shojania KG, Duncan BW,McDonald KM, Wachter RM, eds. Making health care safer: a critical analysis of patient safety practices. Evidence report/technology assessment no. 43. AHRQ publication no. 01-E058. Rockville, MD: Agency for Healthcare Research and Quality, 20 July 2001:221-44.
Perencevich EN, Sands KE, Cosgrove SE, Guadagnoli E, Meara E, Platt R. Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis 2003; 9: 196-203.
Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis 2004; 38: 1707-15.
Jacobson CS, Osmon DR, Hanssen A, et al: Preventions of Wound Contamination Using DuraPrep™ Solution Plus Ioban™ 2 Drapes. Clinical Orthopaedics and Related Research Number 439 October 2005.p.32-37.
Hemani ML, Lepor H. Skin Preparation for the Prevention of Surgical Site Infection: Which Agent Is Best? Rev Urol. 2009; 11(4):190-5.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC Definitions of nosocomial surgical site infections, 1992: A modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 1992;13 606-8.
Lohsiriwat V, Lohsiriwat D. Antibiotic prophylaxis and incisional surgical site infection following colorectal cancer surgery: an analysis of 330 cases. J Med Assoc Thai 2009;92:12-6.
Berrios-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 2017;152:784-91.
Kashimura N, Kusachi S, Konishi T, Shimizu J, Kusunoki M, Oka M, Wakatsuki T, Sumiyama Y. Impact of surgical site infection after colorectal surgery on hospital stay and medical expenditure in Japan. Surg Today. 2012;42(7):639-45. doi: 10.1007/s00595-012-0126-8. PMID: 22286573.
Turner MC, Migaly J. Surgical Site Infection: The Clinical and Economic Impact. Clin Colon Rectal Surg. 2019;32(3):157- 65. doi: 10.1055/s-0038-1677002. Epub 2019 Apr 2. PMID: 31061644; PMCID: PMC6494617.
Gomila A, Badia JM, Carratalà J, Serra-Aracil X, Shaw E, Diaz-Brito V, Castro A, Espejo E, Nicolás C, Piriz M, Brugués M, Obradors J, Lérida A, Cuquet J, Limón E, Gudiol F, Pujol M; VINCat Colon Surgery Group. Current outcomes and predictors of treatment failure in patients with surgical site infection after elective colorectal surgery. A multicentre prospective cohort study. J Infect. 2017;74(6):555-63. doi: 10.1016/j.jinf.2017.03.002. Epub 2017 Mar 16. PMID: 28315721.
Lohsiriwat V, Chinswangwatanakul V, Lohsiriwat D, Rongrungruang Y, Malathum K, Ratanachai P, et al. Guidelines for the Prevention of Surgical Site Infection: The Surgical Infection Society of Thailand Recommendations (Executive Summary). J Med Assoc Thai 2020;103:99-105.
Tang R, Chen HH, Wang YL, Changchien CR, Chen JS, Hsu KC, Chiang JM, Wang JY. Risk factors for surgical site infection after elective resection of the colon and rectum: a singlecenter prospective study of 2,809 consecutive patients. Ann Surg. 2001;234(2):181-9. doi: 10.1097/00000658-200108000-00007. PMID: 11505063; PMCID: PMC1422004.
Hennessey DB, Burke JP, Ni-Dhonochu T, Shields C, Winter DC, Mealy K. Risk factors for surgical site infection following colorectal resection: a multi-institutional study. Int J Colorectal Dis. 2016;31(2):267-71. doi: 10.1007/s00384-015-2413-5. Epub 2015 Oct 28. PMID: 26507963.
Anjum N, Ren J, Wang G, Li G, Wu X, Dong H, Wu Q, Li J. A Randomized Control Trial of Preoperative Oral Antibiotics Tanjak et al. https://he02.tci-thaijo.org/index.php/sirirajmedj/index Volume 73, No.9: 2021 Siriraj Medical Journal 567 Original Article SMJ as Adjunct Therapy to Systemic Antibiotics for Preventing Surgical
Site Infection in Clean Contaminated, Contaminated, and Dirty Type of Colorectal Surgeries. Dis Colon Rectum. 2017;60(12):1291-1298. doi: 10.1097/DCR.0000000000000927. PMID: 29112565.
Leaper DJ, Holy CE, Spencer M, Chitnis A, Hogan A, Wright GWJ, Po-Han Chen B, Edmiston CE Jr. Assessment of the Risk and Economic Burden of Surgical Site Infection Following Colorectal Surgery Using a US Longitudinal Database: Is There a Role for Innovative Antimicrobial Wound Closure Technology to Reduce the Risk of Infection? Dis Colon Rectum. 2020;63(12):1628-38. doi: 10.1097/DCR.0000000000001799. PMID: 33109910;
PMCID: PMC7774813.
Lohsiriwat V, Jaturanon, P. Effect of Intraoperative Hypothermia on Surgical Outcomes after Colorectal Surgery within an Enhanced Recovery after Surgery Pathway. Siriraj Medical Journal 2019;71(1):52-58. https://doi.org/10.33192/Smj.2019.09
Nampoolsuksan C, Parakonthun T, Tawantanakorn T, Mora A, Swangsri J, Akaraviputh T, Methasate A, Yiengpruksawan A, Chinswangwatanakul V. (2020). Short-term Postoperative Outcomes Before and After the Establishment of the Siriraj Upper Gastrointestinal Cancer Center: A Propensity Score Matched Analysis. Siriraj Medical Journal 2020;72(4):215-320. https://doi.org/10.33192/Smj.2020.43.
Downloads
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














