Study of Congenital Malformation in a Tertiary Care Teaching Hospital
DOI:
https://doi.org/10.33192/Smj.2021.79Keywords:
Congenital anomalies, Genitourinary system, Gastrointestinal system, HypospadiasisAbstract
Objective: Congenital anomaly is one of the most important causes & being the 5th most common cause of
neonatal mortality & morbidity. It may present as a structural or functional abnormality. These defects occur due to defective embryogenesis. Associated factors may be maternal age, maternal TORCH infection, drugs, genetic factors. Antenatal USG reduces the incidence.
Materials and Methods: A cross-sectional study was done in the Pediatric department over 1 year. Diagnosis of
all congenital anomalies was done by the concerned pediatrician& pediatric surgeon. Data was collected in the
specified format.
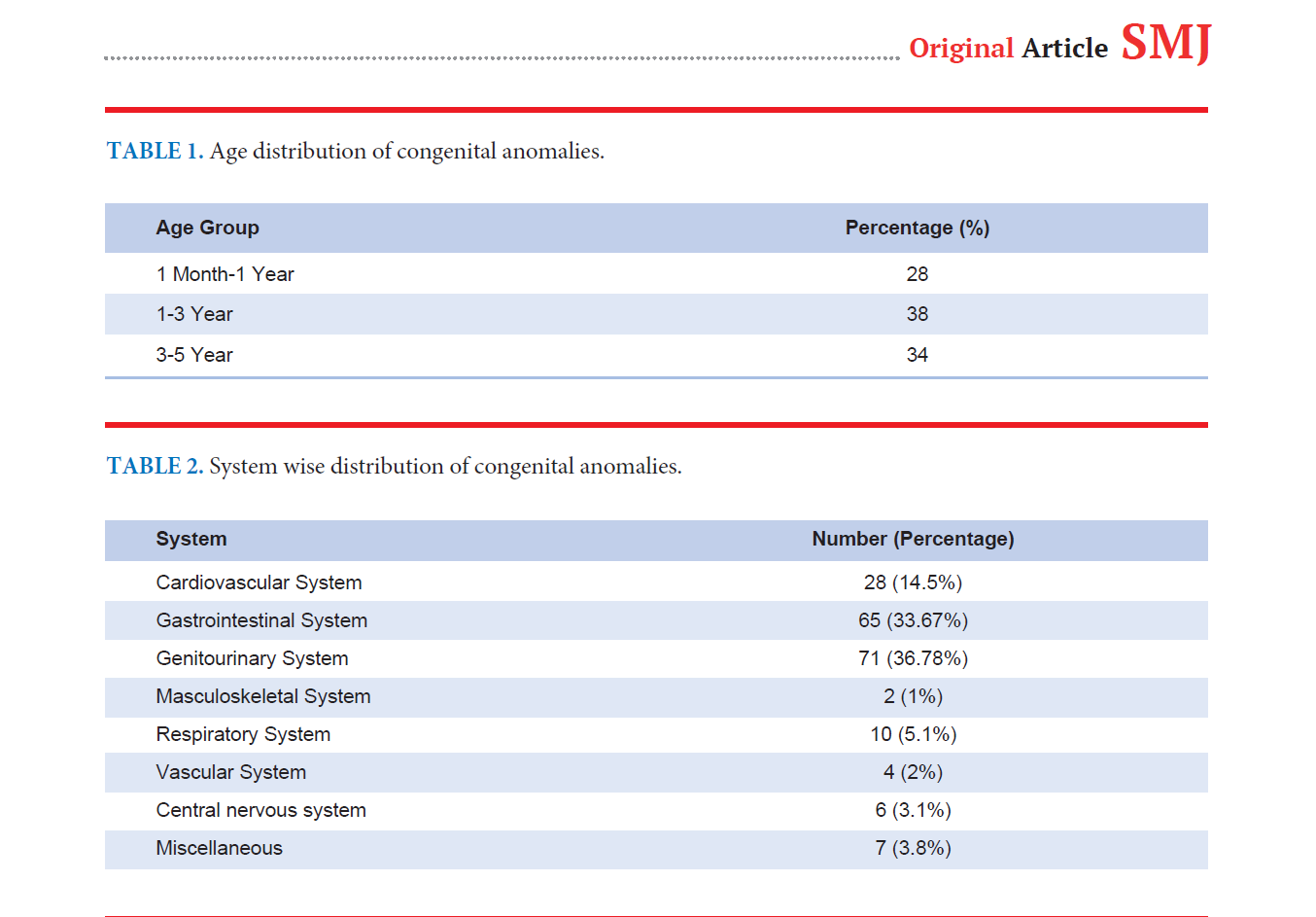
Results: A total of 10205 cases of age group 1 month to 5 years presented to the paediatric OPD, out of which 193
children were diagnosed as congenital anomalies in 1 year. Males were found to be affected the most. The most
common system involved was found to be the genitourinary system (36.78%). The second most common system involved was the gastrointestinal system (33.67%). The least common system involved was the musculoskeletal system.
Conclusion: Congenital anomalies are a major cause of neonatal & infantile mortality & morbidity. Routine
screening with a level II targeted scan for all the pregnant mothers should be mandatory. Adequate nutrition, parental education & Rubella vaccination of the mother can decrease the prevalence of congenital anomalies to some extend.
References
Kar A. Birth Defects in India: Magnitude, Public Health Impact and Prevention. Journal of Krishna Institute of Medical Sciences University 2014;3:7-16
Taksande A, Vilhekar K, Chaturvedi P, Jain M. Congenital malformations at birth in Central India: A rural medical college hospital based data. Indian Journal of Human Genetics 2010;16:159
Pandala P, Kotha R, Singh H, Nirmala C. Pattern of congenital anomalies in neonates at tertiary care centre in Hyderabad, India: a hospital based prospective observational study. International Journal of Contemporary Pediatrics 2018;6: 63-67
Stark RB. Congenital anomalies. Rev Surg 1965;22:305-10.
Agarwal SS, Singh U, Singh PS, Singh SS, Das V, Sharma A et al. Prevalence & spectrum of congenital malformations in a prospective study at a teaching hospital. Indian Journal of Medical Research 2011;94: 413-419.
Praneshwari RK, Singh NN, Devi AT, Priya J, Singh LR. Congenital anomalies in a tertiary care hospital in North East region, India. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 2019;8:3295-3299
Devi KR, Devi RKP, Priya J, Sanaton A, Singh LR, Murray L. A study of congenital anomalies in a tertiary care hospital in North East region, India. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 2018; 7: 2899-2903.
Vinodh SL, Balakrishnan D, Brahmanandan M. Role of Ultrasound as a Diagnostic Modality in Detecting Congenital Anomalies. J Med Sci Clin Res 2017;05(1):7157–60.
Sarkar S, Patra C, Dasgupta MK, Nayek K, Karmakar PR. Prevalence of Congenital Anomalies in Neonates and Associated Risk Factors in a Tertiary Care Hospital in Eastern India. Journal of Clinical Neonatology 2013;2:131-134
Pabbati J, Subramanian P, Raj C, Sadhana N, Rao R. Study on incidence of congenital anomalies in a rural teaching hospital, Telangana, India. International Journal of Contemporary Pediatrics 2016;3:887-890.
Swain S, Agrawal A, Bhatia BD. Congenital malformations at birth. Indian Pediatr 1994;31:1187-91.
Devi KR, Devi RK, Priya J, Sanaton A, Singh LR, Murray L. A study of congenital anomalies in a tertiary care hospital in North East region, India. International journal of reproduction, contraception, obstetrics and gynecology 2018;7:2899.
Thaddanee R, Patel HS, Thakor N. A study on incidence of congenital anomalies in newborns and their association with maternal factors: a prospective study. International Journal of Contemporary Pediatrics 2016; 3:579-582
Dingemann C, Sonne M, Ure B, Bohnhorst B, von Kaisenberg C, Pirr S. Impact of maternal education on the outcome of newborns requiring surgery for congenital malformations. PLoS ONE 2019;14: e0214967.
Downloads
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














