Effects of Physical Exercise Program on Physical Mobility of Patients with Cranial Surgery
DOI:
https://doi.org/10.33192/Smj.2021.89Keywords:
physical exercise, physical mobility, cranial surgeryAbstract
Objective: This research aimed to study the effects of a physical exercise program on physical mobility in cranial surgery patients.
Materials and Methods: The researcher used a quasi-experimental method of surveying 58 patients who had cranial surgery at Siriraj Hospital. The research group was divided into two groups: an experimental group (28 patients) participating in a physical exercise program of patients after cranial surgery, and a control group (30 patients) receiving routine nursing care only. The evaluation of the patients’ physical mobility was performed three days after the surgery.
Results: Most patients in the research group had an intracranial tumor (86.2%). One day after the surgery, the
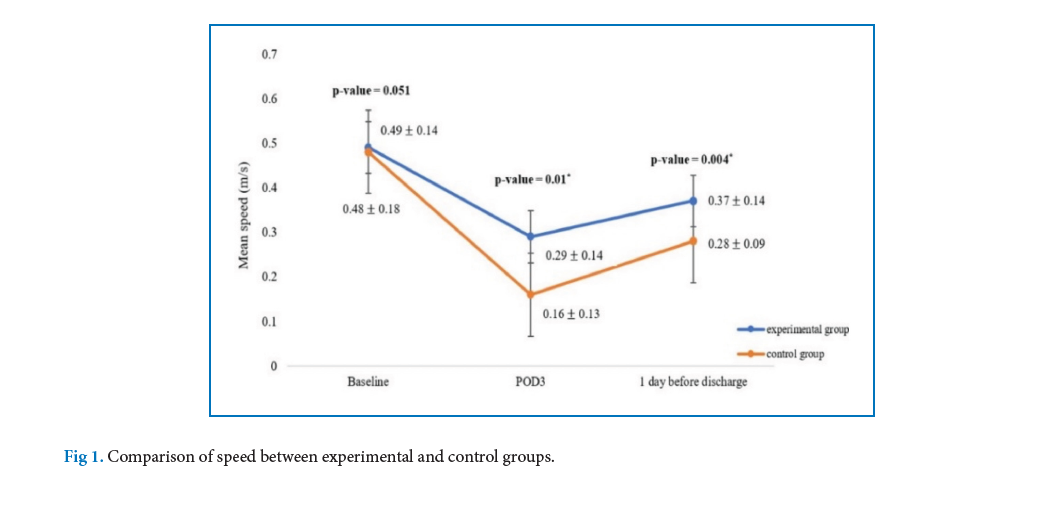
experimental group had minor pain at the wound site while the control group had moderate pain. Both groups felt discomfort (64.2%) or had muscle stiffness in the neck and shoulder areas (63.3%). Three days after the surgery, at the end of the program, the body movement function of both groups was reduced compared with the preoperative data. However, the experimental group showed better body movement function scores than the control one as the scores of the former were reduced less than those of the latter at p < 0.05.
Conclusion: Nurses who provide health care services to patients after cranial surgery should apply the physical
exercise program to promote the recovery of the patients’ physical mobility.
References
Foust. (2018). The experience of post-craniotomy pain among person with brain tumors (dissertation). Bloomington: Indiana University; 2018.
Hemmings G. Neurosurgery after cranial surgery information for patients. (internet). Oxford: Oxford University Hospital NHS Trust; 2018 (cited 2019 Aug 18). Available from https://www.ouh.nhs.uk/patient-guide/leaflets/files/11585Pcranial.pdf
Khan F, Amatya B, Drummond K, Galea MP. Effectiveness of integrated multidisciplinary rehabilitation in primary brain cancer survivors in an Australian community cohort: a controlled clinical trial. J Rehabil Med 2014;46(8):754-60.
Pace A, Villani V, Parisi C, Di Felice S, Lamaro M, Falcicchio C, et al. Rehabilitation pathways in adult brain tumor patients in the first 12 months of disease. A retrospective analysis of services utilization in 719 patients. Support Care Cancer 2016;24(11):4801-6.
Nader R, Gragnaniello C, Berta SC, Sabbagh AJ, Levy ML. Neurosurgery tricks of the trade. New York: Thieme medical publishers; 2014.
Meng L, Berger MS, Gelb AW. The potential benefits of awake craniotomy for brain tumor resection: an anesthesiologist's perspective. J Neurosurg Anesthesiol 2015;27(4):310-7.
Boonprakob Y, Phadungkit S, Nongharnpitak S, Srijessadarak T, Supasatean W, Nakhengrit C. Trigger point: curable or palliative symptoms. J Assoc Med Sci 2016;49(1):155-66.
Sriwicha W. Myofascial pain syndrome. Hua Hin Sook Jai Klai Kangwon Journal 2016;1(1):10-28.
Minerbi A, Vulfsons S. Challenging the Cinderella Hypothesis: a new model for the role of the motor unit recruitment pattern in the pathogenesis of myofascial pain syndrome in postural muscles. Rambam Maimonides Med J 2018;9(3):e0021.
Flexman AM, Ng JL, Gelb AW. Acute and chronic pain following craniotomy. Curr Opin Anaesthesiol 2010;23(5):551-7.
Pavlin DJ, Chen C, Penaloza DA, Polissar NL, Buckley FP. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg 2002;95(3).
Wang Y, Liu B, Zhao T, Zhao B, Yu D, Jiang X, et al. Safety and efficacy of a novel neurosurgical enhanced recovery after surgery protocol for elective craniotomy:a prospective randomized controlled trial. J Neurosurg 2018:1-12.
Janda M, Steginga S, Dunn J, Langbecker D, Walker D, Eakin E. Unmet supportive care needs and interest in services among patients with a brain tumour and their carers. Patient Educ Couns. 2008;71(2):251-8.
Giordana MT, Clara E. Functional rehabilitation and brain tumour patients. A review of outcome. Neurol Sci 2006;27(4):240-4.
Wattradul D. Cardiac rehabilitation: transition care from hospital to home. Thai Journal of Cardio-Thoracic Nursing 2015;26(1):89-103.
Hickey JV. The Clinical practice of neurological and neurosurgical nursing. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2019.
Liu B, Liu S, Wang Y, Lu D, Chen L, Zheng T, et al. Impact of neurosurgical enhanced recovery after surgery (ERAS) program on health-related quality of life in glioma patients: a secondary analysis of a randomized controlled trial. J Neurooncol 2020;148(3):555-67.
Meleis, A.I. Transitions theory: The use of a middle-range and situation-specific theory in the research and care of individuals, families and communities. New York: Springer; 2010.
Im, Eun-Ok. Situation-specific theories from the middle-range transitions theory. ANS Adv Nurs Sci 2014;37(1):19 – 31.
Lu D, Wang Y, Zhao T, Liu B, Ye L, Zhao L, et al. Successful implementation of an Enhanced Recovery After Surgery (ERAS) protocol reduces nausea and vomiting after infratentorial craniotomy for tumour resection: a randomized controlled trial. BMC Neurol 2020;20(1):1-11.
Gemmell H, Miller P, Nordstrom H. Immediate effect of ischaemic compression and trigger point pressure release on neck pain and upper trapezius trigger points:a randomised controlled trial. Clin Chiropr 2008;11(1):30-6.
Taspinar F, Aslan UB, Sabir N, Cavlak U. Implementation of matrix rhythm therapy and conventional massage in young females and comparison of their acute effects on circulation. J Altern Complement Med 2013;19(10):826-32.
Andersson P, Franzén E. Effects of weight-shift training on walking ability, ambulation, and weight distribution in individuals with chronic stroke: a pilot study. Top Stroke Rehabil 2015;22(6):437-43.
Liljehult MM, Buus L, Liljehult J, Rasmussen BK. Walking ability in patients with glioblastoma: prognostic value of the Berg Balance Scale and the 10 meter walk test. J Neurooncol 2017;135(2):335-42.
Noinawakul U, Pinyopasakul W, Kimpee S, Puwarawuttipanit W. The effects of a walking exercise program on perceived self-efficacy and functional capacity in stroke patients with hemiparesis. J Nurs Sci 2010;28(4):45-53.
Qu L, Liu B, Zhang H, Sankey EW, Chai W, Wang B, et al. Management of postoperative pain after elective craniotomy: a prospective randomized controlled trial of a neurosurgical Enhanced Recovery After Surgery (ERAS) program. Int J Med Sci. 2020;17(11):1541-9.
Teerateadtakul B. The effect of massage and exercise of neck on the level of the headache in surgical patients with head elevated position. Thai J Nurs Res 1996;46(1):23-32.
Choy NL, Kuys S, Richards M, Isles R. Measurement of functional ability following traumatic brain injury using the Clinical Outcomes Variable Scale: a reliability study. Aust J Physiother 2002;48(1):35-9.
Leelayuwat N. Physiology of exercise. Khon Kaen: Khon Kaen University; 2553.
Fox SW, Lyon D, Farace E. Symptom clusters in patients with high-grade glioma. J Nurs Scholarsh 2007;39(1):61-7.
Treede, Rolf-Detlef. Gain control mechanisms in the nociceptive system. PAIN 2016;157(6):99-1204.
Field T, Diego M, Gonzalez G, Funk CG. Neck arthritis pain is reduced and range of motion is increased by massage therapy. Complement Ther Clin Pract 2014;20(4):219-23.
Flinder LI, Timofeeva OA, Rosseland CM, Wierød L, Huitfeldt HS, Skarpen E. EGF – induced ERK-activation downstream of FAK requires Rac1-NADPH oxidase. J Cell Physiol 2011;226:2267–78.
Braun, Beth M. Introduction to massage therapy. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
Pianbanyat K, Choowattanapakorn T. The effect of nursing process combined with Swedish massage on pain in older persons with lung cancer. Kuakarun Journal of Nursing 2015;22(1):98-112.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














